Case Report
A term male baby born at 38 weeks gestation to a 26-year-old primi gravida mother by cesarean section was admitted on fifth day of life with seizures and jaundice. Antenatal period was normal with no history of fever or rupture of membranes. Baby was vigorous at birth, weighed 2800 grams and was breastfed. Bilirubin on third day of life was 16.4 mg/dL and baby received phototherapy. Baby had an episode of seizures on fourth day of life, controlled with phenobarbitone and was referred to our unit.
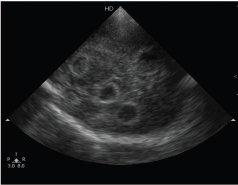
At admission, baby was febrile (101.90F), deeply icteric, sick looking and anterior fontanelle was full. Laboratory investigations showed haemoglobin of 12.5 gm/dL, leucopenia (WBC: 3200/mm3), thrombocytopenia (platelets: 1.1 lakhs/mm3) and positive septic screen (CRP: 65.4 mg/l). Bilirubin was 24.6 mg/dL with direct fraction of 1.2 mg/dL and there was evidence of haemolysis due to blood group incompatibility (baby’s group: B+; mother’s group: O+; reticulocyte count 12%; direct Coombs test positive). Baby was given intensive phototherapy, antibiotics (cefotaxime, amikacin) and ionotropic support. Head ultrasound at admission showed multiple cerebral abscesses in bilateral frontal and parietal lobes [Table/Fig-1]. Cerebrospinal Fluid (CSF) was turbid and showed 720 cells (neutrophils 90%; lymphocytes 10%), proteins 382 mg/dL and glucose 10 mg/dL (blood glucose: 64 mg/dL). Gram-stain showed Gram-negative intracellular diplococci.
Ultrasound brain at admission showing multiple cerebral abscesses
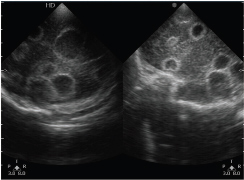
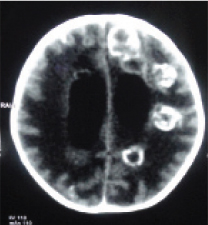
Double volume exchange transfusion was done at four hours after admission with fresh O+ whole blood. Baby had six episodes of seizures, controlled with phenobarbitone and phenytoin. Blood culture was negative. CSF culture grew N. meningitidis B which was sensitive to ceftriaxone, cefotaxime, meropenem and penicillin and resistant to ciprofloxacin. CSF analysis repeated after 48 hours showed 280 cells (neutrophils 80%; lymphocytes 20%), proteins 146 mg/dL and glucose 34 mg/dL. Serial head ultrasound scans (done twice weekly) showed multiple cerebral abscesses and mild ventricular dilatation [Table/Fig-2]. CT scan of brain done at three weeks of age showed mild hydrocephalus and few abscesses [Table/Fig-3]. Neurosurgeon’s consultation was taken and no surgical intervention was required till three weeks of age. Repeat cultures (blood and CSF) were sterile and baby received antibiotics (penicillin, cefotaxime) for three weeks. Head circumference remained static measuring 34 cm at discharge.
Ultrasound brain showing increase in number of abscesses.
CT scan brain at three weeks showing mild hydrocephalus and cerebral abscesses.
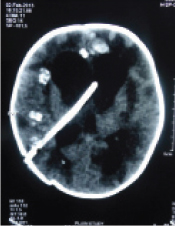
Unfortunately, mother and her family members were not screened for N. meningitidis before rifampicin prophylaxis was given. CT scan of brain repeated at five weeks of age showed hydrocephalus and a VP shunt was placed [Table/Fig-4]. Child is 18 months of age now, weighed 10.9 kg with height of 79 cm. Child has motor delay (truncal weakness and walking with support) without any recurrence of seizures. Child’s vision and hearing were normal.
CT scan brain done after placement of VP shunt.
Discussion
Neisseria meningitidis is a Gram-negative, aerobic, encapsulated intracellular diplococcus primarily transmitted by close contact with respiratory secretions but can colonize maternal genital tract leading to intrauterine infections. N. meningitidis causes significant morbidity and mortality in children but is uncommon in neonates, possibly due to transplacental transmission of maternal antibodies [1]. The incidence of neonatal meningococcal infection is estimated to be 2- 9/100,000 newborn infants in the developed world [1-4].
Both sporadic infections and wide spread epidemics of N. meningitidis were reported [5-8]. The route of transmission could be intrauterine or acquired during perinatal or postnatal period and is often difficult to ascertain [3,9-12].
Literature search of Pubmed, EMBASE, MEDLINE and Google scholar was done using the words: neonate, sepsis, N. meningitidis and meningitis. WHO bulletins and cross references of all articles were reviewed. Infants < 30 days of age and those reported as newborn or neonate were included in the review. Early and late onset infections were defined as development of symptoms during first 7 days of life and between 8 to 30 days of life respectively.
In our literature review, though we found 127 reported cases of infection (from 55 articles) with N. meningitidis in the neonatal period, we believe it may be an underestimate of the true burden of this infection [Table/Fig-5] [1-55]. Invasive meningococcal disease can have a fulminant course with fatality rates of 5%-20%. Infection was early in onset in 17.9% of cases (n=23 cases, from 16 citations) with mortality of 34.8% [1,2,5,6,10-14,17,24,30,35,43,46,51]. Two neonates in early onset group developed hydrocephalus [13,36]. Serogroups were reported in 13 cases: serogroup B being the most common with five cases, serogroup A-2 cases, serogroup C-3 cases, serogroup W135-2 cases and one case of serogroup Y.
Characteristics of neonates with meningitis caused by Neisseria meningitides [1-55].
| Author | Year | No. of cases | Age in days | Group | Complications | Outcome |
|---|
| Koplik H [13] | 1916 | 1 | 3 | ND | Hydrocephalus | Survived |
| Barron M [14] | 1916 | 1 | Newborn* | ND | - | Unknown |
| Miller DJM [15] | 1917 | 1 | 14 | ND | | Died |
| White TW [16] | 1917 | 1 | 29 | ND | - | Survived |
| Root JH [17] | 1921 | 1 | Newborn* | ND | | Died |
| Cooke JV [18] | 1922 | 1 | 17 | ND | | Died |
| Neal JB [19] | 1927 | 2 | 21, 21 | ND | | Both died |
| McLean S [20] | 1928 | 1 | 23 | ND | - | Unknown |
| Brown A [21] | 1933 | 1 | 22 | ND | - | Survived |
| Ravid JM [22] | 1935 | 1 | 27 | ND | - | Unknown |
| Garrow DH [23] | 1951 | 1 | 10 | ND | - | Died |
| Carmona EM[24] | 1953 | 2 | 2, 4 | ND, ND | - | Survived |
| Smith ES [25] | 1954 | 1 | 30 | ND | - | Unknown |
| Yung-en K [26] | 1956 | 5 | 8, 22, 25, 26, 28 | ND | | 1 Died / 4 Survived |
| Watson DG [27] | 1957 | 1 | 24 | ND | Subarachnoid haemorrhage | Died |
| Ziai M [28] | 1958 | 1 | Newborn* | ND | | Unknown |
| Stiehm ER [29] | 1966 | 1 | 7 | B | - | Survived |
| Wherle P [30] | 1976 | 1 | Newborn* | ND | | Unknown |
| Sunderland WA [9] | 1972 | 1 | 2 | C | | Died |
| Jones RN [10] | 1976 | 1 | 15 | ND | | Died |
| Manginello FP [31] | 1979 | 1 | 15 | B | - | Survived |
| Clegg HW [32] | 1980 | 1 | 25 | B | | Survived |
| Mulder CJJ [33] | 1984 | 3 | Newborn* | B, B, A# | | Unknown |
| Donald PR [34] | 1986 | 4 | Newborn* | ND | | Unknown |
| Embree J [35] | 1987 | 1 | 1 | W135 | - | Survived |
| Chugh K [36] | 1988 | 1 | 3 | A | Cerebral abscess, hydrocephalus | Died |
| Bhutta ZA [11] | 1991 | 1 | 1 | ND | | Died |
| J de Louvois [37] | 1991 | 11 | ≤28 days | ND | - | Survived |
| Ellis M [12] | 1992 | 2 | 2,3 | C, W135 | - | Survived |
| Sapan N [38] | 1993 | 1 | 20 | ND | | Died |
| Kirkpatrick M [39] | 1994 | 1 | 21 | B | Spinal dysfunction | Survived |
| Chiu CH [40] | 1994 | 2 | 28, 16 | ND,ND | - | Survived |
| Arango CA [41] | 1996 | 2 | 21, 13 | B, B | | Survived |
| Falero GMP [42] | 1999 | 1 | 25 | C | - | Survived |
| Campagne G [8] | 1999 | 11 | < 1 month | ND | - | Unknown |
| Casanova RM [43] | 2000 | 1 | 3 | B | - | Survived |
| Shepard LW [5] | 2003 | 6 | < 7 days | ND | | Unknown |
| Shepard CW [5] | 2003 | 16 | 8 - 30 days | ND | | Unknown |
| Lo WT [2] | 2003 | 1 | 1 | C | | Survived |
| Katier N [44] | 2003 | 1 | 12 | C | | Survived |
| Huang HR [6] | 2006 | 2 | 28, 28 | -/B | -, Subdural empyema | Survived |
| Falcao MC [1] | 2007 | 1 | 15 | C | | Survived |
| Arya S [3] | 2007 | 1 | 1 | A | | Died |
| Tinsa F [45] | 2008 | 1 | 20 | B | | Survived |
| Ahmareen O [4] | 2008 | 1 | 12 | B | - | Survived |
| Kurlenda J [46] | 2010 | 1 | 1 | B | - | Survived |
| Cho HK [47] | 2010 | 2 | < 1 month | ND | | Unknown |
| Fuentes AD [48] | 2011 | 3 | 9,15,15 | B,B,B | - | Survived |
| Gaschignard J [7] | 2011 | 14 | 5 - 28 | ND | | Unknown |
| Smith A [49] | 2013 | 1 | 7 | B | | Died |
| Ramsamy Y [50] | 2013 | 1 | 21 | W135 | Subdural empyema, hydrocephalus | Survived |
| Bosman M [51] | 2013 | 1 | 3 | Y | - | Survived |
| Shah S [52] | 2013 | 1 | 12 | B | | Died |
| Kumar D [53] | 2014 | 1 | 9 | ND | - | Survived |
| Devi U [54] | 2014 | 1 | 14 | Y | - | Survived |
| Kiray Bas E [55] | 2014 | 1 | 10 | ND | | Died |
| Present report | 1 | 5 | B | Cerebral abscesses, hydrocephalus | Survived |
Newborn: age not specified; ND: not done, Unclusterable or not disclosed early neonatal period
Serotypes A, B
In 2003, Lo WT et al published a review on early-onset meningococcal infection and reported a mortality rate of 50% [2]. In 2014, two cases of uncomplicated late onset meningococcal meningitis were reported from India [53,54]. In the same year, Kiray Bas E et al., reported a fatal case of meningococcal infection in a 10 day old neonate and reviewed the literature [55]. There are few published case reports of neonatal meningococcal meningitis complicated by subdural empyema, cerebral abscess and hydrocephalus [6,13,36,50].
Chugh K et al., reported a case of meningococcal meningitis in a three-day-old neonate which had complications of cerebral abscess and hydrocephalus at three weeks of age [36]. We did not find any other case reports of multiple cerebral abscesses presenting in the neonatal period.
The possible mode of transmission of infection in this patient is either intrauterine or perinatal, because of development of cerebral abscesses by the fifth day of life. Unfortunately, neither were we able to obtain a culture of the placenta or high vaginal swabs nor screen the health care personnel of the referral hospital. In this patient, there was evidence of motor delay without vision or hearing impairment or recurrence of seizures. Despite prompt diagnosis at admission and treatment, baby developed hydrocephalus requiring a VP shunt.
Conclusion
Meninogoccal meningitis should be suspected in neonates who present with sepsis and seizures even in the absence of rash. Establishing the aetiological diagnosis and identifying cerebral abscesses early was vital for treating meningitis and the associated complication of hydrocephalus. To the best of our knowledge, this is the youngest reported case of neonatal meningococcal meningitis with multiple cerebral abscesses.
*Newborn: age not specified; ND: not done, Unclusterable or not disclosed early neonatal period
#Serotypes A, B
[1]. Falcao MC, Andrade SB, Ceccon ME, Costa Vaz FA, Neonatal sepsis and meningitis caused by Neisseria meningitidis: a case reportRev Inst Med Trop S Paolo 2007 49(3):191-94. [Google Scholar]
[2]. Lo WT, Yuh US, Wang CC, Early onset neonatal infection with Neisseria meningitidis serogroup C: case report and literature reviewEur J Pediatr 2003 162(11):785-87. [Google Scholar]
[3]. Arya S, Nair D, Harish Chellani H, Deb M, Hasan AS, Gaurav J, Molecular evidence suggestive of intrauterine transmission of Neisseria meningitidis serogroup A from mother to infantPediatr Infect Dis J 2007 2(1):45-50. [Google Scholar]
[4]. Ahmareen O, Donnell SO, Satas S, Cafferkey M, Gormally S, Neonatal meningococcal meningitis: case reportArchives of Disease in Childhood 2008 93:206 [Google Scholar]
[5]. Shepard CW, Rosenstein NE, Fischer M, Neonatal meningococcal disease in the United States 1990-1999Pediatr Infect Dis J 2003 22(5):418-22. [Google Scholar]
[6]. Huang HR, Chen HL, Chu SM, Clinical spectrum of meningococcal infection in infants younger than six months of ageChang Gung Med J 2006 29(1):107-12. [Google Scholar]
[7]. Gaschignard J, Levy C, Romain O, Cohen R, Bingen E, Aujard Y, Boileau P, Neonatal bacterial meningitis:444 Cases in 7 YearsPediatr Infect Dis J 2011 30(3):212-17. [Google Scholar]
[8]. Campagne G, Schuchat A, Djibo S, Ousseini A, Cisse L, Chippaux JP, Epidemiology of bacterial meningitis in Niamey, Niger 1998-96Bulletin of the World Health Organization 1999 77(6):499-509. [Google Scholar]
[9]. Sunderland WA, Harris HH, Spence DA, Lawson HW, Meningococcemia in a newborn infant whose mother had meningococcal vaginitisJ Pediatr 1972 81:856 [Google Scholar]
[10]. Jones RN, Slepack J, Eades A, Fatal neonatal meningococcal meningitis association with maternal cervical-vaginal colonizationJAMA 1976 236(23):2652-53. [Google Scholar]
[11]. Bhutta ZA, Khan IA, Agha Z, Fatal intrauterine meningococcal infectionPediatr Infect Dis J 1991 10:868-69. [Google Scholar]
[12]. Ellis M, Weindling AM, Davidson DC, Ho N, Damjanovic V, Neonatal meningococcal conjunctivitis associated with meningococcal meningitisArch Dis Child 1992 67(10):1219-20. [Google Scholar]
[13]. Koplik H, Meningitis in the newborn and in infants under three months of ageArch Pediatr 1916 33(7):481-500. [Google Scholar]
[14]. Barron M, Meningitis in newborn and early infancyAm J Med Sci 1916 33:387-96. [Google Scholar]
[15]. Miller DJM, A case of meningococcal meningitis in the newborn with interesting unusual featuresArch Pediatr 1917 34:824-26. [Google Scholar]
[16]. White TW, Case reports of infectious meningitis developing in babies 29 and 39-day-old respectivelyArch Pediatr 1917 34:312-16. [Google Scholar]
[17]. Root JH, A case of meningococcus meningitis with obstructive hydrocephalus in the newly bornAm J Dis Child 1921 21:500-05. [Google Scholar]
[18]. Cooke JV, Bell HH, The incidence of meningitis in early infancy with a description of two cases due to unusual organismAm J Dis Child 1922 22:359-87. [Google Scholar]
[19]. Neal JB, Jackson HW, Epidemic meningitis in the first three months of lifeJAMA 1927 88:199-300. [Google Scholar]
[20]. McLean S, Caffey JP, Endemic meningococcus meningitis, clinical manifestation in infancy and in early childhoodAm J Dis Child 1928 35(3):357-87. [Google Scholar]
[21]. Brown A, Silverthrone N, Meningococcic meningitis in infancy: report of a caseJAMA 1933 101(4):272-73. [Google Scholar]
[22]. Ravid JM, Meningococcic and non meningococcic meningitis in the newborn and young infantsAm J Dis Child 1935 49:1282-98. [Google Scholar]
[23]. Garrow DH, Neonatal meningococcosisPostgraduate Med J 1951 27:358-63. [Google Scholar]
[24]. Carmona EM, Teizido JV, Two cases of meningococcal meningitis in the first week of lifeAm J Dis Child 1953 86:810 [Google Scholar]
[25]. Smith ES, Purulent meningitis in infants and children: A review of 408 casesJ Pediatrics 1954 45:425-36. [Google Scholar]
[26]. Yung-En K, Shang-Jen C, Heuch-Ying L, Purulent meningitis in the newborn. Report of 11 casesChinese Med J 1956 74:573-77. [Google Scholar]
[27]. Watson DG, Purulent neonatal meningitisJ Pediatr 1957 50:352-60. [Google Scholar]
[28]. Ziai M, Haggerty RJ, Neonatal meningitisN Eng J Med 1958 :314-20. [Google Scholar]
[29]. Stiehm ER, Damrosch DS, Neonatal meningococcal meningitis: report of a case acquired in the nurseryJ Pediatr 1966 68:654-56. [Google Scholar]
[30]. Wherle P, Cited in Fatal neonatal meningococcal meningitis association with maternal cervical-vaginal colonizationJAMA 1976 236(23):2652-53. [Google Scholar]
[31]. Manginello FP, Pascale JA, Wolfsdorf J, Klein GM, Neonatal meningococcal meningitis and meningococcemiaAm J Dis Child 1979 133:651-52. [Google Scholar]
[32]. Clegg HW, Todres ID, Moylan FM, Keim DE, Shannon DC, Fulminant neonatal meningococcemiaAm J Dis Child 1980 134(4):354-55. [Google Scholar]
[33]. Mulder CJ, Zanen HC, A study of 280 cases of neonatal meningitis in the NetherlandsJ Infect 1984 9:177-84. [Google Scholar]
[34]. Donald PR, Burger PJ, Becker WB, Pediatric meningitis in the western CapeS Afr Med J 1986 70:391-95. [Google Scholar]
[35]. Embree J, Law BJ, Williams T, Edye-Mazowita G, Early onset neonatal sepsis due to Neisseria meningitidis W135Pediatr Infect Dis J 1987 6(3):299-300. [Google Scholar]
[36]. Chugh K, Bhalla CK, Joshi KK, Meningococcal brain abscess and meningitis in a neonatePediat Infect Dis J 1988 7(2):136-37. [Google Scholar]
[37]. de Louvois J, Blackbourn J, Hurley R, Harvey D, Infantile meningitis in England and Wales: a two year studyArch Dis Child 1991 66:603-07. [Google Scholar]
[38]. Sapan N, Cuneydi S, Ildirim I, Koksal N, Songur S, Tas Z, A meningococcal meningitis case in neonatal periodJ ANKEM 1993 7:12-14. [Google Scholar]
[39]. Kirkpatrick M, Brooker RJ, Helma PJ, Cole GF, Spinal cord dysfunction in neonatal meningococcal meningitisEur J Ped 1994 153:367-68. [Google Scholar]
[40]. Chiu CH, Lin TY, Yang PH, Hwang MS, Neonatal meningococcal meningitis: report of two casesZhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 1994 35(6):542-45. [Google Scholar]
[41]. Arango Carlos A, Rathore Mobeen H, Neonatal meningococcal meningitis: case reports and review of literaturePediatr Infect Dis J 1996 15(12):1134-36. [Google Scholar]
[42]. Falero GMP, Arroyos PA, Santillana FL, Cazorla CR, Cobas PJ, Ureta HA, Late neonatal sepsis with meningitis due to meningococcus serogroup CAn Esp Pediat 1999 50(6):639-40. [Google Scholar]
[43]. Casanova-Román M, Rios J, Garcia-Del-Rio M, Martínez-Valverde A, Early onset neonatal sepsis due to Neisseria meningitidis BMinerva Pediatr 2000 52(11):659-60. [Google Scholar]
[44]. Katier N, Traen M, De Dooy J, Geyskens L, Mahieu L, Neonatal Purpura fulminans due to Neisseria meningitidis serogroup C infectionEur J Ped 2003 162:283-84. [Google Scholar]
[45]. Tinsa F, Jallouli M, Ben Lassouad M, Smaoui H, Brini I, Bousseta K, Neonatal meningitis by Neisseria meningitisB La Tunisie Medicale 2008 86(11):1014-15. [Google Scholar]
[46]. Kurlenda J, Agata KP, Grinholc M, Neonatal intrauterine infection with Neisseria meningitidisB Clin Pediatr 2010 49(4):388-390. [Google Scholar]
[47]. Cho KH, Lee H, Kang JH, Kim KN, Kim DS, Kim YK, The causative organisms of bacterial meningitis in Korean children in 1996 – 2005J Korean Med Sci 2010 25(6):895-99. [Google Scholar]
[48]. Fuentes AD, Fuhrmann CF, Santis DA, Neonatal meningococcal disease 2011An Pediatr 2011 75:213-15. [Google Scholar]
[49]. Smith A, Zehetner A, Early onset neonatal serogroup B meningococcal meningitis and septicaemiaJ Paediatr Child Health 2013 49(2):158 [Google Scholar]
[50]. Ramsamy Y, Mahabeer P, Archary M, Bobat RA, Coovadia YM, An unusual case of neonatal meningococcal meningitis complicated by subdural empyema and hydrocephalusS Afr J of Child Health 2013 7(1):35-37. [Google Scholar]
[51]. Bosman M, Archary M, Mahabeer P, Bobat RA, Early onset meningococcal meningitisSouth Afr J Epidemiol Infect 2013 28(3):177-79. [Google Scholar]
[52]. Shah S, Gross JR, Stewart CT, A case report of meningococcal disease in a neonateWMJ 2013 112(1):28-30. [Google Scholar]
[53]. Kumar D, Yadav RK, Singh DK, Sharma IK, Shukla KM, Avais M, Fulminant meningococcemia with meningococcal meningitis in the neonate: a case reportInt J Contemp Pediatr 2014 1:190-92. [Google Scholar]
[54]. Devi U, Mahanta J, Neonatal meningitis due to Neisseria meningitidis serogroup Y (letter)Indian Pediatr 2014 51:757 [Google Scholar]
[55]. Kiray Bas E, Bulbul A, Comert S, Uslu S, Arslan S, Nuhoglu A, Neonatal infection with Neisseria meningitidis: analysis of a 97-year period plus case studyJ Clin Microbiol 2014 52(9):3478-82. [Google Scholar]