A Rare Case of Primary Calcific Pleural Tuberculosis – A Case Report
G Sahana1, Vishak Acharya2, Santosh Rai3, Nishanth Baliga4
1 Senior Resident, Department of Internal Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
2 Professor, Department of Pulmonary Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
3 Professor, Department of Radiodiagnosis, Kasturba Medical College, Mangalore, Karnataka, India.
4 Senior Resident, Department of Anaesthesiology, Kasturba Medical College, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vishak Acharya, Professor, Department of Pulmonary Medicine, Kasturba Medical College, Lighthouse Hill Road, Mangalore-575001, Karnataka, India.
E-mail: achvish@gmail.com
Tuberculosis is a highly prevalent disease in India. It has a myriad of presentations. Usually pleural tuberculosis occur secondary to pulmonary tuberculosis which can manifest as pleural effusion leading to pleural calcification. Primary pleural calcification due to tuberculosis is an extremely rare manifestation of active tuberculosis. We present a case of a 21-year-old female presenting with fever, cough, weight loss and loss of appetite who was diagnosed to have pleural calcification due to primary tuberculosis. We highlight the need to keep primary pleural tuberculosis in mind with above symptoms suggestive of active tuberculosis even when there is no underlying lung pathology.
Atypical, Calcification, Extrapulmonary
Case Report
A 21-year-old female presented to the Department of Pulmonary Medicine with complaint of fever of one month duration. Patient also gave history of cough with minimal expectoration. She had dull aching chest pain since two weeks. She also gave a history of decreased appetite and weight loss of 3 kg in one month. Patient had no history of tuberculosis, pleural aspirations or chest trauma in the past. No history of contact with tuberculosis or family history of tuberculosis was noted.
On examination, patient had pallor with stable vitals. Patient had reduced chest movements in the right hemithorax with lung volume loss including tracheal and mediastinal shift. Percussion revealed dull note over the right hemithorax. Breath sounds were diminished over the entire right hemithorax. Rest of the systemic examinations was within normal limits.
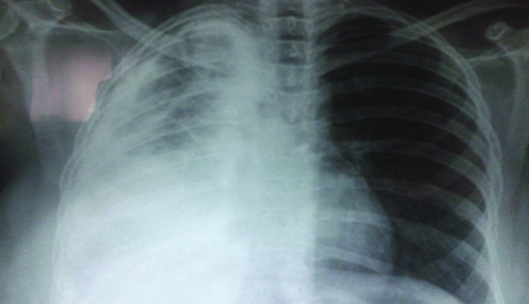
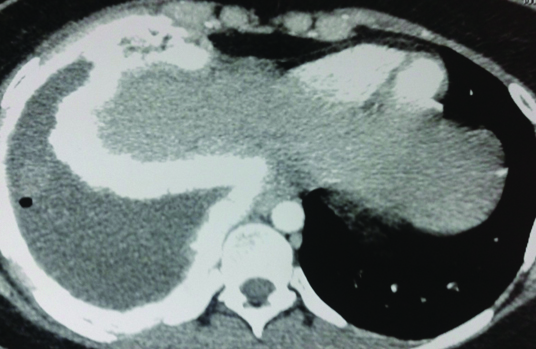
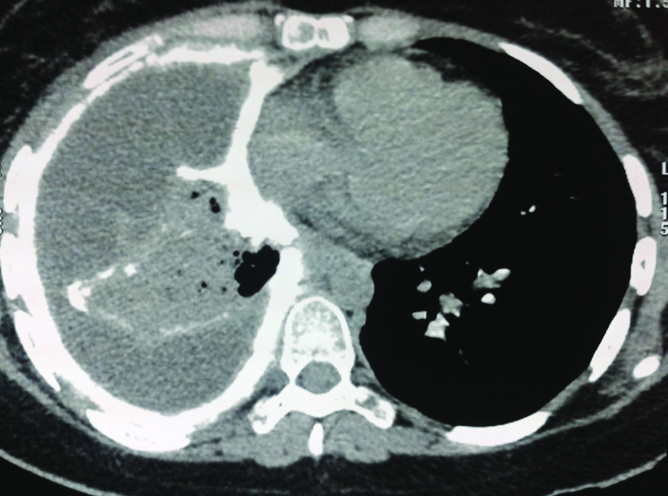
Laboratory investigations showed, Hb-9.2 gm%, Total WBC count-6800 cells/cumm, ESR-64 mm, Serum calcium-9.6 mg/dl. Peripheral smear showed microcytic hypochromic blood picture. Two sputum samples for Acid Fast Bacilli (AFB) stain were negative. Sputum culture showed no growth. Chest X-ray showed right sided lung volume loss with diffuse pleural calcification [Table/Fig-1]. HIV was negative. CT chest revealed extensive pleural fibrosis and calcification causing underlying parenchymal atelectasis [Table/Fig-2,3].
Chest X-ray showing right sided lung volume loss.
CT chest revealed extensive calcification of the right pleura with lung volume loss.
CT chest shows atelectasis and consolidation in right parenchyma probably secondary to compression due to pleural fibrosis as bronchoscopy and lavage were negative for AFB stain and cultures ruling out parenchymal involvement.

Pleural fluid analysis showed 100 cells all of which were lymphocytes, fluid glucose was 50 mg/dl, fluid proteins were 5.8 mg/dl, fluid LDH was 570 IU/l, suggestive of exudative type of effusion. Staining for AFB was negative. Pleural fluid adenosine deaminase level was elevated i.e., 90 IU/l.
Fluid obtained from bronchoscopic lavage was negative for AFB stain. Lavage fluid culture showed no growth. It was negative for malignant cytology. CT guided FNAC was attempted but could not be done due to calcific pleura. Patient was initiated on standard four drug Antitubercular Treatment (ATT) i.e., Isoniazid, Rifampicin, Ethambutol and Pyrazinamide. At the end of six months of ATT, patient’s symptoms subsided and she gained four kilograms of weight. However, radiological changes persisted after six months of ATT [Table/Fig-4].
CT scan after six months of antitubercular treatment still showing pleural calcification.
Discussion
Pleural tuberculosis is the most common presentation of extrapulmonary tuberculosis and the most common cause of pleural effusion worldwide [1,2]. Involvement of the pleura accounts for approximately 20% of the extrapulmonary cases. Pleural effusion is a very common manifestation. The collection of fluid in the pleural space represents hypersensitivity response to mycobacterial antigens. Tuberculous empyema is a less common complication of tuberculosis; it is usually due to rupture of a cavity with spillage of large number of organisms into the pleural space. Long standing empyema results in severe pleural fibrosis and then calcification [3]. IL-1 has an essential role in T-cell activation and is considered a proinflammatory cytokine [3]. It is a strong immune adjuvant and contributes to the stimulation of non specific host responses besides promoting wound healing [4]. It enhances blood flow and the induction of chemoattractants, which brings to the injury sites the key inflammatory cells. Patients with tuberculous pleuritis who develop chronic pleural thickening have significantly higher IL-1 levels [4].
The differential diagnosis in a patient with extensive pleural calcification are hemothorax, malignant mesothelioma secondary to exposure to asbestos, pleural lymphoma, pleural metastasis and rarely primary pleural calcification due to tuberculosis [5]. In our case hemothorax was unlikely as there was no history of trauma and CT did not show any evidence of parenchymal contusion. Mesothelioma is a highly malignant condition which is secondary to asbestos exposure in 40%-80% of patients and presents after fifth decade [6]. CT shows irregular nodular internal margin of the tumour with local infiltration [6]. The young age of our patient and lack of asbestos exposure makes the diagnosis of mesothelioma highly unlikely. Infiltration of the pleura manifests as pleural effusion which is the first manifestation of pleural metastasis which later can calcify. Patient can have lung nodules or rib erosions. Pleural metastasis arises from lung in 40% of cases, carcinoma breast in 20% of cases, 10% lymphoma and 30% from other sites.
As there was no evidence of pleural nodules along with rib erosions the probability of metastatic lesion was excluded as well as she did not have any features of primary malignancy.
Pleural lymphoma occurs both in Hodgkin and Non-Hodgkins lymphoma. In our patient there were no systemic lymph nodes and no evidence of lymphoma, the possibility of pleural lymphoma as a diagnosis was ruled out. Hence, a preliminary diagnosis, by exclusion, of primary pleural tuberculosis was made as there were no features of primary pulmonary involvement. Pleural fluid ADA levels, good response of the patient to ATT confirmed the diagnosis.
Conclusion
Pleural calcification presenting as primary active tuberculosis is a rare presentation. This case is discussed here to emphasize on the fact that a differential diagnosis of active tuberculosis must be included by the pulmonary physicians in patients with above symptoms with pleural calcification without any underlying lung pathology.
[1]. Lazarus AA, McKay S, Gilbert R, Pleural tuberculosisDis Mon 2007 53(1):16-21. [Google Scholar]
[2]. Wong PC, Management of tuberculous pleuritis: can we do better?Respirology 2005 10(2):144-48. [Google Scholar]
[3]. Sargent EN, Jacobson G, Gordonson JS, Pleural plaques: a signpost of asbestos dust inhalationSemin Roentgenol 1977 12(4):287-97. [Google Scholar]
[4]. Berger HW, Mejia E, Tuberculous pleurisyChest 1973 63(1):88-92. [Google Scholar]
[5]. Ariyurek OM, Cil BE, Atypical presentation of pleural tuberculosis CT findingsBr J Radiol 2000 73:209-10. [Google Scholar]
[6]. Wang ZJ, Reddy GP, Gotway MB, Higgins CB, Jablons DM, Ramaswamy M, Malignant pleural mesothelioma: evaluation with CT, MR imaging, and PETRadio Graphics 2004 24(1):105-19. [Google Scholar]