A Rare Case of Ileocecal Tuberculosis with Pulmonary Embolism and Deep Vein Thrombosis
Tan Jih Huei1, Tan Chor Lip Henry2, Choon Aik Ho3, Yuzaidi Mohamad4
1 Medical Officer, Department of General Surgery, Hospital Sultanah Aminah, Johor Bahru, Johor, Malaysia.
2 Medical Officer, Department of General Surgery, Hospital Sultanah Aminah, Johor Bahru, Johor, Malaysia.
3 General Surgeon, Department of General Surgery, Hospital Sultanah Aminah, Johor Bahru, Johor, Malaysia.
4 General and Trauma Surgeon, Department of General Surgery, Hospital Sultanah Aminah, Johor Bahru, Johor, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tan Jih huei, Medical Officer, Department of General Surgery, Hospital Sultanah Aminah, Jalan Abu Bakar, Masjid Sultan Abu Bakar-80000, Johor Bahru, Johor Darul Takzim, Malaysia.
E-mail: huei_87@hotmail.com
Venous thromboembolism in tuberculosis is not a well recognised entity. It is a less frequently reported complication of severe pulmonary tuberculosis. It is exceedingly rare when it complicates extrapulmonary tuberculosis. Here, we present a case of 22-year-old young female with abdominal tuberculosis complicated with reverse ileocecal intussusception, deep vein thrombosis and pulmonary embolism. An emergency vena cava filter was inserted prior to a limited right hemicolectomy. In this article, we discuss the rare association of venous thromboembolism with ileocecal tuberculosis.
Gastrointestinal tuberculosis, Ileocecal intussusception, Venous thromboembolism
Case Report
A 22-year-old female presented with lower abdominal pain, loose stools, weight loss and right lower limb painful swelling for three months. There was no history of oral contraceptives use. She was cachexic, dehydrated with dry lips and sunken eyeballs. She had tenderness and guarding over right iliac fossa. Right thigh and calf was swollen and tender.
Blood investigations revealed iron deficiency anaemia [Total Iron = 4.1 (5-29) mcmol/l, Total Iron Binding Capacity = 36.0 (45-66) mcmol/l, Haemoglobin = 5.3 (13.0-17.0) g/dl], thrombocytosis {709 (150 - 400) x10^3/Ul} and hypoalbuminemia {11 (35 -50) g/l}. C-reactive protein was raised 103 mg/l and erythrocyte sedimentation rate was 15 mm/hr. Fibrinogen, protein S and C level was not available due to resource constraint.
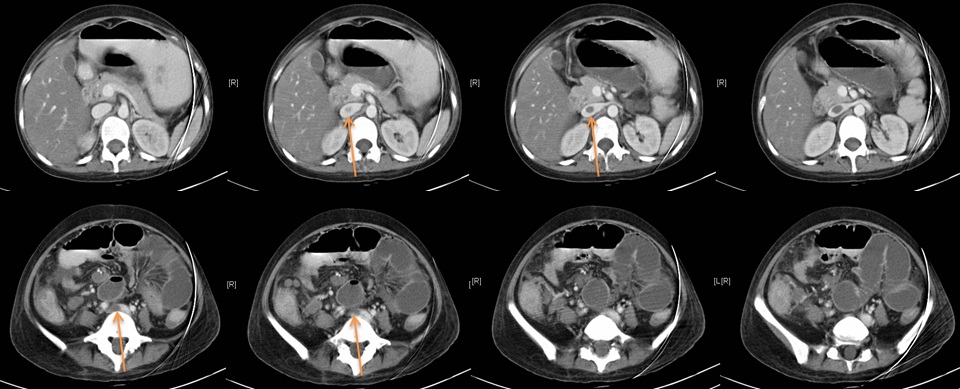
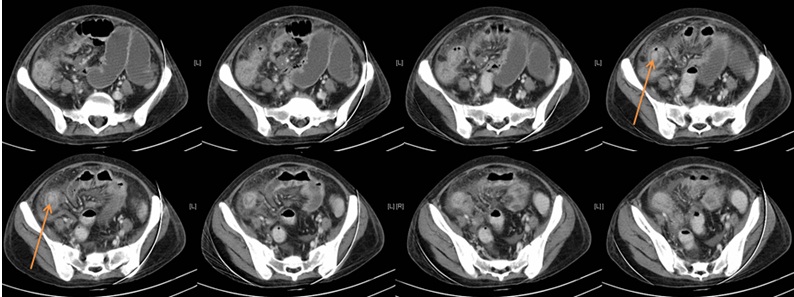
Contrast-enhanced Computed Tomography (CT) of the abdomen showed bowel within bowel over ileocecal junction. Ceacal mucosa was intussuscepted into terminal ileum. Small bowel proximal to terminal ileum was dilated. There was extensive fat stranding of the surrounding mesentery and omentum with multiple enlarged mesenteric nodes [Table/Fig-1]. There was a filling defect in the right common femoral, right external iliac and inferior vena cava (at the level of first lumbar vertebrae) in favour of venous thrombosis [Table/Fig-2].
Contrast-enhanced CT abdomen showing reverse intussusception with ceacal mucosa (contrast enhanced mucosa marked with arrow) invaginated into ileum with proximal dilatation of small bowel loops.
*CT Images are arranged cephalic to caudal from left to right.
Contrast-enhanced CT abdomen showing the proximal extent of the inferior vena cava (IVC) thrombus at the level of confluence of left renal vein to IVC (upper row) and distal extent of the thrombus extends beyond IVC into right common iliac vein (lower row).
*CT Images are arranged cephalic to caudal from left to right.
**The proximal and distal extent of the IVC thrombus marked with arrow
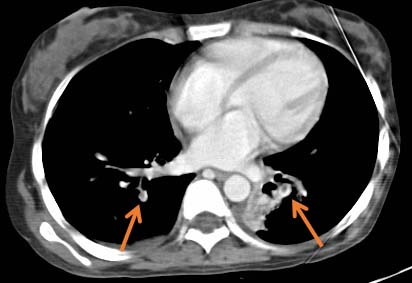
There was filling defect of visualised posterior lower lobe of sub-segmental branch of the both pulmonary arteries in keeping with emboli [Table/Fig-3].
CT image showing embolus in the posterior lower lobe sub-segmental branch of both pulmonary arteries (marked with arrow).
Due to high risk of further dissemination of the deep vein emboli, an inferior vena cava filter (IVC filter) was inserted via internal jugular vein prior to abdominal surgery. Following packed cell transfusion for her anaemic state, she was scheduled for an emergency laparotomy. Intraoperatively, there was an ileocecal intussusception with surrounding friable inflamed paracolic fat and small bowel mesentery. Limited right hemicolectomy was performed with double barrel stoma matured due to unhealthy bowel at the site of intussusception. Postoperative recovery was uneventful and hospitalised for two weeks.
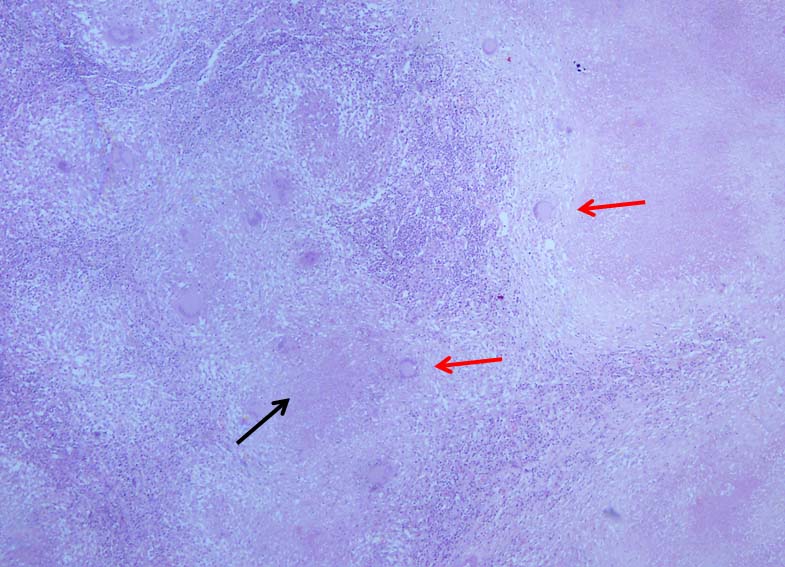
Gross examination of the resected specimen showed perforation at terminal ileum and caecum measuring 7x6 cm. Mucosa of the distal terminal ileum, caecum, ascending colon appeared ulcerated and nodular corresponding to the site of perforation measuring 2x3 cm. On microscopy, caecum and terminal ileum showed extensive areas of mucosal ulceration with multiple foci of large caseating granuloma with multinucleated giants cells and small lymphocytic reaction seen at mucosa, submucosa, muscularis propria and serosa [Table/Fig-4]. Staining for acid fast bacilli was positive. Mesenteric lymph nodes showed epithelioid granuloma with extensive areas of necrosis.
Haematoxylin & eosin slide showing areas of caseating granuloma (black arrow) and multinucleated giant cells (red arrow) at magnification 40X.
She was treated by the respiratory physician with a four drugs regimen which is isoniazid, rifampicin, ethambutol and pyrazinamide for two months. After two months, she responded to treatment with increased weight gain. Isoniazid and rifampicin were continued as a daily therapy for another four months. Warfarin was initiated, but a therapeutic International Normalized Ratio (INR) was difficult to maintain due to drug-drug interaction with rifampicin. She required more meticulous adjustment for optimisation of warfarin.
There was no residual pulmonary embolus or any thrombus in the IVC and lower limb deep vein on a repeated CT pulmonary angiogram scan and Ultrasound Doppler seven months after the surgery. Stoma reversal was performed two months later. A perioperative switch of anticoagulation from warfarin to heparin was required prior to the surgery. Postoperatively, she was maintained with dabigatran until the removal of IVC filter three months later.
Discussion
Abdominal tuberculosis resulting in venous thromboembolism can be due to many causes. One of the most common explanation is due to an inflammatory response which triggers an elevated fibrinogen levels with impaired fibrinolysis coupled with a decrease in antithrombin III and reactive thrombocytosis [1]. Secondly, patients with severe tuberculosis are often dehydrated due to extended period of appetite loss. According to Poiseuille’s Equation, when fluid in plasma is diminished due to dehydration, the blood viscosity will increase and result in a reduced blood flow and increased prothrombotic state [2]. The third reason is attributed to the use of antitubercular drugs such as rifampicin. This drug is associated with a four times higher risk of deep vein thrombosis in retrospective analysis of 1366 adults TB patients [3]. The occurrence of thrombosis usually happened two weeks from the commencement of the antitubercular drugs. Lastly, enlarged lymph nodes due to cell mediated immunity can cause compressive effects on blood vessels which result in vascular thrombosis [4,5].
Gogna A et al., described two cases of Deep Vein thrombosis (DVT) secondary to tubercular lymphadenitis of which both were aged 21 and 60 years old. Both patients had enlarged para-aortic lymph nodes that caused vena cava obstruction which led to bilateral DVT [4]. Another report by Gathwala G et al., of a 13-year-old girl with abdominal tuberculosis with DVT was due to a decreased level of antithrombin III [6]. Likewise, a report by Gupta R et al., of a 13-year-old girl with abdominal tuberculosis from Afghanistan developed DVT but with no explainable cause [7]. This clearly demonstrates that DVT caused by abdominal tuberculosis varies from patient to patient and all cases were successfully treated with standard antitubercular regimen and anticoagulation. Our patient had abdominal tuberculosis which was complicated by reverse ileocecal intussusception and venous thromboembolism. An IVC filter was inserted to prevent further emboli dissemination into the pulmonary trunk. Subsequently, she was successfully treated with an emergency laparotomy with limited right hemicolectomy and delayed anastomosis.
Warfarin was the drug of choice for anticoagulation, which required more frequent INR monitoring. This is due to the drug-drug interaction of the anti-TB drugs with warfarin. Warfarin is metabolised by CYP450 pathway similar to rifampicin and in contrast isoniazid inhibits it [8]. Therefore, she was switched to dabigatran, a direct thrombin inhibitor which has less interaction with anti-TB medications. Nevertheless, rifampicin is known to reduce the anticoagulant effect of dabigatran [9].
The complexity of the management of this case arises when she presented to us with pulmonary embolism and extensive DVT on top of intussuscepted ileocecal tuberculosis. Although the IVC filter was inserted, anticoagulation was still required as it prevents further thrombosis and formation of new thrombus below the filter.
Conclusion
Abdominal tuberculosis complicated with DVT and pulmonary embolism is a rare encounter. This can lead to mortality which is potentially preventable. Thrombo-prophylaxis is essential in the management of abdominal tuberculosis. Multidisciplinary team involving the interventional radiologist, chest physician, haematologist and acute care surgeon is the key for the optimal care in such a rare and complex case.
[1]. Robson SC, White NW, Aronson I, Woollgar R, Goodman H, Jacobs P, Acute-phase response and the hypercoagulable state in pulmonary tuberculosisBr J Haematol 1996 93(4):943-49. [Google Scholar]
[2]. Singh S, Randle LV, Callaghan PT, Watson CJE, Callaghan CJ, Beyond poiseuille: preservation fluid flow in an experimental modelJ Transplant 2013 2013:01-06. [Google Scholar]
[3]. White NW, Venous thrombosis and rifampicinLancet Lond Engl 1989 2(8660):434-35. [Google Scholar]
[4]. Gogna A, Pradhan GR, Sinha RS, Gupta B, Tuberculosis presenting as deep vein thrombosisPostgrad Med J 1999 75(880):104-05. [Google Scholar]
[5]. Sharma A, Sharma V, Abdominal aortic thrombosis and tuberculosis: an uncommon associationGastroenterol Rep 2014 2(4):311-12. [Google Scholar]
[6]. Gathwala G, Dalal P, Gehlawat V, Singh J, Arya V, A case of deep vein thrombosis and intracranial sinus thrombosisSultan Qaboos Univ Med J 2016 16(4):e516-19. [Google Scholar]
[7]. Gupta R, Brueton M, Fell J, Lyall H, An Afghan child with deep vein thrombosisJ R Soc Med 2003 96(6):289-91. [Google Scholar]
[8]. Sekaggya C, Nalwanga D, Von Braun A, Nakijoba R, Kambugu A, Fehr J, Challenges in achieving a target international normalized ratio for deep vein thrombosis among HIV-infected patients with tuberculosis: a case seriesBMC Hematol [Internet] 2016 16:01-05. [Google Scholar]
[9]. Härtter S, Koenen-Bergmann M, Sharma A, Nehmiz G, Lemke U, Timmer W, Decrease in the oral bioavailability of dabigatran etexilate after co-medication with rifampicinBr J Clin Pharmacol 2012 74(3):490-500. [Google Scholar]