Intertrochanteric fractures of the femur are extremely common fractures occurring in elderly osteoporotic individuals. Recumbency following a hip fracture is known to be associated with increased mortality in this group of patients. Surgical treatment is now the accepted standard of management to attain acceptable reduction and early mobilization in the elderly osteoporotic individual [1]. Obtaining a successful fixation is of paramount importance in this group of patients because implant failure has disastrous complications and revision surgery is a highly morbid procedure owing to these patients’ poor general condition; thus, evidence regarding the ideal implant that would provide enduring fixation for such fractures, has continued to be a topic of on-going research for several years.
The dynamic hip screw, which has become the gold standard treatment of stable fractures, was found to be inappropriate to treat the unstable class of intertrochanteric fractures [2]. For fixation of unstable fractures, the use of an intramedullary nail coupled with a dynamic femoral head/neck stabilization implant is the ideal method [3]. Over time, various designs of nails incorporating a single compression screw or a compression screw coupled with an antirotation screw like the PFN, have become popular for treating unstable fractures. Although PFN proved to be superior to extramedullary devices for unstable intertrochanteric fractures, screw cut-out, back out, varus collapse and rotational instability continued to be significant postoperative complications, with up to 31% complication rates being reported in literature [4]. The PFNA was designed to achieve better stabilization of the femoral head and neck by using a single helical blade rather than a screw system for fixation. The helical blade is said to increase the bone-implant interface and result in compaction of cancellous bone, thereby providing excellent stability of fixation [5]. The blade, which can be inserted without reaming out bone from the head/neck fragment, seems to provide additional anchoring, particularly in osteoporotic bone. Biomechanical studies have proven that the helical blade, by compaction of cancellous bone around it, has superior resistance to rotation and varus collapse [6]. Clinical trials are needed to confirm whether this superior biomechanical performance also has benefits in terms of functional outcomes and complication rates. However, studies on fixation with the helical blade have shown that this can also be associated with cut-through into the hip joint, cut-out and back-out just like other implant designs [7].
This prospective clinical trial was performed to compare the functional outcomes and complications with the use of PFN and PFNA in treatment of unstable intertrochanteric fractures and assess their comparative performance in the setting of osteoporosis.
Materials and Methods
The study was an eighteen-month prospective comparative study from 1st December 2013 to 1st June 2015 conducted in the Department of Orthopaedics, Christian Medical College and Hospital, Ludhiana, Punjab, India. Approval for the study was obtained from the Institutional Ethics Committee. All skeletally mature patients with unstable intertrochanteric AO 31.A2 and 31.A3 fractures presenting to the institution during this period, after applying the exclusion criteria, were included in this study. Those with stable 31.A1 type intertrochanteric fractures, those immobile or bed-ridden prior to injury and those with previous implants in the fractured hip or femur were excluded. The study included 48 patients with unstable intertrochanteric fractures treated with either PFN or PFNA, who were followed up for a minimum of nine months.
The A.O. alphanumeric classification [8] was used to classify the fractures after obtaining radiographs – an anteroposterior view of the pelvis with both hips and a lateral view of the affected hip. Singh’s index [9] was used to grade the radiographs for the degree of osteoporosis. Preoperative and postoperative haemoglobin and units of blood transfused were recorded. The operative time was recorded as per the anaesthesia record sheet.
The quality of reduction was assessed by comparing the neck-shaft angle of the operated hip, to that of the normal hip on the antero-posterior view. A variation of less than 5 degrees from the normal side was considered a ‘good’ reduction. Between 5 and 10 degrees of variation was considered ‘acceptable’ and more than 10 degrees variation was considered ‘poor’ [10].
The quality of fixation was assessed using the tip-apex distance described by Baumgaertner MR [11] and the Cleveland index [12]. A tip apex distance <25 mm is protective of the screw cutting out of the femoral head and was considered adequate for both type of implants. The tip apex distance was measured using the Picture Archiving and Communication System (PACS) tool on the immediate postoperative radiographs. The Cleveland index [12] was used to assess the position of the compression screw in PFN and helical blade in PFNA. A centre-centre or centre-inferior placement of the compression screw or helical blade was considered optimal.
Functional outcomes were assessed using the Parker and Palmer mobility score [13]. The pre-injury mobility score was noted and compared with the score at final follow up as a measure of return of mobility. The Harris Hip score [14] was calculated at final follow up to assess hip function post surgery. Any complications encountered during the follow up period namely deep infection, acetabular penetration, blade/screw migration, nail breakage, non-union, rotation failure or screw/blade loosening were documented for both groups of patients. Complications occurring in patients with Singh’s grade ≤ 3 in both groups were also compared.
Statistical Analysis
Quantitative variables were compared using unpaired t-test/ Mann-Whitney test and qualitative variables were correlated using Chi-square test/Fisher’s exact test. A p-value of less than 0.05 was considered significant. The data was entered in MS Excel spreadsheet and statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 16.0.
Results
Of 48 patients with AO type 31.A2 and 31.A3 fractures, 23 were treated with PFN and the other 25 with PFNA. The average age of the PFN group was 60.78 years (30-90 years) and that of the PFNA group was 74.12 years (37-96 years). The difference in age distribution of the two groups was significant (p=0.05) with the PFNA group being older. Demographic data is tabulated in [Table/Fig-1].
Demographic data and patient distribution of the two groups.
| Variables | PFN (23) | PFNA (25) |
|---|
| Average age (in years) | 60.78 | 74.12 |
| Gender DistributionMalesFemales | 16/23 (69.5%)7/23 (30.5%) | 10/25 (40%)15/25 (60%) |
| Percentage of patients with 31.A3 fractures | 7/23 (30.4%) | 3/25 (12%) |
| Percentage of patients with significant osteoporosis (Singh’s index ≤ 3) | 8/21 (38.09%) | 13/24 (54.1%) |
| Distribution by Singh’s grade in those with significant osteoporosisGrade 3Grade 2 | 6 (75%)2 (25%)0 (0%) | 9 (69.2%)3 (23.1%)1 (7.7%) |
Degree of Osteoporosis
For two patients in the PFN and one in the PFNA group, the Singh’s index could not be assessed due to previous implants in the opposite hip. In the PFN group, 8 of 21 patients (38.09%) and in PFNA group, 13 of 24 patients (54.16%), had a Singh’s index of 3 or less indicating significant osteoporosis. This distribution of osteoporotic individuals in the two groups was not significantly different (p = 0.15). However, the relatively greater number of patients with radiological osteoporosis in the PFNA group correlated with the average age of the two groups, with the PFN group being more than 10 years younger.
A detailed description of the results has been summarized in [Table/Fig-2].
Comparison of PFN and PFNA groups in terms of quality of fixation, functional outcomes and complications.
| Parameters | PFN (23) | PFNA (25) | p-value |
|---|
| Percentage with tip-apex distance (TAD) ≥ 25 mm | 4 (17.4%) | 8 (32%) | 0.32 |
| Percentage with sub-optimal position (as per Cleveland index) | 4 (17.4%) | 8 (32%) | 0.32 |
| Average postoperative Harris hip score | 75.37 | 78.85 | 0.54 |
| Return to preinjury status (as per Parker Palmer mobility score) | 8 (34.7%) | 8 (32%) | 0.83 |
| Complications (overall) | 8 (34.7%) | 3 (12%) | 0.08 |
| Complications (implant related) | 7 (30.4%) | 1 (4%) | 0.02 |
| Complications (in patients with Singh’s index 3 or less) | 3 (37.5%) | 0 (0%) | 0.04 |
(Quantitative variables were compared using unpaired t-test/Mann-Whitney test and qualitative variables were correlated using Chi-square test/Fisher’s-exact test)
The average drop of haemoglobin post-surgery was similar for the two groups (p=0.61). The operative time was found 40 minutes lesser for PFNA group; however this measure was not purely of procedural time, but instead was from anaesthesia record sheets.
Comparison of Reduction and Fixation
Quality of Reduction: Reduction could not be accurately assessed in two patients in PFN group and one patient in PFNA group (due to previous implants in the opposite hip, not allowing assessment of neck shaft angle). In the PFN group 71% (15/21) of patients and in the PFNA group 83% (20/24) of patients had a good reduction [Table/Fig-3,4]. Only one patient had a poor reduction as per our criteria (from PFNA group), but no complication was encountered. Implant failure occurred in four cases with good reduction of which three were from the PFN group.
A 31.A3 fracture treated with PFN, with good union at one year follow up.

A 31.A2 fracture treated with PFNA with good union at eight months follow up.

Tip-apex Distance: The average Tip Apex Distance (TAD) for both groups was well within the described safe limit of 25 millimeters. It was 19.08 mm for the PFN group (range 8.42–27.37 mm) and 21.13 mm for the PFNA group (range 11.08–36.1 mm). The average TAD for cases of implant failure in the PFN group was 22.21 mm whereas the one patient with implant failure with PFNA had a TAD of 32.32 mm. In seven other cases of TAD > 25 mm with the PFNA no implant failure was seen.
Implant Position as per Cleveland Index: In the PFN group 19 of 23 patients (83%) and in the PFNA group 17 of 25 patients (68%) had an optimal implant position in the femoral head i.e., either centre-centre or inferior-centre. Only two cases of failure with the PFN had a sub-optimal implant position and the single case of PFNA failure also had a sub-optimal position (superior-centre).
Comparison of Functional Outcomes
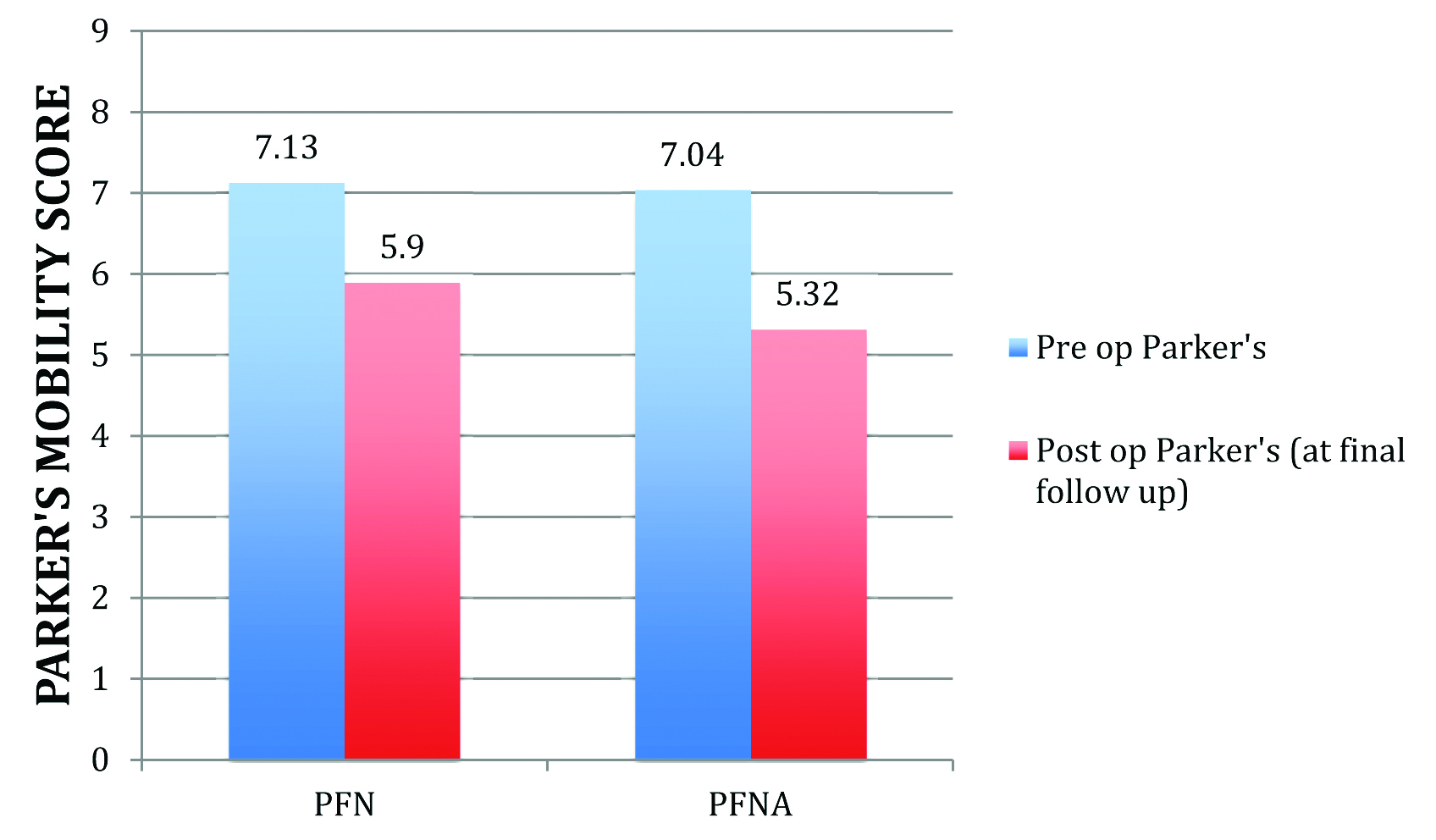
Parker’s Mobility Score and Return of Mobility [Table/Fig-5]: The average postoperative Parker’s mobility score achieved at final follow up was identical in both groups of patients (5.9 for PFN vs 5.32 for PFNA) and the difference was not statistically significant. An identical percentage of patients from both groups were able to return to their pre-injury level of Parker’s score – 8/23 (35%) in the PFN group and 8/25 (32%) in the PFNA group.
The preoperative and postoperative Parker’s mobility score at final follow up.
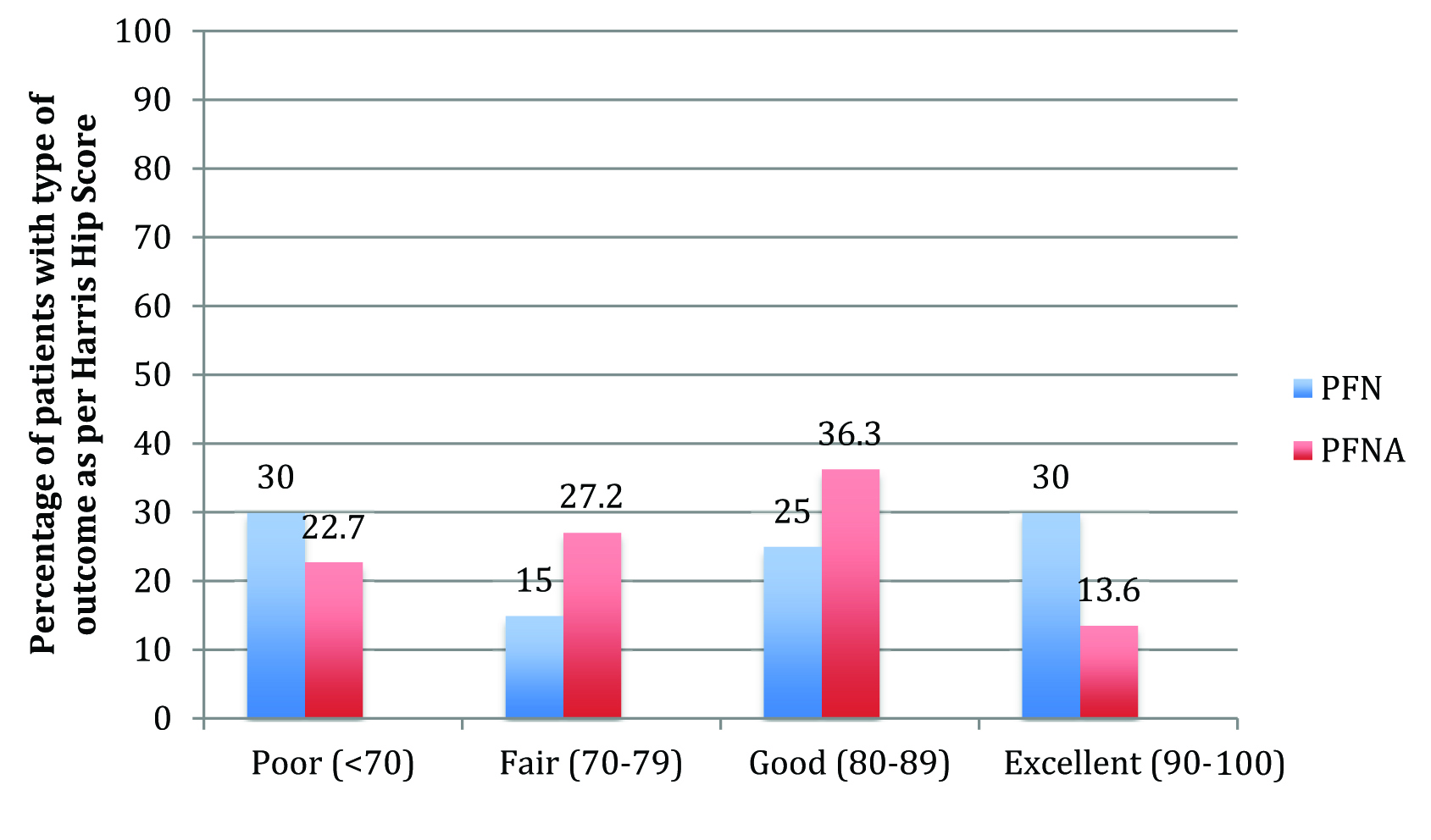
Harris Hip Score [Table/Fig-6]: The average Harris Hip Score obtained at final follow up was identical in the two groups of patients – 75.37 for the PFN group and 78.85 for the PFNA group. The average Harris Hip Score for cases of implant failure in the PFN group was 41.3. The case of medial migration with the helical blade of PFNA showed radiological varus collapse but continued to have good hip function with a score of 86.
A comparison of Harris hip scores obtained at final follow up with the two implants.
Comparison of Complications [Table/Fig-7]: Seven patients (30.4%) in the PFN group suffered an implant related complication whereas only one patient (4%) from PFNA group suffered an implant related complication [Table/Fig-8]. The difference in implant related complication rates was found to be statistically significant (p=0.02). There was one case of deep infection encountered in both groups, which was not considered as an implant related complication. One patient from the helical blade group died from an unrelated medical cause.
The number and type of implant related complications encountered with both devices.
| Complications | Group | Total |
|---|
| PFN | PFNA |
|---|
| Screw/blade cut-out | 1 (14.2%) | 0 | 1 (12.5%) |
| Screw back-out | 2 (28.4%) | 0 | 2 (25%) |
| Medial migration or reverse Z effect | 2 (28.4%) | 1 (100%) | 3 (37.5%) |
| Z effect | 1 (14.2%) | 0 | 1 (12.5%) |
| Implant breakage | 1 (14.2%) | 0 | 1 (12.5%) |
| Total | 7 (100%) | 1 (100%) | 8 (100%) |
A 31.A3 fracture treated with a helical blade showing varus collapse of the fracture and medial migration of the blade at six weeks.

Complications in patients with Singh’s index ≤ 3: Three of eight patients with significant osteoporosis in PFN group suffered from implant failure whereas none of the 13 patients in PFNA group with significant osteoporosis suffered implant failure. This difference in complication rates in the setting of osteoporosis was found to be significant (p=0.04). The complications encountered in these osteoporotic cases were implant breakage, screw back out [Table/Fig-9] and Z effect. In the former two cases, both the TAD as well as implant position was optimal and the Singh’s grade was 3. In the case with Z-effect, the TAD was 26.47 mm and the Singh’s grade was 2. In the PFNA group, four patients with Singh’s grade of 3 had TAD > 25 mm but none of these showed blade migration or failure.
A case of back-out of the compression screw of a dual screw design over six weeks after initial fixation.

Discussion
Management of unstable intertrochanteric fractures continues to pose a challenge to orthopaedic surgeons, which is further compounded by the effect of osteoporosis on the outcome of these injuries [15]. Biomechanical studies have proven that osteoporosis is an important determinant of screw migration in the proximal femur, thereby predisposing to implant failure [16]. Clinical studies have also shown that osteoporosis is associated with inferior outcomes in intertrochanteric fractures [17]. Therefore, various methods are being used in attempt to improve fixation in osteoporotic intertrochanteric fractures, including cement augmentation [18] and improvements in implant design. The search for an ideal implant for these osteoporotic fractures continues and is evidenced by the variety of nail designs available today.
A significant innovation in improving fixation in these fractures was that of a helical blade device. The idea behind the innovation of the helical blade was its biomechanical superiority in the setting of osteoporosis [6]. The blade can be inserted without reaming, thereby preserving vital bone stock in the femoral head. During insertion, it compacts cancellous bone around it, providing a better purchase, with increased resistance to varus collapse and rotational stress [19]. The present study provides evidence that compared with the conventional PFN; this results in lesser complications in the clinical setting in an osteoporotic patient group.
It the present study, it was generally preferred to use PFNA in older patients, owing to its theoretical advantage of better purchase in osteoporotic bone. This is the reason that the PFNA group was significantly older than the PFN group, although comparable on other parameters. Our results show no statistically significant differences in the functional outcomes between the two implants as determined by the Harris Hip Score and Parker’s mobility score, but a significantly lower complication rate overall.
Our results are consistent with other studies comparing these implant designs. Mora A et al., compared the PFNA (helical blade) with PFN and found a lower incidence of cut-out with the PFNA [20]. Choo SK et al., found less postoperative sliding of the PFNA compared to PFN, but similar to our study, no difference in the walking capacity of the patients with either implant [21]. In contrast, Park JH et al., found significantly better social function scores, mobility scores and complication rates with helical blade nails [22]. Gardenbroek et al., in their study found that the risk of a secondary late complication and re-surgery is much higher with a PFN than the helical blade device [23].
Other advantages of the helical blade device over a two-screw design reported in literature include its ease of insertion, lesser operative time [24-26] and lesser fluoroscopic exposure [25,26]. Similar to the findings in these studies, we found the average time of surgery (from the onset of anaesthesia induction to the end of anaesthesia monitoring) to be 40 minutes shorter when a helical blade was used. This is at best a rough estimate since our measurement was not purely of procedural time. We did not find any significant difference in the amount of blood loss or need for transfusion after surgery with the use of either implant, but this benefit has also been mentioned in literature [24]. Stern R et al., analysed whether the use of a single helical blade improves positioning of the device in the femoral head and found no difference in implant positioning between nails employing blades and screws [27]. In our study, the number of patients with optimal implant position was lesser in the helical blade group (17 of 25 as compared to 19 of 23 in PFN group), hence supporting their finding.
There is however, little reporting in literature of clinical studies comparing the helical blade to other cephalo-medullary nails in the setting of osteoporosis. In the present study, implant failure was seen in three of eight cases with definite osteoporosis in the PFN group and none of the 13 patients in the PFNA group, indicating a better performance of the helical blade in osteoporotic bone. It is known that osteoporosis predisposes to implant failure in intertrochanteric fractures, especially if the device is malpositioned [28]. In the present study, in four cases of grade 3 osteoporosis, the helical blade held in spite of a TAD > 25 mm. This is attributed possibly to the advantages of helical blade in terms of preservation of vital bone stock and compacting the available bone stock around it during insertion. Siwach RC et al., used a helical blade extramedullary device in 51 patients with Singh’s index 3 or lesser and reported a 4% complication rate, comparable to our results with PFNA [29]. However, the Singh’s index is at best, a subjective indicator of osteoporosis [30] and this must be kept in mind while drawing an inference from our findings and of others using this index as an estimate of osteoporosis.
Limitation
Being a single centre trial, our study has the limitation of a small sample size, operated by two senior surgeons. Due to the short period of follow up (minimum nine months), we cannot comment on the long term complications, if any, of these implants. Our use of the Singh’s index rather than a Dual Energy X-Ray Absorptiometry (DEXA) scan to assess osteoporosis was due to financial constraints and makes our inference of the effect of osteoporosis on the performance of these implants subjective.
Conclusion
To conclude, we infer that once fracture union occurs, functional outcomes are similar irrespective of the type of implant used. The number of implant related complications however, is less when a helical blade device is used, indicating its biomechanical superiority over a dual screw design. PFNA has a superior performance over PFN in the setting of osteoporosis, which is attributed to compaction of cancellous bone by the helical blade. Nevertheless, it must be remembered that no implant design can compensate for poor reduction or poor implant placement in these fractures.