Evaluation of Anti-Cyclic Citrullinated Peptide Autoantibodies and C-Reactive Protein in Common Autoimmune Skin Diseases with and without Arthritis
Bandana Kumari1, Pawan Kumar2, Radha Krishna Prasad Chaudhary3
1 Assistant Professor, Department of Biochemistry, Vardhman Institute of Medical Sciences, Pawapuri, Nalanda, Bihar, India.
2 Ex-Resident, Department of Radiology, Darbhanga Medical College and Hospital, Darbhanga, Bihar, India.
3 Professor and Hod, Department of Skin and VD, Patna Medical College and Hospital, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bandana Kumari, Road No. 2, Brindavan Colony, Near Kidzee School, Phulwari sharif, Patna-801505, Bihar, India.
E-mail: drpawan.kumar@yahoo.com; drbandana.kumari@yahoo.com
Introduction
Anti-Cyclic Citrullinated Peptides (CCPs) are a well known diagnostic and prognostic noble marker for rheumatoid arthritis. C-Reactive Protein (CRP) is an acute phase protein whose level rises in response to inflammation.
Aim
This study was undertaken to show the role of the two markers (anti-CCPs and CRP) in autoimmune skin disorder and their association with associated arthritis in these disorder.
Materials and Methods
Serum anti-CCP antibodies and CRP was measured in 50 patients of autoimmune skin disease of which 28 were of psoriasis, 12 of Systemic Lupus Erythematosus (SLE) and 10 of Pemphigus Vulgaris (PV). These patients were categorised in two groups, with associated arthritis and without arthritis. The serum level of anti-CCP and CRP was correlated with the presence or absence of arthritis in these patients. Control group consists of 20 healthy subjects in which these two parameters were measured.
Results
Out of total of 50 patients, anti-CCP was raised in 36.37% of patients with associated arthritis and 12.82% of patients without arthritis whereas CRP was raised in 63.63% of patients with arthritis and 35.89% of patients without arthritis. Mean serum anti-CCP in patient with arthritis was 15.78±13.94 U/ml and without arthritis was 7.56±7.68 U/ml with p=0.01 which was statistically significant. Mean serum CRP in arthritis was 21.11±15.51 mg/l and CRP without arthritis was 13.14±12.27 mg/l with p=0.07 which was statistically not significant.
Conclusion
Although both anti-CCP and CRP are valuable markers for autoimmune skin disorder, anti-CCP seems to show significant association with arthritis.
Pemphigus Vulgaris, Rheumatoid Arthritis, Systemic Lupus Erythematosus
Introduction
Anti-CCP are autoantibodies against citrullinated peptide and proteins. During inflammation arginine residues present in some protein get converted into citrulline residue, a process called citrullination. This leads to drastic change in their shape because of which these proteins are recognised as antigen by immune system thus leading to antibody formation [1].
CRP is an acute phase protein and was the first Pattern Recognition Receptor (PRR) to be discovered. PRRs are primitive part of immune system as they evolve even before adaptive immunity [2].
Psoriasis is an immune mediated, systemic and chronic disease with red, itchy scales all over the body due to overactive immune system that cause skin cells to grow at approximately ten times faster rate and accumulate to form plaques [3].
Interleukin-23 is the main culprit of psoriasis. It leads to the production of other interleukins i.e., IL-17 and IL-22 that has direct role in skin inflammation and flaring of psoriasis [4].
SLE is a chronic autoimmune disease that can affect any organ system with typical presentation being fever, joint pain, malar rash, ulcer and mucocutaneous involvement occurring mostly in females [5].
PV is an autoimmune disease, affecting skin and mucous membrane, mediated by circulating autoantibodies directed against keratinocytes cell surface and is characterised by intraepithelial blisters and sores [6].
Anti-CCP is an autoantibody produced when the patient’s immune system attacks its own body. Till date anti-CCP is used as a diagnostic marker for rheumatoid arthritis but now studies are going on to establish its role in other autoimmune diseases, with and without arthritis.
The aim of this study was to assess the role of anti-CCP and CRP in patients of autoimmune skin diseases and to see their correlation with presence and absence of arthritis in these patients.
Materials and Methods
This was a case-control study which included 50 patients of autoimmune skin disease attending the Department of Dermatology from January 2013 to December 2015 as cases. Control group consisted of age and sex matched 20 normal paramedical staffs, patient’s attendants and students.
Written informed consent was taken from all the subjects before undergoing any investigation. The research protocol was conducted in accordance with the Helsinki Declaration.
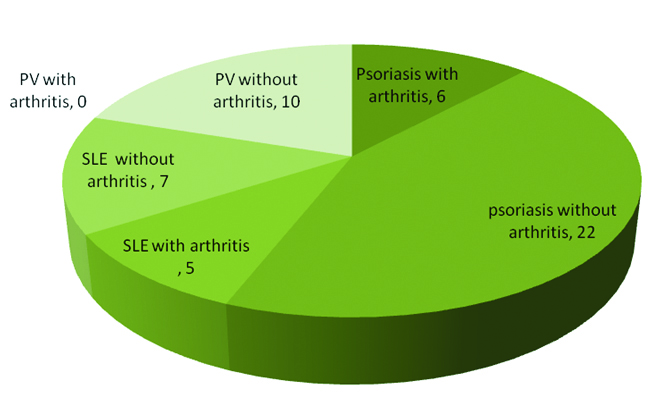
Out of 50 patients of autoimmune skin disease, 28 were patients of psoriasis, 12 of SLE and 10 of PV. These patients were further categorised into two groups based on the presence and absence of arthritis. Group I –Those associated with arthritis; Group II- Those without arthritis.
Out of 28 psoriasis patients six were associated with arthritis. Similarly five out of 12 SLE patients were associated with arthritis. None of patients with PV had arthritis.
Thus Group I consist of 11 patients of autoimmune skin disease with arthritis and Group II had the rest 39 patients of autoimmune skin disease without arthritis.
Serum CRP was estimated in all the subjects. CRP was assayed by means of particle enhanced turbidimetric immunoassay method. Principle behind the test is that latex particle coated with goat IgG anti human CRP when mixed with patients serum causes agglutination leading to change in absorbance. This change depends on concentration of CRP in patient’s serum which can be estimated by comparison with a calibrator of known CRP concentration [7]. Upto 6 mg/l was the cut-off normal serum CRP level [7].
A 10 ml of venous blood was collected under aseptic precaution in a plain vacutainer. Serum was separated and CRP estimation was done.
Test for anti-CCP was not done in our hospital. So the same sample was sent to an accredited private laboratory. Anti-CCP was assayed by means of Enzyme Linked Immunosorbent Assay (ELISA) for the detection of IgG class of autoantibody specific to cyclic citrullinated peptide in human serum or plasma [8]. Level>5 U/ml was considered positive and <5 U/ml was considered negative [9].
Statistical analysis was performed using Graph pad Prism 5.0 statistical software. Student’s unpaired t-test was applied to the result data and values obtained were expressed as mean and standard deviation. Percentage association was shown. Results of the study were discussed at 95% confidence interval. Interpretation of the test results was done according to p-value (p<0.05; significant).
Result
Of the total 50 patients of autoimmune skin disease 29 were females and 21 were males. Age of the patient and control group ranged from 18-60 years.
[Table/Fig-1] shows the distribution of patients of autoimmune skin diseases with and without arthritis. [Table/Fig-2] shows the percentage variation of anti-CCP and CRP in autoimmune skin diseases based on the presence and absence of arthritis.
Distribution of patients of autoimmune skin diseases with and without arthritis.
SLE-Systemic lupus Erythematosus
PV-Pemphigus Vulgaris
Percentage variation of anti-CCP and CRP between different autoimmune skin diseases with and without arthritis.
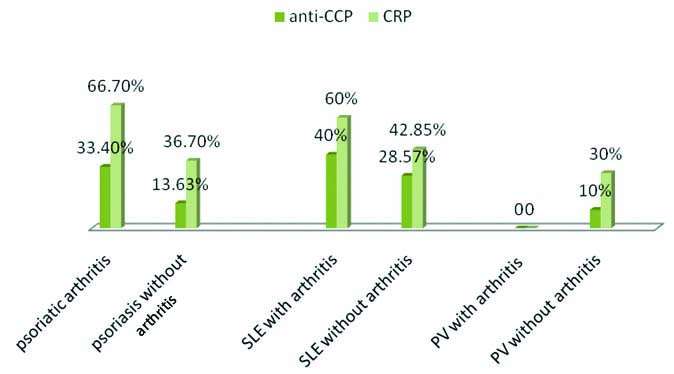
Group I comprised of 11 patients of autoimmune skin disease associated with arthritis. A total of six patients were of psoriatic arthritis and 5 patients of SLE had arthritis. CRP was raised in seven out of 11patients (63.63%) and anti-CCP was raised in four out of 11 patients with arthritis (36.37%).
Group II comprised of 39 patients of autoimmune skin disease without arthritis in which twenty two were of psoriasis, seven of SLE and 10 of PV. CRP was raised in 14 out of 39 patients (35.89%) and anti-CCP was raised in five out of 39 patients (12.82%) without arthritis.
Mean serum CRP (mg/l) in group I was 21.11±15.51 and in Group II was 13.14±12.27 with p=0.07 (not significant). Mean serum anti-CCP (U/ml) in Group I was 15.78±13.94 and in Group II was 7.56±7.68 with p=0.01(significant) as shown in [Table/Fig-3].
Comparison of levels of anti-CCP and CRP with presence and absence of arthritis.
| Group I(with arthritis, n=11) | Group II(without arthritis, n=39) | p-value |
|---|
| Anti-CCP(U/ml) | 15.78±13.94 | 7.56±7.68 | 0.01 |
| CRP(mg/l) | 21.11±15.51 | 13.14±12.27 | 0.07 |
All patients in control group had normal anti-CCP level. Mean serum anti-CCP (U/ml) was 4.36±0.68. CRP was normal in 17 subjects out of 20. Only three had mildly elevated CRP level. Mean serum CRP (mg/L) was 5.86±1.73.
Discussion
During inflammation of joints secondary to any immune mediated disease, there is release of enzyme called Peptidylarginase Deiminase (PADs) which catalyses the conversion of proteins (fibrin, fibrinogen, vimentin found in synovium of inflamed joint) arginine residue to citrulline in the presence of calcium. This process is called citrullination or deimination [10]. It is referred to as deimination because the enzyme PADs replace the primary ketimine group (=NH) by a ketone group (=O). Arginine being positively charged at neutral pH is replaced by citrulline that has no net charge. This leads to increased hydrophobicity of protein that causes defective protein folding affecting its structure and function. Due to change in shape, these proteins are recognised by immune system as antigen, thus leading to antibody formation [11].
Few data are available related to the prevalence of arthritis in various autoimmune skin diseases. A study in Sweden has shown 30% prevalence of arthritis in psoriasis [12]. Another study has shown a prevalence of 6-42% [13]. In our study six out of 28 patients had arthritis i.e. 21.42%.
Prevalence of arthritis in SLE is 48 % [14,15]. In our study five out of 12 SLE patients had arthritis (41.66%).
In our study we found that 20% and 42% of patients of autoimmune skin disease had raised anti-CCP and CRP respectively. When these patients were categorized in two groups; i.e., with arthritis and without arthritis, we found a higher level of anti-CCP and CRP in Group I as compared to Group II. But this increase was significant only for anti-CCP, not for CRP. This finding was consistent with the finding of Grover C et al., [16]. Other studies like that of Isha Jain VK and Laal H and Vadakayil AR et al., has shown raised CRP levels in patients of psoriasis and psoriatic arthritis but none have shown any significant difference in CRP levels between psoriasis and psoriatic arthritis [17,18]. Our study also does not show any significant difference in levels between Group I and Group II.
Studies have shown significantly raised anti-CCP in psoriatic arthritis as compared to psoriasis which was in accordance with our findings [19,20]. Very few studies are done on the association of SLE with anti-CCP or association of anti-CCP with other autoimmune skin diseases in common. Grover C et al. in his study has shown raised anti-CCP in autoimmune skin diseases and the rise was more significant if associated with arthritis [16].
CRP was positive in three (30%), and anti-CCP was positive in one (10%) out of 10 patients of PV. None of these were associated with arthritis. So, we were unable to study the difference in level of serum anti-CCP and CRP based on the presence and absence of arthritis in these patients.
Grover C et al., in his study has shown CRP positive in (22.22%) and anti-CCP in none of the patients of immunobullous disease [16]. His study also didn’t enroll any subject of immunobullous disease associated with arthritis.
There is certain limitation of this study. The study needs to be more extensive taking larger number of subjects and should individually focus on different forms of autoimmune skin diseases with and without arthritis.
Conclusion
From our study it is concluded that anti-CCP and CRP both are raised in patients of autoimmune skin disease, however association with arthritis is significant only for anti-CCP. Anti-CCP till date has been known to be a valuable marker for Rheumatoid Arthritis (RA) only, however this study has shown its association with other disorders also and its significance in other forms of arthritis as well.
[1]. Puszczewicz M, Iwaszkiewicz C, Role of anti-citrullinated protein antibodies in diagnosis and prognosis of rheumatoid arthritisArch Med Sci 2011 7(2):189-94. [Google Scholar]
[2]. Mantovani A, Garlanda C, Doni A, Bottazzi B, Pentraxins in innate immunity: from C-reactive protein to the long pentraxin PTX3Journal of Clinical Immunology 2008 28(1):01-13. [Google Scholar]
[3]. National Psoriasis Foundation: moderate to severe psoriasis and psoriatic arthritis: biologic drugs 2015 March [Google Scholar]
[4]. Boehringer Ingelheim’s Investigational Biologic Cleared Skin Better than Ustekinumab in Head-to-Head 2015 March20GermanyPhase II Psoriasis Study SAN FRANCISCO Calif.- Ingelheim [Google Scholar]
[5]. Bartels CM, Muller D, Systemic Lupus Erythematosus (SLE):Drug & diseases, Rheumatology 2016 [Google Scholar]
[6]. Ahmed AR, Moy R, Death in pemphigusJ Am Acad Dermatol 1982 7(2):221-28. [Google Scholar]
[7]. ACCUCARE CRP-turbilatex Latex turbidity, Labcare, Quantitative Determination of C-reactive protein [Google Scholar]
[8]. Axis-Shield Anti-CCP, FCCP600, ELISA, Axis-Shield Diagnostics Limited [Google Scholar]
[9]. Popescu C, Zofotă S, Bojincă V, Ionescu R, Anti-cyclic citrullinated peptide antibodies in psoriatic arthritis—cross-sectional study and literature reviewJ Med Life 2013 6(4):376-82. [Google Scholar]
[10]. Wang S, Wang Y, Peptidylarginine deiminases in citrullination, gene regulation, health and pathogenesisBiochim Biophys Acta 2013 1829(10):1126-35. [Google Scholar]
[11]. Coenen D, Verschueren P, Westhovens R, Bossuyt X, Technical and diagnostic performance of 6 assays for the measurement of citrullinated protein/peptide antibodies in the diagnosis of rheumatoid arthritisClin Chem 2007 53(3):498-504. [Google Scholar]
[12]. Zachariae H, Prevalence of joint disease in patients with psoriasis: implications for therapyAm J Clin Dermatol 2003 4:441-47. [Google Scholar]
[13]. Gladman DD, Antoni C, Mease P, Clegg DO, Nash P, Psoriatic arthritis: epidemiology, clinical features, course, and outcomeAnn Rheum Dis 2005 64(Suppl II):ii14-ii17. [Google Scholar]
[14]. Cronin ME, Musculoskeletal manifestations of systemic lupus erythematosusRheum Dis Clin North Am 1988 14(1):99-116. [Google Scholar]
[15]. Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, Morbidity and mortality in systemic lupus erythematosus during a 10-year period: A comparison of early and late manifestations in a cohort of 1,000 patientsMedicine (Baltimore) 2003 82(5):299-308. [Google Scholar]
[16]. Grover C, Kashyap B, Daulatabad D, Dhawan A, Kaur IR, Significance of anti-cyclic citrullinated peptide autoantibodies in immune-mediated inflammatory skin disorders with and without arthritisIndian J Dermatol 2016 61(5):510-14. [Google Scholar]
[17]. Isha Jain VK, Lal H, C-Reactive protein and uric acid levels in patients with psoriasisInd J Clin Biochem 2011 26(3):309-11. [Google Scholar]
[18]. Vadakayil AR, Dandekeri S, Kambil SM, Ali NM, Role of C-reactive protein as a marker of disease severity and cardiovascular risk in patients with psoriasisIndian Dermatol Online J 2015 6(5):322-25. [Google Scholar]
[19]. Abdel Fattah NSA, Hassan HE, Galal ZA, El Okda ESE, Assessment of anti-cyclic citrullinated peptide in psoriatic arthritisBMC Research Notes 2009 2:44 [Google Scholar]
[20]. Alenius GM, Berglin E¨a¨, Dahlqvist SR, Antibodies against Cyclic Citrullinated Peptide (CCP) in psoriatic patients with or without joint inflammationAnn Rheum Dis 2006 65:398-400. [Google Scholar]