Kikuchi-Fujimoto Disease Masquerading as Acute Appendicitis
Vinita Pandey1, Yasmeen Khatib2, Rahul Pandey3, Archana L Khade4, Manisha Khare5
1 Ex-Registrar, Department of Pathology, HBT Medical College and Dr. R.N. Cooper Hospital, Juhu, Mumbai, Maharashtra, India.
2 Associate Professor, Department of Pathology, HBT Medical College and Dr. R.N. Cooper Hospital, Juhu, Mumbai, Maharashtra, India.
3 Ex-Registrar, Department of Pathology, TATA Memorial Hospital, Parel, Mumbai, Maharashtra, India.
4 Assistant Professor, Department of Pathology, HBT Medical College and Dr. R.N. Cooper Hospital, Juhu, Mumbai, Maharashtra, India.
5 Professor, Department of Pathology, HBT Medical College and Dr. R.N. Cooper Hospital, Juhu, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Archana Khade, Department of Pathology, 1st Floor, ‘B’ wing, HBTMC and Dr. R.N. Cooper Hospital, Juhu, Mumbai, Maharashtra, India.
E-mail: arck115@gmail.com
Kikuchi-Fujimoto Disease (KFD) is a self-limiting necrotizing lymphadenitis that usually presents with fever and cervical lymphadenopathy. Recognition of this condition is crucial, because it can be mistaken for tuberculosis, lymphoma and connective tissue disorders. When present at an unusual location the diagnosis can be challenging. We present an unusual case of Kikuchi-Fujimoto disease involving mesenteric lymph node masquerading as acute appendicitis along with its differential diagnosis.
A 30-year-old female presented with complaints of acute abdominal pain, vomiting and fever. Physical examination revealed rebound tenderness in the right iliac fossa. The abdominal sonography was suspicious of acute appendicitis. The patient underwent appendectomy with excision of an enlarged mesenteric lymph node. On histopathology mesenteric node showed features of KFD which was confirmed on immunohistochemistry. Appendix was unremarkable. Although rare KFD should be added to the differential diagnosis of acute appendicitis in patients with enlarged mesenteric lymph nodes, Awareness of this disorder helps to prevent misdiagnosis and inappropriate treatment.
Acute abdomen, Histiocytic necrotizing lymphadenitis, Mesenteric lymph node
Case Report
A 30-year-old female presented to the emergency department with acute abdominal pain, vomiting and fever. There was no history of skin rash or joint symptoms. On examination patient was febrile and revealed rebound tenderness in the right iliac fossa. There was no peripheral lymphadenopathy or hepatosplenomegaly. The leukocyte count was 12,300 cells/cumm and erythrocyte sedimentation rate was 30 mm/hr.
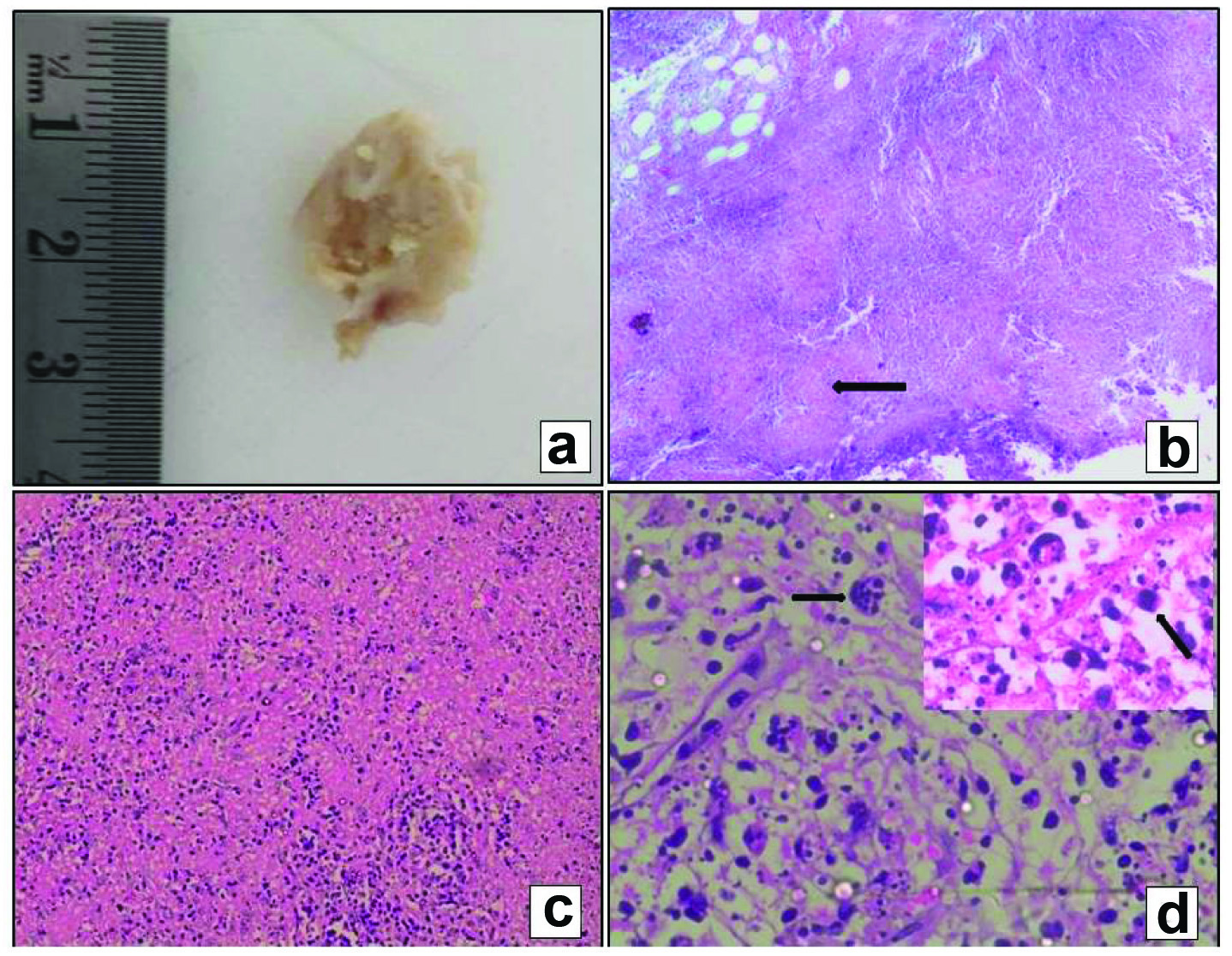
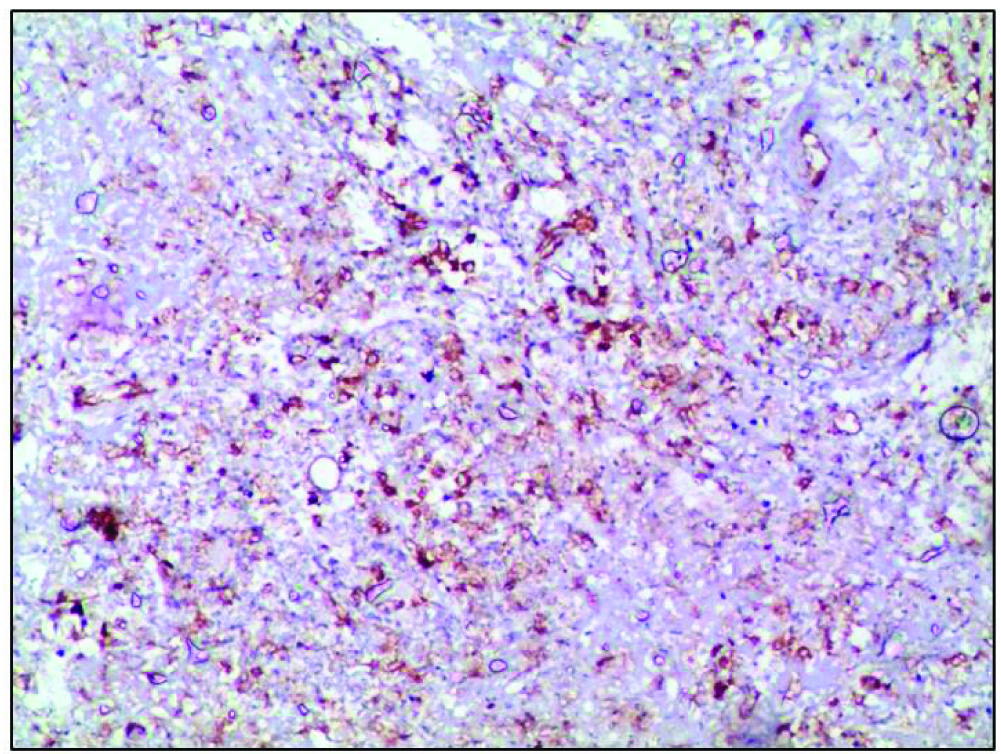
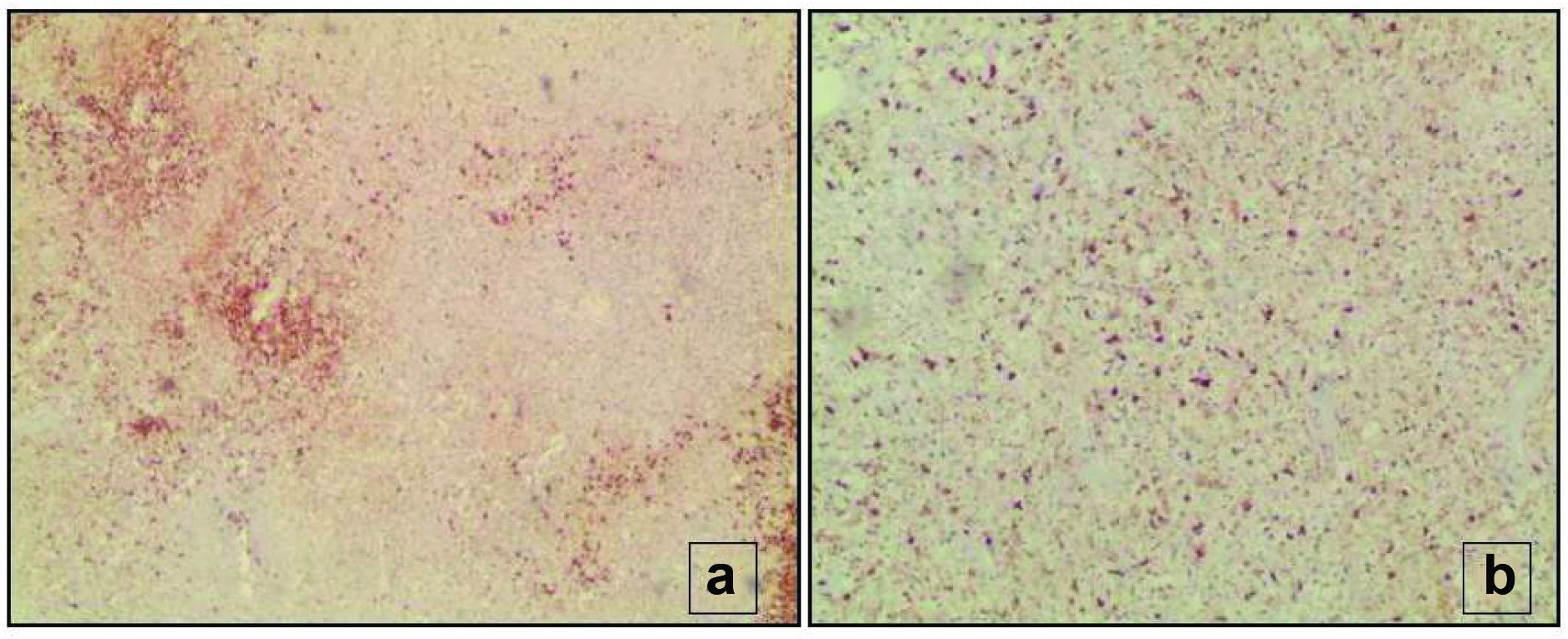
The abdominal sonography showed features suspicious of acute appendicitis. With the clinical impression of acute appendicitis, the patient underwent laparotomy. Intraoperatively, a normal appearing appendix was found along with an enlarged ileocaecal lymph node. Appendectomy and excision of the mesenteric lymph node was carried out. On gross examination, the appendix was unremarkable. The mesenteric lymph node measured 1.5 cm in diameter and was extremely friable [Table/Fig-1a]. On microscopic examination, the lymph node showed partial effacement of nodal architecture with patchy necrosis in cortical and paracortical areas [Table/Fig-1b]. High power examination showed karyorrhectic nuclear debris along with lymphocytes, histiocytes and mononuclear cells with plasmacytoid morphology [Table/Fig-1c,d]. No neutrophils, plasma cells or granulomas were seen. Evaluation with periodic acid-schiff and silver stains, to rule out fungal infection, and special stain for acid fast bacilli, were negative. On immunohistochemical examination the histiocytes were highlighted by CD 68 and CD 123 {Interleukin (IL)-3-R} stains [Table/Fig-2]. CD20 shows few residual lymphoid follicles [Table/Fig-3a]. CD 3 showed few T-lymphocytes in the background [Table/Fig-3b]. The appendix was unremarkable. Based on the histopathological and immunohistochemical findings the diagnosis of necrotizing lymphadenitis of Kikuchi Fujimato type was made. The patient had an uneventful postoperative course.
(a) Gross appearance of mesenteric lymph node which is grayish white with necrosis: (b) Shows low power view with effacement of lymph node architecture with patchy areas of necrosis (H & E, 4X); (c) Shows necrosis with abundant karryorrhectic debris and histiocytes (H & E, 10X); (d) Shows macrophages with emperipolesis (H & E 40X) and plasmacytoid histiocytes (Inset, H & E, 100X),
CD 123 positive plasmacytoid histiocytes characteristic of Kikuchi – Fujimoto disease (10X).
(a) shows CD 20 positive cells representing residual lymphoid follicles. (10X); (b) Shows CD 3 positive T lymphocytes in the background (10X).
Discussion
KFD is a rare self limiting benign form of necrotizing histiocytic lymphadenitis first reported by Fujimoto Y and Kikuchi Y in Japan in 1972 [1,2]. Though, it has a worldwide distribution, it is more common in young women of Asian background. Clinical features include painful lymphadenopathy, commonly involving the cervical lymph nodes, fever, malaise, anorexia, myalgia, rash and arthralgia [3]. Localization of Kikuchi’s Disease (KD) to the mesenteric lymph nodes is quite unusual and presents with clinical features of acute abdomen. This unusual location of lymph node involvement can make the diagnosis of KD perplexing for both the surgeon and the pathologist. Only 16 cases have been previously reported in the world literature with this presentation to the best of our knowledge [4-13]. These patients presented with fever along with right quadrant abdominal pain, positive Mcburneys sign and rebound tenderness which are the classic features of acute appendicitis which was similar to our case [5,6,9]. Eleven of these patients underwent laparotomy [4,5,8] and three underwent laparoscopy for diagnosis [6,9]. In one case percutaneous transabdominal lymph node biopsy was done [12]. Eleven of the 15 cases had isolated mesenteric lymphadenitis on CT scan examination with the clinical impression of acute abdomen, as in our case [10]. Vijayraghavan R et al., did a review of all cases of KD of mesenteric lymphadenitis presenting as acute appendicitis and reported five cases [9]. Preston DV et al., has reported a case of KD involving mesenteric lymph node with overlapping features of Systemic Lupus Erythaematosus (SLE) [13]. Patel N et al., reported a case of mesenteric lymphadenitis in which PET scan revealed enlarged inguinal node which was biopsied and surgery was avoided [10]. Although, the diagnosis of KD is based on histopathology examination and Immunohistochemistry (IHC) of the affected lymph node, the list of morphologic mimics is long. Grossly the nodes measure 0.5 to 4 cms in size [9]. The characteristic microscopic features of KFD include areas of coagulative necrosis, with abundant karyorrhectic debris which can distort the nodal architecture along with a large number of plasmacytoid histiocytes at the margin of the necrotic area. These cells are of intermediate size with eosinophilic cytoplasm and nucleus pushed to the periphery. Neutrophils and plasma cells are significantly absent [5]. A predominance of CD8+ cells over CD4+ cells among the T-cell infiltrate is noted. The histiocytes express histiocyte-associated antigens such as myeloperoxidase, lysozyme, CD 68 and interleukin receptor CD 123 [14].
The differential diagnosis of KD includes lymphadenitis associated with SLE, lymphoma and infections like tuberculosis. Unlike KFD, SLE lymph node shows presence of haematoxylin bodies which are composed of altered nuclear material and Azzopardi phenomenon (degenerated nuclear material aggregated in the walls of blood vessels). In SLE, abundant plasma cells, prominent reactive follicular hyperplasia, sparse cytoxic T-cells and capsular and pericapsular inflammation are seen [14,15]. The clinical presentation and positivity for antinuclear antibodies can be helpful in difficult cases.
KD can mimic lymphoma in the presence of atypical mononuclear cells and immunoblasts. These plasmacytoid monocytes are positive for CD 68 and CD 123, while they are negative for CD 3, CD 20, which excludes the possibility of lymphomas [11]. Rarely, KD may be associated with histiocytes resembling signet ring cells and a diagnosis of metastatic adenocarcinoma can be considered. The latter however has atypical nuclei containing mucin rather than cellular debris [7].
Several infectious aetiologies can also mimic KD [15]. Tuberculosis remains a major differential diagnosis, especially in a developing country like India. Non reactive tuberculosis may show large areas of necrosis and paucity of epithelioid granulomas. It is therefore necessary to screen a necrotic lymphnode, for acid fast bacilli, with special stains. A perivascular plasma cell rich inflammatory infiltrate is seen in necrotizing lymphadenitis due to syphilis.
Yersinia infection is characterized by the presence of micro-abscesses with polymorphonuclear leukocytes localized to germinal centers and aggregates of epithelioid histiocytes producing a granulomatous reaction. The absence of granulocytes in the areas of necrosis and lack of follicular hyperplasia also differentiates KFD from cat - scratch disease and other bacterial infections [15]. The course and treatment of KD differs greatly from these conditions which should be excluded before a diagnosis of KD is made.
The etiology of KD is not known although an infectious, viral, genetic and autoimmune hypothesis has been proposed [9]. Infection with EBV virus, human herpes virus 6, toxoplasma and yersinia has been implicated as the causative agents. It has been hypothesized that KD might represent a T-cell mediated response to certain antigenetic stimuli in genetically susceptible individuals. The CD 8 positive lymphocytes induce apoptosis which results in characteristic necrosis and nuclear debris seen in KD. It might represent a SLE like autoimmune type lymphadenitis triggered by viruses or other infectious agents [9]. KD can also precede or coincide with the diagnosis of SLE and SLE should always be excluded in patients presenting with necrotising lymphadenitis [13].
Conclusion
KD is a rare and possibly an under-diagnosed condition with a good prognosis. When the mesenteric node is involved it can present as acute abdomen and clinically mimic appendicitis. If a peripheral lymph node is also enlarged excision can be done avoiding abdominal surgery. In case of isolated mesenteric lymph node involvement excision of the node followed by histopathology and IHC is necessary for the diagnosis.
[1]. Fujimoto Y, Kozima Y, Yamaguchi K, Cervical subacute necrotizing lymphadenitis:A new clinicopathologic entityNaika 1972 20:920-27. [Google Scholar]
[2]. Kikuchi M, Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes:a clinicopathological studyActa Haematol Jpn 1972 35:379-80. [Google Scholar]
[3]. Kucukardali Y, Solmazgul E, Kunter E, Oncul O, Yildirim S, Kaplan M, Kikuchi-Fujimoto disease:analysis of 244 casesClin Rheumatol 2007 26:50-54. [Google Scholar]
[4]. Mcloughlin J, Creagh T, Taylor A, Lampert I, Kikuchi’s disease simulating acute appendicitisBr J Surg 1988 75:1206 [Google Scholar]
[5]. Min KW, Jang K, Jang SH, Paik SS, Kikuchi’s disease of the mesenteric lymph nodes presenting as acute appendicitisKorean J Pathol 2007 41:44-46. [Google Scholar]
[6]. Oh BJ, Choi WJ, Lim KS, Kim W, Kikuchi-Fujimoto disease:three cases presenting as acute abdomenJ Korean Soc Emerg Med 2005 16:194-99. [Google Scholar]
[7]. Tsang WY, Chan JK, Ng CS, Kikuchi’s lymphadenitis. A morphologic analysis of 75 cases with special reference to unusual featuresAm J Surg Pathol 1994 18:219-31. [Google Scholar]
[8]. Van Rij S, Wright D, Kikuchi-Fujimoto’s disease mimicking acute appendicitisANZ J Surg 2010 80:760-61. [Google Scholar]
[9]. Vijayaraghavan R, Chandrashekar R, Saraswathi A, Belagavi CS, Kikuchi-Fujimoto’s disease involving mesenteric nodes:a report and review of literatureBMJ Case Rep 2011 2011:bcr1020114945 [Google Scholar]
[10]. Patel N, Philips D, Nigo M, Kaminsky D, Mildvan D, Kikuchi-Fujimoto disease and acute appendicitisBMJ Case Rep 2014 2014pii:bcr-201420409815 [Google Scholar]
[11]. Teranishi H, Kawasaki K, Sasaki A, Fujimoto H, Inoue M, Monju A, Localized intraabdominal Kikuchi-Fujimoto’s disease:a case report and review of literatureKawasaki Med J 2008 34:285-89. [Google Scholar]
[12]. Suda H, Itoh S, Saigusa Y, A case of histiocytic necrotising lymphadenitis showing focal lymph node swelling in the abdomenNihon shokakibyo Gakkai Zasshi 2007 104:579-83.Japanese [Google Scholar]
[13]. Preston DB, Pound CM, Jurencak R, An atypical presentation of Kikuchi-Fujimoto disease mimicking SLE:Case report and literature reviewOpen Journal of Paediatrics 2011 1:67-71. [Google Scholar]
[14]. Kuo TT, Kikuchi’s disease (histiocytic necrotizing lymphadenitis). Aclinicopathologic study of 79 cases with an analysis of histologicsubtypes, immunohistology and DNA ploidyAm J Surg Pathol 1995 19:798-809. [Google Scholar]
[15]. Hutchinson CB, Wang E, Kikuchi-Fujimoto diseaseArch Pathol Lab Med 2010 134:289-93. [Google Scholar]