Reconstruction of Maxilla with Titanium Mesh and Fascia Lata - A Case Report
Devkumar Rengaraja1, Mohan Jagade2, Karthik Rao3, Radhika Sonate4, Arpita Singhal5
1 Senior Resident, Department of ENT, Grant Medical college and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
2 Professor, Department of ENT, Grant Medical college and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
3 Senior Resident, Department of ENT, Grant Medical college and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
4 Senior Resident, Department of ENT, Grant Medical college and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
5 Senior Resident, Department of ENT; Grant Medical college and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Devkumar Rengaraja, Room No-216, 300 Resident Hostel, Grant Medical College and Sir JJ Group of Hospitals, Byculla, Mumbai-400008, Maharashtra, India.
E-mail: devkumar16@gmail.com
Maxillary defect reconstruction has been a grave challenge which unfortunately has stopped many ENT surgeons from attempting maxillectomy due to the fear of reconstruction. With our technique of reconstructing the maxillary defect with titanium mesh and fascia lata, the need for microvascular assistance is obviated. Here we describe a revision case of ameloblastoma of maxilla in a 33-year-old female for which total maxillectomy with reconstruction was done without the aid of microvascular tissue transfer. The aim of this article is to encourage and alleviate the fear among the ENT surgeons, in attempting maxillectomy and its reconstruction for delivering an equally good aesthetic and functional outcome especially at the centres where the facility of plastic assistance is not readily available.
Ameloblastoma, Class 3a defect, Maxillectomy
Case Report
A 33-year-old female presented to the ENT Out Patient Department with a swelling in the right maxillary sinus and the mass protruding through the right nostril [Table/Fig-1].
Clinical presentation- swelling in the right maxillary sinus and the mass protruding through the right nostril.

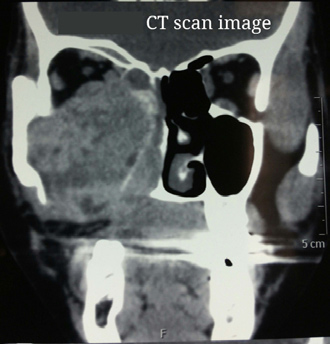
Patient was a diagnosed case of ameloblastoma for which she had underwent surgery twice in the past in the span of 10 years. The recurrence was due to inadequate clearance. Biopsy was taken and diagnosis was confirmed on histopathologial examination. A CT scan for the paranasal sinus [Table/Fig-2] and 3D face CT [Table/Fig-3] was done to know the extent of the disease.
CT scan image: A hetrogenous mass seen in the right maxillary sinus with evidence of bony destruction.
3D face CT image showing the bony destruction and the bony wall defect.

A complete biochemical, routine blood investigations and chest X-ray were done prior the surgical intervention [Table/Fig-4]. Patient underwent a revision surgery, right total maxillectomy, under general anaesthesia with aseptic precautions creating a class 3a defect as per Brown JS classification [1].
Diagnostic evaluation table.
| Parameter | Results | Normal |
|---|
| Haemoglobin | 12.9 gm/dl | 11.0–13.3 gm/dl |
| White blood cells | 6400/mm3 | 4500–10500/mm3 |
| Neutrophils | 65% | 50-70% |
| Lymphocytes | 28% | 20-40% |
| Monocytes | 5% | 2-8% |
| Eosinophils | 2% | 1-4% |
| Basophils | 0 | 0.5-1% |
| Platelet count | 3.5×106/mm3 | 1.94–364 × 106/mm3 |
| INR | 1.06 | 1-1.4 |
| APTT | 35 sec | 42-54 sec |
| PT | 14 sec | 11-15 sec |
| BUN | 12 mg/dl | 7-17 mg/dl |
| Creatinine | 0.8 mg/dl | 0.3-0.9 mg/dl |
| Na+/K+ | 141/ 4.2 mEq/l | (Na+) 135–148 mEq/l (K+) 3.5–58 mEq/l |
| Total protein | 6.8 gm/dl | 5.9-80 gm/dl |
| Albumin | 4.8 gm/dl | 3.7-5.6 gm/dl |
| Total Bilirubin | 0.9 mg/dl | 0.2-1.0 mg/dl |
| ALT (SGPT) | 12 IU/l | 5-35 IU/l |
| AST (SGOT) | 12 IU/l | 5-40 IU/l |
| Alkaline phosphatase | 135 IU/l | 115–345 IU/l |
| Histopathological biopsy report | Ameloblastoma of odentogenic origin | |
| CT scan report | A post-partial maxillectomy status with heterogenic mass seen in the right maxilla and right nostril filling the other sinuses with evidence of bony destructions and orbital floor erosion | |
*INR-International Normalized Ratio, APTT-Activated Partial Thromboplastin Time, PT- Prothrombin Time, BUN-Blood Urea Nitrogen, AST-Aspartate Transaminase, ALT-Alanine Transaminase
Total Maxillectomy was done taking a modified Weber-Ferguson incision respecting the facial asthetic subunits. Skin and soft tissue flaps were raised. The tumour was exposed from all the edges and complete clearance was achieved with osteotomies performed freeing it from all the edges.
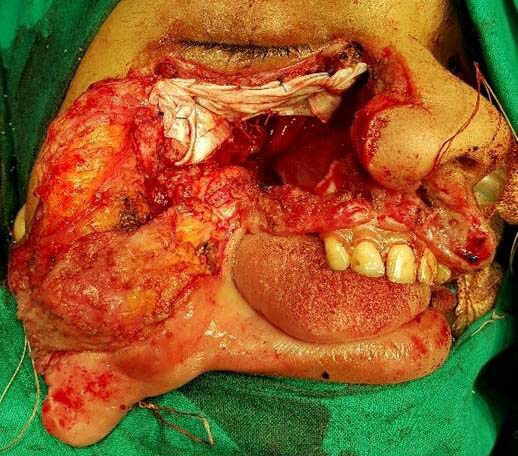
In this the infraorbital plate, zygoma, anterior maxillary wall, ipsilateral hard palate and upper lateral dentition were absent because of the previous surgeries. The mucosa over the hard palate and the soft palatal tissue which were free of tumour were preserved. This created a Class 3a defect (total maxillectomy with ipsilateral removal of the alveolus and the infraorbital floor with the orbital contents intact) after complete excision of the tumour [Table/Fig-5]. Complete clearance of the disease was done and haemostasis was achieved.
Class 3a defect: showing total maxillectomy with removal of ipsilateral alveolus and infraorbital floor with the orbital contents intact.

Reconstruction of the class 3a defect posed a grave challenge. The defect was reconstructed with the help of a titanium orbital mesh and tensor fascia lata.
Tensor fascia lata of about 8x5 cm was harvested from the right side of lateral part of thigh for which a vertical incision was taken under aseptic precautions. Primary closure was done by layered suturing with vicryl and ethilon. A double layered fascia lata was sutured with round body prolene suture on the under surface of the orbit supporting the orbital content to prevent its prolapse was fixed in place by anchoring it to frontonasal process of maxilla and zygomatic prominence remanant. This also avoids the entrapment of the periorbital fat with the titanium mesh. Precautions were taken to prevent injury to the globe [Table/Fig-6].
Reconstruction with fascia lata.
The titanium orbital mesh plate was bent with a plate bender to form an inverted L shape [Table/Fig-7]. Measurement was taken from the incisor to the inferior orbit floor which formed the anterior maxillary wall. The straight plate was then bent a in such a fashion that, the upper half of the mesh supported the orbital contents, while the lower part formed the anterior wall of maxilla thus supporting the cheek skin and soft tissue. To fix the plate in that position, the plate was screwed to the bony prominences-the zygomatic eminence, frontonasal process of nasal bone with self-tapping screws and the alveolar margin of the incisor with prolene sutures [Table/Fig-8]. The cavity was filled with a roller gauge soaked in framycetin sulfate ointment which was kept in for 24 hours. The skin flap was reposited and suturing was done in layers with vicryl and prolene sutures. Immediate postoperative period was uneventful and patient didn’t have any visual symptoms. The nasal pack was removed after 24 hours. The postoperative specimen’s histopathological report was consistent with the preoperative diagnosis and the tumour was proved to have adequate free margins in all the dimensions. Patient was fitted with a dental prosthesis after one month. The patient was followed up for one year and bilateral facial symmetry was satisfactory. During follow up, no infection or foreign body reaction was encountered [Table/Fig-9a,b].

Reconstruction with titanium mesh.

a) Follow up after two weeks; b) Follow up after one year.

A detailed patient’s consent was procured for using her images for the article. The results were satisfactory in terms of vision and eye movements. There was no sagging of the orbit indicating the fascia lata supported the orbit and its content adequately. The aesthetic look of the patient and bilateral facial symmetry was maintained due to the support offered by the titanium mesh. Moreover, there was no postoperative complication and no foreign body reactions noted in the follow up period. As the maxillary cavity was not filled with any soft tissue, examining the cavity for any early recurrence during the follow up period was easier as compared with free tissue transfer.
Discussion
Maxilla is the central bone of midface, supporting the anterior facial and cheek skin, orbit and dentition. It separates the oral and orbital cavities and also provides skeletal support to the orbital contents. Maxillectomy is a complex procedure which has a negative impact on nutrition, speech, communication, deglutition, social acceptability and self image. Odontogenic tumours like ameloblastoma requires an ablative surgery as chances of recurrence are very high, if not resected completely. Maxillectomy defects if not reconstructed leads to aesthetic and functional deficits [2]. Hence, defect reconstruction becomes essential for a good postoperative rehabilitation to improve the quality of life. Reconstruction becomes mandatory when a higher class of defect is created namely class 3 and 4 [3]. Conservative treatment by mere resection and primary soft-tissue closure will result in loss of both soft and hard tissue support resulting in a shallow defect on the face. A radical excision of the tumour followed by an adequate reconstruction can improve survival and provide more satisfactory functional and aesthetical outcome. In the management of the maxillary tumours, it’s not only the treatment modality that requires multidisciplinary decision making, but also the method of rehabilitation.
In the reconstruction of maxillary defects secondary to trauma or ablative tumour surgery one needs to restore: (1) essential functions of the midface; (2) provision for adequate structural support; and (3) aesthetic reconstruction of the external features [4]. Thus, the aim of a class 3 defect reconstruction is to close oro-nasal fistula, restore dentition, support face and nose, restore orbital floor and to maintain the contour of cheek [1]. Various free flap tissue transfer techniques have been described which requires an expert plastic surgery and microvascular assistance or virtual planning and the use of rapid prototyping mainly used in cranio-maxillofacial surgery [5]. Due to the use of specialised software systems, applications of these techniques are limited to only larger medical centers. The other disadvantages estimated are the additional costs for software and computers and the additional time required for planning the operation [5]. In those setups which lack efficient plastic surgery assistance and facilities of high technology computer assistance, the reconstruction of such class 3a maxillary defect becomes a grave challenge. The difficult nature of reconstructing the huge defect poses a dilemma for many otolaryngologists from operating such cases and providing a complete clearance. The other problems of free flap tissue transfer were donor site failures. In non-vascularised bone flaps, chances of necrosis and infections were high. Free flap reconstruction usually requires a neck dissection for anastomosis which in turn increases the morbidity and mortality [3]. Moreover, the challenge of providing long pedicles for anastomosis of the vessels wasn’t evaded. This also included the difficulty of dehiscence in larger defects more than 4 cm which resulted in immediate or late trismus. Also these flaps made dental rehabilitation difficult due to the contraction and obliteration of the sulcus following epithelisation [3]. These difficulties are ruled out with our technique of reconstruction with titanium mesh and fascia lata which are easily available, economic, requires less time for harvesting and reconstructing, has a smaller learning curve and provides comparable outcome to the free flap tissue transfer. Moreover, during the follow up period the detection of any early recurrence is possible with our technique as the maxillary cavity isn’t filled up with soft tissue unlike the cavity defect when reconstructed with free tissue transfer. Dediol E et al., had reported the use of prefabricated titanium mesh with soft tissue free flap for reconstructing a class 3 maxillary defect. The mesh was bent on a 3D skeletal model intraoperatively. The postoperative results were found to be satisfactory. Though, in few cases they have mentioned about the mesh exposure post radiotherapy [6]. However, when reconstruction was attempted by our method where the mesh was bent in an appropriate fashion, the need for free flap was obviated and better results were obtained. Moreover, the need for neck dissection for long pedicles for anastomosis was negated thus reducing the operative time and reducing the morbidity and mortality of the patient. The aesthetic outcome of the titanium mesh is better as it can be molded as per the contour on the other side, on the contrary to the free tissue which invariably gives a bulge to the midface. This is a very economic and simple way of reconstruction. it marks an alternative for the more tiring reconstructive techniques and provides equally good functional and aesthetic outcome.
Limitation
It requires requisite expertise for bending the titanium plate and fixing it in place. Radiotherapy may cause dehiscence of the plate which might limit its use in cases which require postoperative radiotherapy.
Conclusion
Reconstruction is essential. Though there are numerous methods of reconstructing a Class 3 a maxillary defect, reconstructing the defect with titanium mesh and fascia lata is a safe, easier, economic and less time consuming. It also requires less expertise in reconstruction, giving an equally good aesthetic and functional outcome. All this can be achieved at the same sitting without any microvascular assistance.
*INR-International Normalized Ratio, APTT-Activated Partial Thromboplastin Time, PT- Prothrombin Time, BUN-Blood Urea Nitrogen, AST-Aspartate Transaminase, ALT-Alanine Transaminase
[1]. Brown JS, Maxillary reconstructionIndian Journal of Plastic Surgery 2007 40(12):35 [Google Scholar]
[2]. Gellrich NC, Schramm A, Hammer B, Rojas S, Cufi D, Lagrèze W, Computer-assisted secondary reconstruction of unilateral posttraumatic orbital deformityPlastic and reconstructive surgery 2002 110(6):1417-29. [Google Scholar]
[3]. Iyer S, Thankappan K, Maxillary reconstruction: Current concepts and controversiesIndian Journal of Plastic Surgery 2014 47(1):8 [Google Scholar]
[4]. Muzaffar AR, Adams Jr WP, Hartog JM, Rohrich RJ, Byrd HS, Maxillary reconstruction: functional and aesthetic considerationsPlastic and reconstructive surgery 1999 104(7):2172-83. [Google Scholar]
[5]. Lethaus B, Kessler P, Boeckman R, Poort LJ, Tolba R, Reconstruction of a maxillary defect with a fibula graft and titanium mesh using CAD/CAM techniquesHead & face medicine 2010 6(1):1 [Google Scholar]
[6]. Dediol E, Uglešic V, Zubcic V, Kneževic P, Brown class III maxillectomy defects reconstruction with prefabricated titanium mesh and soft tissue free flapAnnals of plastic surgery 2013 71(1):63-67. [Google Scholar]