Wunderlich Syndrome due to Ruptured Pseudoaneurysm of Angiomyolipoma in First Trimester: A Rare Case Report
Sunil Raghunath Patil1, Prakash Wamanrao Pawar2, Ajit Somaji Sawant3, Abhishek Jaysukhbhai Savalia4, Ashwin Sunil Tamhankar5
1 Senior Registrar, Department of Urology, Lokmanya Tilak Municipal Medical College, Sion, Mumbai, Maharashtra, India.
2 Associate Professor, Department of Urology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India.
3 Professor and Head, Department of Urology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India.
4 Senior Registrar, Department of Urology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India.
5 Senior Registrar, Department of Urology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Raghunath Patil, Senior Registrar, Department of Urology, Room No. 219, 2nd Floor, College Building, Lokmanya Tilak Municipal Medical College, Sion–400022, Mumbai, Maharashtra, India.
E-mail: sunil7887@gmail.com
Angiomyolipoma (AML) is a rare benign tumour of kidney which demonstrates rapid growth during pregnancy due to hormonal stimulation, leading to rupture. Majority of reported ruptured AMLs are in third trimester. We report a case of ruptured angiomyolipoma at 10th week of gestation, the earliest rupture known in singleton pregnancy. The AML had pseudo-aneurysm formation with extra-tumoural rupture during pregnancy, a finding never reported in literature yet. The patient had active bleeding with expanding peri-nephric haematoma during initial two days of conservative management. Hence, after counselling and taking prior informed written consent for Medical Termination of Pregnancy (MTP), computed tomography scan of abdomen with angiography followed by emergency coil embolization of the bleeding right upper polar segmental artery was done. After stabilization, MTP was done at 12th week of gestation. Counselling and consent for continuing or aborting the pregnancy is of utmost importance for best possible outcome for patient and foetus.
Abortion, Angiomyolipoma pregnancy, Coil embolisation, Medical termination of pregnancy
Case Report
A 24-year-old female {Gravida 2, Medical Termination of Pregnancy (MTP) 1} presented at emergency department at 10th week of gestation with history of right flank pain since three days. She had no complaints of fever, vomiting or haematuria. There was no history of flank pain or any other surgical illness. She had history of first trimester (six weeks) abortion done nine months back as it was an unplanned pregnancy. On physical examination, she had tachycardia (pulse = 106 per minute), blood pressure of 100/60 mmHg with pallor. Per-abdominal examination revealed fullness over right flank with tenderness over right flank, lumbar and iliac regions.
Routine blood investigations showed haemoglobin of 7.7 gm/dL with haematocrit 28.4% and total leucocyte count of 12.2 X 109/L. Renal function tests were within normal limits (serum creatinine = 0.8 mg/dL). Ultrasonography of abdomen revealed a hyperechoic lesion measuring (7.4 x 5.7) cm involving upper and mid-pole of right kidney, with vascularity and few hypoechoic areas within, which was suggestive of angiomyolipoma. Also, there was associated heterogeneously hyperechoic collection measuring (10 x 3) cm along anterior pre-renal space extending inferiorly with compression of right kidney which was suggestive of peri-renal haematoma.
On the next day of presentation, tachycardia was persistent with maintained blood pressure. Haemoglobin was 7.3 gm/dL with haematocrit dropping to 22.4% despite one whole blood transfusion. The abdominal girth increased by one inch, suggestive of active bleeding. Patient was explained about her condition and about options of either emergency exploration, which had high probability of requiring nephrectomy, or emergency renal angiography followed by angioembolisation with radiation exposure risk to foetus and consequent foetal malformations, requiring MTP.
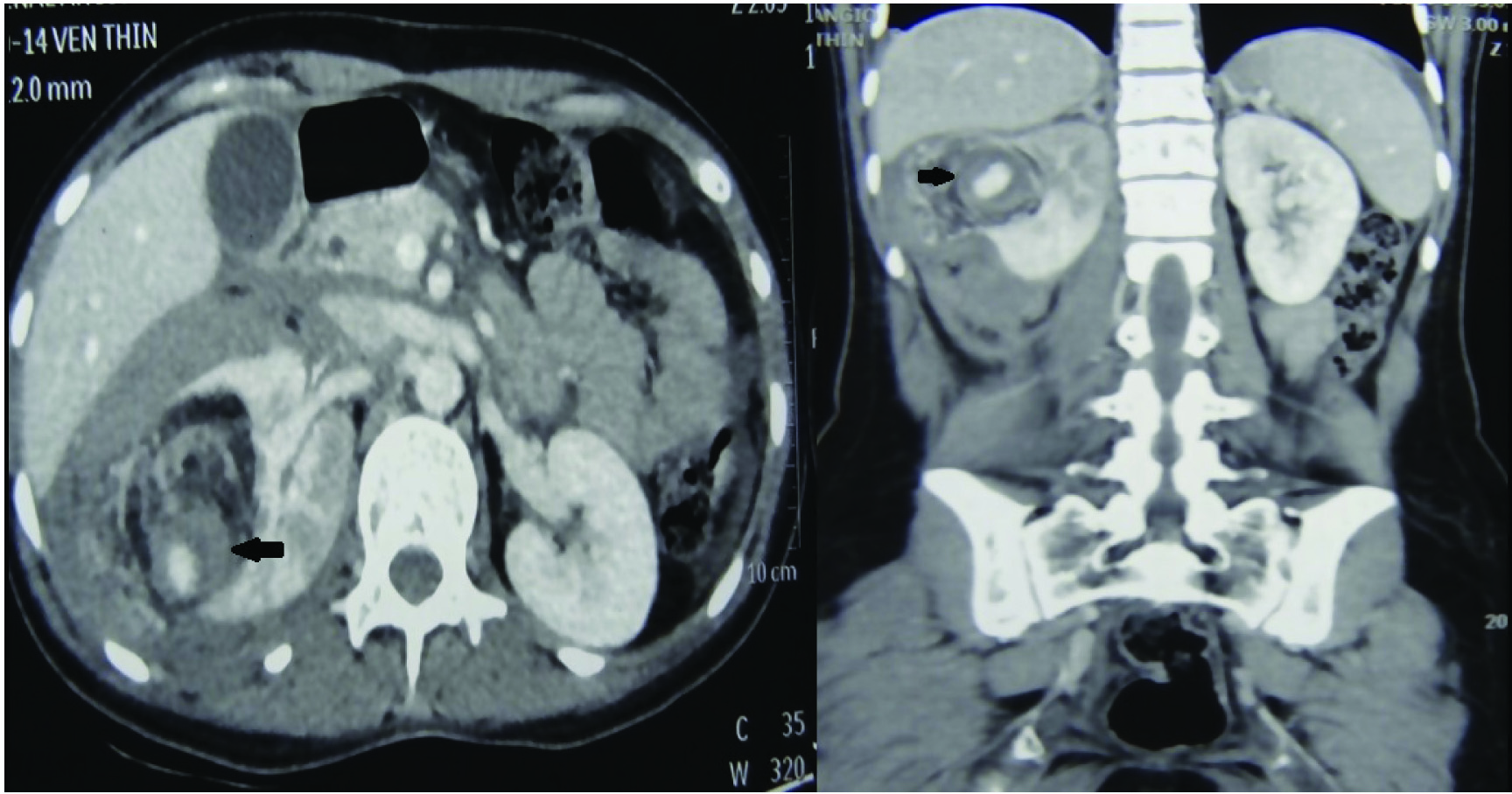
Patient consented for the later procedure. Thus, Computed Tomography (CT) scan of abdomen with angiography [Table/Fig-1] was done. It showed an ill-defined heterogeneously enhancing mass lesion arising from midpole of right kidney, measuring (6.9 x 7.9 x 7.3) cm with few hypodense areas of fat attenuation (mean Hounsfield unit -63), confirming it as angiomyolipoma. Also, a pseudo-aneurysm measuring (17 x 16.5) mm with homogenous contrast blush on arterial phase was seen, arising from peripheral branch of upper polar artery. The retroperitoneal haematoma measured (17 x 9) cm.
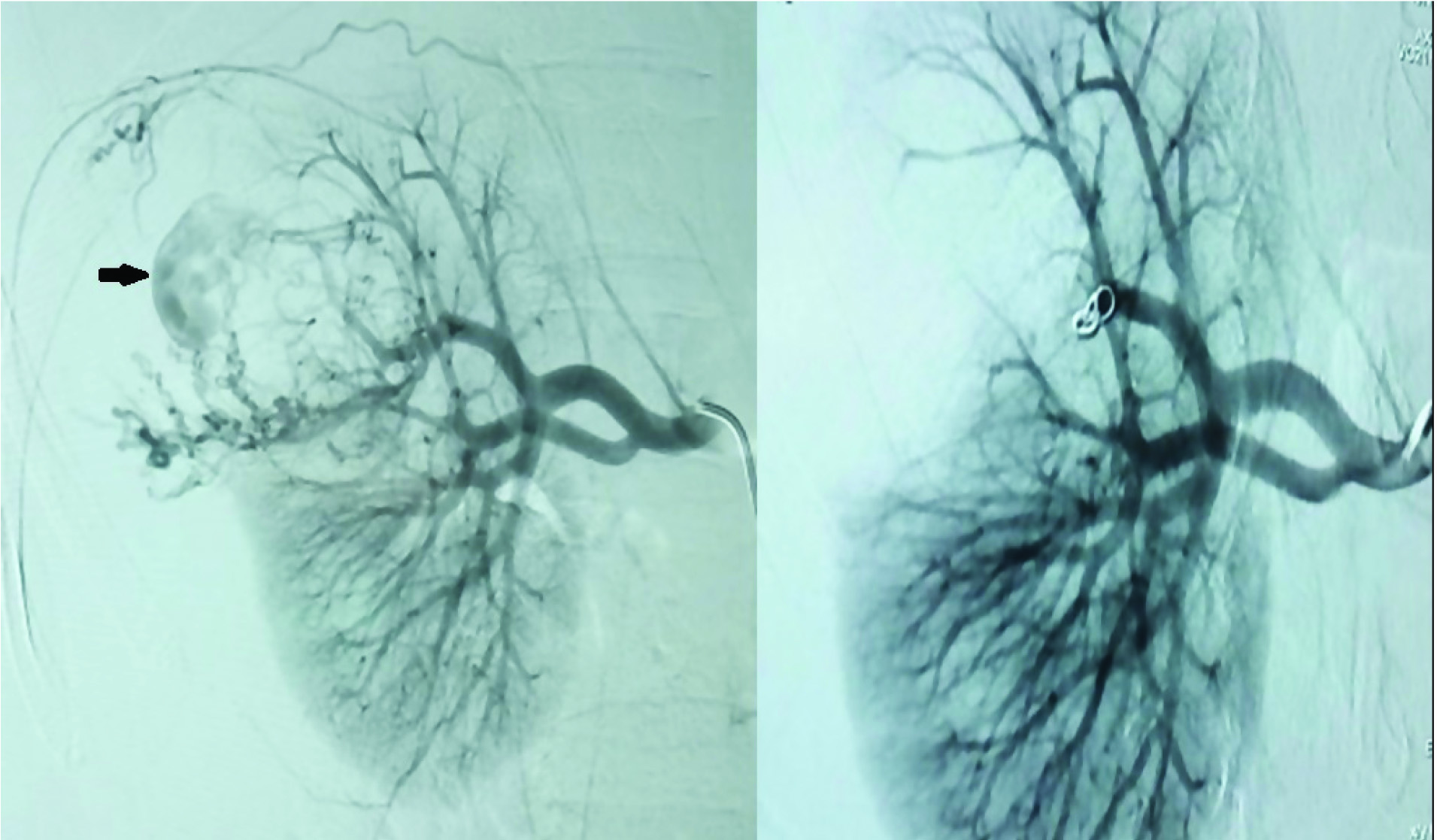
Emergency coil embolization [Table/Fig-2] of the bleeding right upper polar segmental artery was done by vascular interventional radiology department on the second day of presentation. Post-embolisation, patient’s pulse settled to 78 per minute within 72 hours. Her haemoglobin increased to 9.5 gm/dL after two more whole blood transfusions. Repeat ultrasonography studies over next ten days revealed no change in the size of retroperitoneal haematoma. Post-stabilization, she was transferred to obstetrics department for MTP, which was performed at 12 weeks’ gestation. The patient had no complications till three months of follow-up, and had no recurrent bleeding.
Computed tomography images (axial and coronal) showing angiomyolipoma in right midpole with contrast blush suggestive of pseudoaneurysm, and retroperitoneal haematoma.
Pre and post-embolisation renal angiography images showing the pseudoaneurysm, and wedge shaped area of infarct with the coil in situ.
Discussion
Angiomyolipoma (AML) is a rare benign tumour of kidney with incidence of 0.3% [1] in general population. It is more common in females, and demonstrates rapid growth during pregnancy and in patients on oral contraceptive pills [2], indicating response to hormonal stimulation. Very few cases of rupture of angiomyolipoma in pregnancy have been reported, with majority occurring in third trimester [3]. This is a case of ruptured angiomyolipoma at 10th week of gestation, the earliest rupture known in singleton pregnancy. The patient had pseudo-aneurysm formation with extra-tumoural rupture during pregnancy, which is also a unique finding, with no such case reported, to the best of our knowledge.
Angiomyolipoma has a monoclonal origin from perivascular epithelioid cells (PEComas). They are composed of abnormal blood vessels, muscle cells and adipose tissue. Cases associated with tuberous sclerosis present as multiple, bilateral, recurrent tumours. The presence of hormone receptors in angiomyolipoma is well established, with reported oestrogen and progesterone receptor positivity rate of 12.5% and 37.5% respectively in Indian patients [4]. Wunderlich syndrome refers to spontaneous (non-traumatic) peri-renal/subcapsular haemorrhage. Approximately 10% of patients with angiomyolipoma present with Wunderlich syndrome, which can be life threatening. It is more common in pregnancy and the incidence increases with each trimester due to rising levels of oestrogen and progesterone. Approximately two-third cases reported in pregnancy are in the third trimester with average being around 27th week [3]. Our case is the earliest to present in singleton pregnancy at 10th week, along with another case report by Morales JP et al., at 10th week, which was also managed by embolisation [5]. Ferianec V et al., had reported the earliest known case in pregnancy with Wunderlich syndrome, at ninth week [6]. It was a twin pregnancy causing more hormonal escalation than a normal singleton pregnancy, explaining the early rupture.
Pseudoaneurysm formation is a very rare phenomenon in angio-myolipoma of pregnancy, with only two other cases reported in literature [7,8]. Intratumoural rupture has been postulated to be the cause of pseudoaneurysm formation [7]. In our case, it could be attributed to the previous six weeks’ pregnancy. The present pregnancy caused exacerbation leading to extra-tumoural rupture of the pseudoaneurysm at an early stage of 10 weeks.
The management should be individualized based on patient’s haemodynamic status, weeks of gestation, requirement of blood transfusion and association with tuberous sclerosis [1]. Haemodynamically stable patients with non-expanding haematoma and stable haematocrit can be followed up from any trimester till term pregnancy, followed by definitive management in post-natal period with angioembolisation [9] or partial nephrectomy. Haemodynamically unstable patients with expanding haematoma need to be operated on emergency basis, having high rates of nephrectomy (79%) [3] due to extensive haematoma and requirement of urgent haemostatic control. Medical termination of pregnancy may be performed depending on the severity of presentation [6]. But majority of them can be followed up till term [10]. Simultaneous premature termination of pregnancy can be performed for patients more than 28 weeks’ gestation [9]. Haemodynamically stable patients requiring repeated transfusions or with expanding haematoma or pseudo-aneurysm formation can be managed with angio-embolisation of the segmental bleeding vessel [7,8]. The use of radiation shielding of lower abdomen with collimation of X-Ray beam and minimal use of fluoroscopy is necessary during embolisation to reduce radiation exposure to foetus [8]. Successful term delivery post-embolisation is feasible in all trimesters including first trimester [5]. Although the patient needs to be counselled regarding the risk of foetal malformation in first trimester, and then the decision to continue or abort pregnancy should be taken accordingly. Tuberous sclerosis patients require conservative management, including embolisation, for renal preservation, due to high recurrence rates [7].
Davis NF et al., had described successful salvage of foetus from 16th week gestation till term, despite doing CT scan of abdomen and renal angiography for angioembolisation, using the techniques to decrease the radiation exposure to foetus described above[8]. However, our patient was a first trimester case, which has much higher risk of foetal malformations as compared to second or third trimester. The patient was not willing for emergency open exploration (and risk sacrificing one kidney). On the other hand, her clinical condition did not permit waiting till 12 weeks of gestation for renal angiography and embolisation. Hence, after taking consent, CT imaging was done to confirm the diagnosis of angiomyolipoma (more reliable than MRI) and for determining the feasibility of partial/hemi-nephrectomy as definitive management post-MTP.
Conclusion
Foetus can be salvaged in majority of these cases. Counseling and consent for continuing or aborting the pregnancy is of utmost importance for selecting the most appropriate management strategy for best possible outcome for the patient and foetus.
[1]. Zapardiel I, Delafuente-Valero J, Bajo-Arenas JM, Renal angiomyolipoma during pregnancy:review of the literatureGynecol Obstet Invest 2011 72(4):217-19. [Google Scholar]
[2]. Gould Rothberg BE, Grooms MC, Dharnidharka VR, Rapid growth of a kidney angiomyolipoma after initiation of oral contraceptive therapyObstet Gynecol 2006 108(3):734-36. [Google Scholar]
[3]. Raft J, Lalot JM, Meistelman C, Longrois D, Influence of pregnancy on renal angiomyolipomaGynecol Obstet Fertil 2005 33(11):898-906. [Google Scholar]
[4]. Kulkarni B, Desai SB, Dave B, Tongaonkar HB, Kulkarni JN, Chinoy RF, Renal angiomyolipomas--a study of 18 casesIndian J Pathol Microbiol 2005 48(4):459-63. [Google Scholar]
[5]. Morales JP, Georganas M, Khan MS, Dasgupta P, Reidy JF, Embolization of a bleeding renal angiomyolipoma in pregnancy:case report and reviewCardiovasc Intervent Radiol 2005 28(2):265-68. [Google Scholar]
[6]. Ferianec V, Gábor M, Caňo M, Papcun P, Holomáň K, Severe retroperitoneal haemorrhage in the first trimester of a multiple pregnancy after spontaneous rupture of renal angiomyolipomaArch Gynecol Obstet 2013 288(6):1193-94. [Google Scholar]
[7]. Idilman IS, Vesnic S, Cil B, Peynircioglu B, Giant renal artery pseudoaneurysm caused by rupture of renal angiomyolipoma following pregnancy:endovascular treatment and review of the literatureSaudi J Kidney Dis Transpl 2014 25(2):385-89. [Google Scholar]
[8]. Davis NF, Kelly R, Lee MJ, Mohan P, Selective arterial embolisation of bilateral angiomyolipomata in a symptomatic pregnant femaleBMJ Case Rep 2013 2013pii:bcr2013009256 [Google Scholar]
[9]. Tanaka M, Kyo S, Inoue M, Kojima T, Conservative management and vaginal delivery following ruptured renal angiomyolipomaObstet Gynecol 2001 98:932-33. [Google Scholar]
[10]. Preece P, Mees B, Norris B, Christie M, Wagner T, Dundee P, Surgical management of haemorrhaging renal angiomyolipoma in pregnancyInt J Surg Case Rep 2015 7:89-92. [Google Scholar]