New Vision for Improving the Oral Health Education of Visually Impaired Children- A Non Randomized Control Trial
Arpan Debnath1, B.K. Srivastava2, Punith Shetty3, Shruthi Eshwar4
1 Postgraduate Student, Department of Public Health Dentistry, K.L.E Society’s Institute of Dental Sciences, Bengaluru, Karnataka, India.
2 Head, Department of Public Health Dentistry, K.L.E Society’s Institute of Dental Sciences, Bengaluru, Karnataka, India.
3 Senior Lecturer, Department of Public Health Dentistry, Krishnadevaraya College of Dental Sciences, Bengaluru, Karnataka, India.
4 Reader, Department of Public Health Dentistry, K.L.E Society’s Institute of Dental Sciences, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Punith Shetty, International Airport Road, Hunsamaranahalli, Bengaluru-562157, Karnataka, India.
E-mail: punithshetty13@gmail.com
Introduction
Visually impaired people have poorer oral hygiene when compared to others. Therefore, there is a necessity for individual training by making awareness in oral care and plaque control so as to improve their oral hygiene.
Aim
The aim of the present study was to assess the effectiveness of oral health innovative educative method among visually impaired children of Bengaluru city of India.
Materials and Methods
A non-randomized control trial was conducted among 40 visually impaired individuals attending special school for blind. The study was conducted for a duration of six months. Baseline data regarding oral health knowledge, attitude and practices was obtained through a questionnaire in Braille and oral plaque assessment was done using Silness and Loe plaque index (1964). Music based brushing technique, cast models and an oral health education talk and booklet in Braille was delivered stressing on importance of oral health. The results of Knowledge, Attitude and Practices (KAP) before and after health education were analysed using Chi-square test with SPSS version 22.0.
Results
The overall KAP was lower in the preintervention period among the visually impaired children with mean score of 6.98 while after the modified oral health education session, it was increased to a mean score of 14.68 which was statistically significant at p<0.001. There was a significant change in the oral plaque scores with 80% of the children having fair scores in the preintervention period to 30% in the postintervention period.
Conclusion
This oral health education module showed good results which can be implemented to effectively increase the awareness about dental health.
Blindness, Dental plaque, Oral hygiene
Introduction
Dentist’s skills and knowledge often presents a unique challenge in treating special and medically compromised patients. Persons with disability means a person suffering from any of the conditions relating to autism, cerebral palsy, mental retardation or a combination of any two or more of such conditions and a person suffering from severe multiple disability [1]. As per Census 2011, in India, out of the 111 Cr population, about 2.68 Cr persons are ‘disabled’ which is 2.21% of the total population [1]. Among all disabled, sensory impairment accounts for the highest disability at 49% in India. Blindness is acknowledged as an significant public health problem in India. The number of blind persons presently in India has been estimated to be 18.7 million and the projected number of blind persons in India would increase to 31.6 million 2020 [2]. Childhood blindness is a public health problem and this has become the priority of “Vision 2020 - the Right to Sight,” which is a global initiative for the eradication of preventable blindness. In India, 3,20,000 children (<16 years) are blind and this constitutes 1/5th of the total blindness in the world among children [3]. The most common causes for childhood blindness is Corneal Scar- (vitamin A deficiency, measles, trauma) followed by cataract and trachoma and glaucoma [4].
Most handicapped individuals have healthy teeth and gums in the beginning. However, their poor oral health is contributed by their diet, eating pattern, medication, physical limitations, lack of cleaning habits and attitudes of parents and health providers [5]. Dental diseases are the most common and widespread diseases around the globe [6]. Poor oral health and untreated dental conditions influence the quality of life of children specially the visually impaired children [7]. Dental caries are more common among people with disability. Who have consistently poorer state of oral hygiene. Inadequate plaque removal is the main reason for higher prevalence of dental caries in disabled individuals [8]. Since the visually impaired children depend much on sound, speech and touch, to orient themselves to situations, a comprehensive oral health education delivery should be based on easy learning approaches to improve the KAP skills of visually impaired group. Health education, like general education, assesses the changes in knowledge, feelings and behaviour of individual. Generally, health education concentrates on developing health practices which are believed to bring the best possible state of well-being [9].
In recent times, the aims and objectives of a health education has been to encourage people to adopt and sustain health promoting lifestyle and practices. The need for various innovative methods of delivering oral health education should be paramount so as to accommodate new knowledge, improve skills and change attitudes in making rational decisions to solve their own problems and to achieve improved oral health. Thus, the aim of the study was to assess the effectiveness of innovative oral health education methods among visually impaired children of Bengaluru city using a close ended questionnaire and plaque Index [10].
Materials and Methods
The study is a non-randomized controlled trial which was conducted over duration of six months in KLE Institute of Dental Sciences, Bengaluru, Karnataka, India. The sample size was determined using G*Power software version 3.1.9.2. Alpha error was set at 0.05, effect size (Cohen’s d) as 0.5 and Power at 90%, the sample size was estimated to be 36, this was rounded off to 40. Visually impaired children from Snehadeep school for blind, Bengaluru, belonging to the age group 8-18 years, who were mentally sound to answer questionnaire and who can see less at 20 feet than that a person with normal vision can see at 200 feet (a visual acuity is 20/200) were included in the study [11]. The children were selected using simple random sampling technique. Children affected with mental retardation, mentally handicapped, orthopaedic defects, cerebral palsy and children without consent were excluded from the study. The Ethical consent was obtained from the Ethical review Board of the Institute, which was in accordance with the principles of the Declaration of Helsinki (1975, rev. 2000). Informed consent was obtained from the participating subjects.
Study Procedure
The children selected were subjected to Type 3 intraoral examination [12]. Dental plaque status was assessed by plaque index – Silness and Loe (1964) [10]. The questionnaire included questions of knowledge regarding dentition and oral health care, dental health behaviour (brushing frequency and other oral aids), attitude towards oral health (maintenance of teeth and importance of dentist) and knowledge regarding diet [13-15]. This was converted and delivered in Braille format which was done by Snehadeep school for blind and was validated in a pilot study with Cronbach’s alpha 0.72 at the beginning of the study. The oral health status was assessed using the plaque scores which was collected on the same day.
Intervention
Oral health education module was constructed which involved 3 methods:
A Music based brushing technique - a special brushing method with music titled “Brush Your Teeth, Spread the Smile to Change the World All Day Long” was designed to give health education to the children. The music was of 5.5 minutes duration where the emphasis was given on two times brushing and brushing in Modified Bass Technique. Change in the music was the indication for them to change the brushing surface so as to cover all teeth surfaces. Modifications and improvements were accomplished by physical as well as verbal guidance.
Dental cast models highlighting various dental diseases were prepared and demonstrated-patients were aided in exploring the oral structures. These models were used effectively as instructional aids. Various oral diseases of the oral cavity were replicated in the dental model like dental caries, gingival inflammation, attrition, abrasion, and abscess.
A health talk and health education booklet in Braille format was given to all the visually impaired children. At first, the importance of the teeth was explained. Then the general anatomy of tooth was explained. Children were taught the problems associated with their teeth because of early gum diseases and periodontal problems, detail notes on dental caries was given and impact of bad breath explained. Various health facts as well as various preventive dental treatment modalities were explained. At last, the seven golden rules for a healthy oral cavity [16] were explained:
a) Brush your teeth twice daily.
b) Floss once a day.
c) Clean your tongue daily.
d) Rinse your mouth after every meal.
e) Eat nutritious food.
f) Limit snacking between meals.
g) Visit dentist every six months.
Questionnaire was administered before the start of the study, to check for the KAP among the participants. The interventions were conducted by the primary investigator and the plaque scores were recorded by secondary investigator. The intervention was given on the first Saturday of every month for six months, the oral health education module intervention lasted for around 30 minutes. The same questionnaire was distributed after six months to assess the changes in KAP regarding oral health status and plaque scores were determined.
Statistical Analysis
The collected data on oral health awareness questionnaire and plaque status and associated variables were analysed using Chi-square-test and Wilcoxan signed test with SPSS software version 22.0.
Results
A non-randomized control trial was conducted among 40 visually impaired individuals attending special school for blind.
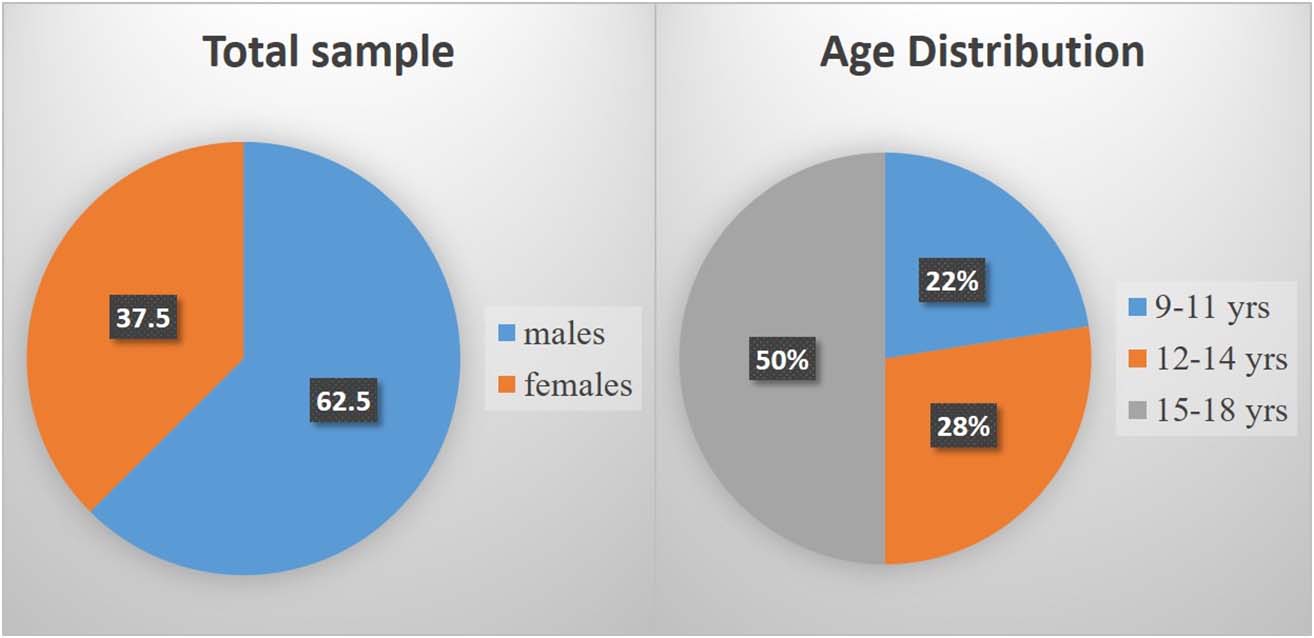
Males formed almost two third’s of the population, and the age group of 15-18 years formed nearly half of the population [Table/Fig-1]. The overall KAP was lower in the preintervention period among the visually impaired children with mean score of 6.98 after the modified oral health education session, the KAP was increased to a mean score of 14.68 with minimum score of 8 and maximum score of 16 which was statistically significant at p<0.001 [Table/Fig-2]. The KAP scores were also converted to percentages and divided into grades such as below average (< 30%), average (31%-70%) and above average (71%-100%). The number of students had increased in the above average KAP group in the after session with 95% increase while in the below average group the number of students has decreased with 4% in the after session [Table/Fig-3].
Descriptive data of total sample and age distribution of the study population.
Mean KAP score before and after health education intervention.
| Intervention | Knowledge | Attitude | Practice | KAP |
|---|
| N | Mean | N | Mean | N | Mean | Mean | p-value |
|---|
| Before | 40 | 3.18 | 40 | 1.50 | 40 | 2.30 | 6.98 | <0.001 |
| After | 40 | 8.97 | 40 | 2.81 | 40 | 2.90 | 14.68 |
* Statistically significant at p<0.05
Wilcoxon signed rank test was applied.
Mean KAP score before and after health education intervention.
| Intervention | KAP Score percentage | Total | χ2 value | p-value |
|---|
| Below average (≤30%) | Average (31%-70%) | Above average (71%-100%) |
|---|
| Before | 4 (10.0%) | 36 (90.0%) | 0 (.0%) | 40 (100.0%) | 72.421 | <0.001 |
| After | 0 (.0%) | 2 (5.0%) | 38 (95.0%) | 40 (100.0%) |
| Difference | 4% | 85.0% | 95.0% | |
* Statistically significant at p<0.05
Chi-square test was applied.
The oral hygiene of the children was assessed using plaque index before and after the intervention. The scores were categorized into good, fair and poor. Improvement was seen in the visually impaired children before and after receiving oral health education as only 5% of the children could be categorized as having good plaque scores before the intervention and this number increased to 67% after the intervention. This difference was found to be statistically significant at p<0.05 [Table/Fig-4]. Behaviour change was one of the main objectives of conducting this study, changes in daily brushing frequency was also analysed and it was found only 37.5% of the students brushed twice in the preintervention period and this increased to 92.5% after the oral health education session was held. The knowledge regarding anatomy of tooth, flossing of teeth and dietary habits also increased postintervention. These differences was also found to be statistically significant at p<0.05 [Table/Fig-5]. Thus, the study opines that oral health education of blind children using innovative methods is effective in improving their KAP towards oral health and can also lead to behaviour modification.
Difference between plaque scores before and after intervention.
| Intervention | Plaque index | Total | χ2 value | p-value |
|---|
| Good | Fair | Poor |
|---|
| Before | 2 (5.0%) | 32 (80.0%) | 6 (15.0%) | 40 (100.0%) | 34.214 | <0.001 |
| After | 27 (67.5%) | 12 (30.0%) | 1 (2.5%) | 40 (100.0%) |
| Difference | 25.0% | 20.0% | 12.5% | |
* Statistically significant at p<0.05
Chi-square test was applied.
Knowledge regarding Oral Hygiene practice before and after intervention.
| Variables | Before intervention (%) | After intervention (%) | p-value |
|---|
| Layers of tooth | 87.5 | 97.5 | < 0.005 |
| Use of floss | 10 | 92.5 | < 0.005 |
| Number of times brushing (Twice daily) | 37.5 | 92.5 | < 0.005 |
| Knowledge about sugar exposure causes caries (true) | 55 | 82.5 | < 0.005 |
| Knowledge about sticky and slow dissolving sugar causes caries (yes) | 17.5 | 97.5 | < 0.005 |
* Statistically significant at p<0.05
Chi-square test was applied.
Discussion
Subjects with disabilities are prone to have higher incidence of dental caries and more problems in accessing dental care. Majority of them do not know the basic preventive aspects regarding oral health. Preventive and oral health education approaches are more effective than the standard dental care when it comes to visually impaired children. A special protocol and design is essential to inculcate a good oral hygiene practice in them.
Chang S and Shih Y observed that students who were visually impaired were less aware of their dental health [17]. Poor knowledge regarding dental health was seen in the present study as well, indicating that their elementary knowledge about the oral cavity was poor. It was found that at the cognitive level also, there was a lack in knowledge. A person suffering from visual disability, despite being in the society, cannot receive the visual social stimuli; so, most of the children were less perturbed about their oral health. In the present study, most of the visually impaired children were unaware of the term “Floss”. This can be explained by their poor oral health knowledge as well as their institutional background where using of floss was never taught. This finding was in accordance to study done by Chang S and Shih Y, where 40% of the sighted participants used both tooth brush as well as floss for teeth cleaning, but only 20% of the participants with visual impairments did so [17]. So, it is necessary to teach appropriate tooth flossing technique with the help of repeated motivation. Also, after the oral health education session, most of them showed a change in their behaviour. The number of children brushing twice a day increased after the intervention. This was in accordance with a study conducted by Ahmad MS et al., [14] It was seen that in this short period, the students developed the habit of brushing their teeth with Modified Bass technique with stipulated amount of toothpaste. It was in accordance to the study conducted by Nandini N, where the cognitive level of dental health knowledge as well as oral health practices was significantly increased with one to one health education to the visually impaired children [18].
It was seen in the study that knowledge about consuming sugary foods and beverages was also poor among the visually impaired children. This was in agreement with the study conducted by Vigild M et al., who reported a high consumption of sugar containing products among the blind children [19]. In our study, the postintervention period showed a significant increase in the knowledge about sugar consumption with 97.5% of the children understanding the fact that sweets that are sticky and which dissolves slowly are the major etiological factors for dental caries causation and that the amount of sugar intake is not so important as compared to the frequency of sugar consumption. The removal of plaque and debris from the teeth is an ability that can be mastered only when individuals have the skill to manipulate the toothbrush and understand the objectives of these activities [20]. In the present study, there was fair plaque scores (80%) among the visually impaired individuals in the preintervention period which was in accordance to study done by Sujal P [21]. The probable reasons for poor oral hygiene in these visually impaired individuals could be due to low power of concentration or lack of motor skills or problem in communication/understanding of instructions and poor co-operation leading to difficulty in learning and adaptation of the oral hygiene practices. But after the stepwise implementation of the health education module, the fair oral plaque scores reduced to 30% among the visually impaired children showing the effectiveness of the motivation element within the programme.
This oral health education module for individuals who are blind can act as a template in planning and improving the oral hygiene of these individuals so that the disabled individuals will not feel left out in this fast moving world in terms of health.
Limitation
The limitations of the study was that the number of individuals selected for the study were from the same institute and the total number of participants was small.
Recommendation
To improve the oral hygiene status of individuals with disabilities is a daunting task, but it can be achieved if even the parents or guardians are given suitable health education. So, the differing needs of these special children and their caregivers needs to be addressed in future. This study only provides an insight into the increase in awareness and increase in oral health maintenance after a comprehensive oral health programme in a relatively small sample. So, a mass study is required if any other factors are required to be modified for the improvement of oral health education among visually impaired children.
Conclusion
This modified dental health education module with its three pillars based on a specially designed educative module comprising of tactile dental models, a specially designed music based brushing technique and health education booklet in Braille will definitely improve knowledge and attitude towards oral health among these visually impaired children.
* Statistically significant at p<0.05
Wilcoxon signed rank test was applied.
* Statistically significant at p<0.05
Chi-square test was applied.
* Statistically significant at p<0.05
Chi-square test was applied.
* Statistically significant at p<0.05
Chi-square test was applied.
[1]. Ministry of Statistics and Programme ImplementationNational Sample Survey Organisation. Disabled Persons in India. Report No. 485 (58/26/1)New DelhiGovernment of India 2016 [Google Scholar]
[2]. Sagar B, Epidemiological study of prevalence and causes of visual disability in a rural communityJ Indian Academy of Geriatrics 2011 7:01-05. [Google Scholar]
[3]. Murthy S, Gupta S K, Bachani D, Jose R, John N, Current estimates of blindness in IndiaBr J Ophthalmol 2005 89(3):257-60. [Google Scholar]
[4]. Murthy G, Gupta SK, John N, Vashist P, Current status of cataract blindness and vision 2020. The right to sight initiative in IndiaIndian J Ophthalmol 2008 56:489-94. [Google Scholar]
[5]. Kamatchy KRJ, Joseph J, Krishnan CGA, Dental caries prevalence and experience among the group of institutionalized hearing impaired individuals in PondicherryIndian Journal of Dental Research 2003 14:29-32. [Google Scholar]
[6]. Priya M, Devdas K, Amarlal D, Venkatachalapathy A, Oral health attitudes, knowledge and practice among school children in ChennaiJ Education and Ethics in Dentistry 2013 3(1):26-32. [Google Scholar]
[7]. “World Blindness Overview.”Himalayan Cataract ProjectAccessed on 7 January 2016www.cureblindness.org [Google Scholar]
[8]. Mann J, Wolnerman JS, Lavie G, Carlin Y, Garfunkel AA, Periodontal treatment needs and oral hygiene for institutionalized individuals with handicapping conditionsSpec Care Dentist 1984 4:173-76. [Google Scholar]
[9]. Kiger A, Teaching for health 2004 3rd EditionEdinburgChurchill Livingstone:8 [Google Scholar]
[10]. Loe H, The gingival index, the plaque index and the retention index systemJ Periodontal 1967 38:610-16. [Google Scholar]
[11]. Parveen KM, Vinay PP, Rohatqi J, Dhaliwal U, Are current guidelines for categorization of visually impairment in India appropriate?Indian J Ophthalmol 2009 57(6):423-26. [Google Scholar]
[12]. Jain M, Bharadwaj S, Singh K, Chopra D, Prabhu D, Kulkarni S, Oral health status and treatment need among institutionalised hearing-impaired and blind children and young adults in Udaipur, India. A comparative studyOral Health Dent Manag 2013 12(1):41-49. [Google Scholar]
[13]. Menacker SJ, Batshaw ML, Batshaw ML, Vision: Our window to the worldChildren with Disabilities 2000 4th edBaltimore, MDPaul H Brookes:211-39. [Google Scholar]
[14]. Ahmad MS, Jindal MK, Khan S, Oral health knowledge, practice, oral hygiene status and dental caries prevalence among visually impaired students in residential institute of AligarhJ of Dent and Oral Hygiene 2009 1(2):022-26. [Google Scholar]
[15]. J Sharda A, Shetty S, A comparative study of oral health knowledge, attitude and behavior of first and final year dental students of Udaipur city, RajasthanJ Oral Health Commu Dent 2008 2(3):46-54. [Google Scholar]
[16]. Health centre for oral health strategyEarly childhood Oral Health Guidelines for Child Health Professionals 2014 July3rd Edition [Google Scholar]
[17]. Chang S, Shih Y, Knowledge of dental health and oral hygiene practices of Taiwanese visually impaired and sighted studentsJVIB 2004 98(5):11-19. [Google Scholar]
[18]. Nandini N, New insights into improving the oral health of visually impaired childrenJ Indian Soc Pedod Prev Dent 2003 21(4):142-43. [Google Scholar]
[19]. Vigild M, Petersen PE, Hadi R, Oral health behaviour of 12-year-old children in KuwaitInternational Journal of Paediatric Dentistry 1999 9:23-29. [Google Scholar]
[20]. Snyder JR, Knopp JJ, Jordan WA, Dental problems of non institutionalized mentally retarded childrenNorthwest Dent 1960 44:123-26. [Google Scholar]
[21]. Parkar S, Patel N, Zinzuwadia H, Dental health status of visually impaired individuals attending special school for blind in Ahmedabad city, IndiaIndian J Oral Sci 2014 5:73-77. [Google Scholar]