An Unusual Presentation of Conjunctival Infection
Shobha Pai1, Madhurima Nayak2, Gloria George3
1 Head, Department of Ophthalmology, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
2 Senior Resident (Former), Department of Ophthalmology, Kasturba Medical College, Mangalore, Karnataka, India.
3 PG Resident, Department of Ophthalmology, Kasturba Medical College, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shobha Pai, Head, Department of Ophthalmology, Kasturba Medical College, Mangalore-575001, Karnataka, India.
E-mail: drsgpai@rediffmail.com
Conjunctival ulcer, limbal nodule, Phlyctenulosis
Dear Editor,
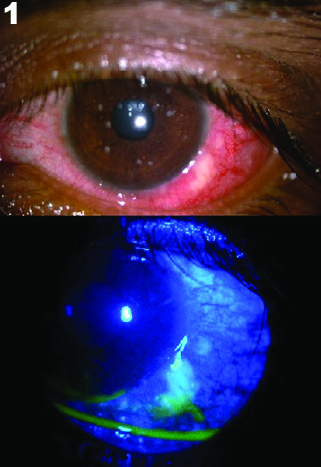
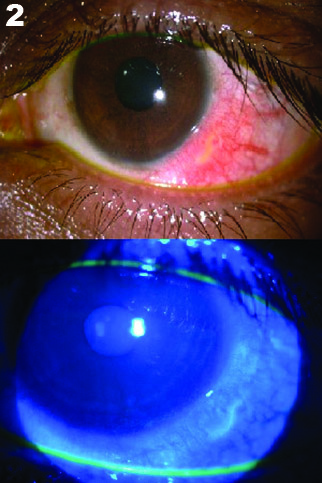
We report a case of unilateral conjunctival ulceration in a 24-year-old male patient. He presented to us with pain and redness of his left eye since two weeks and noticed a small swelling over the white area of his eye which was painful. He consulted a nearby ophthalmologist who started him on Topical antibiotics and was referred to us after a week, when his symptoms increased. He gives a history of a similar episode six months earlier. There was no history of joint pain, fever, and cough, genital or oral ulceration. On examination, he was afebrile, vitals were stable and systemic examination was normal. Unaided visual acuity was 6/6 in both eyes. Lids and adnexa were normal. The temporal conjunctiva in the left eye was congested with presence of a mildly elevated, irregular, nodular yellow lesion 2 mm away from the limbus with a raw surface which was demonstrated by staining with fluorescein dye and measured 3.4 x 2 mm. It was surrounded by dilated and tortuous conjunctival and episcleral vessels [Table/Fig-1]. The lesion was tender. The cornea revealed superficial punctate erosions inferiorly. Rest of the anterior segment was normal. There was no preauricular lymphadenopathy. Corneal sensations were intact. A provisional diagnosis of conjunctival ulcer was made. Edges of the ulcer were scraped and sent for culture and sensitivity, blood was sent for routine investigations, Rheumatoid factor (RA factor), Anti-nuclear Antibody (ANA) and Mantoux test was done to rule out systemic associations. Gram stain showed polymorphonuclear leukocytes and culture revealed no growth, RA factor and ANA were negative, blood investigations were within normal limits and Mantoux reading after 48 hours was 8mm. He was started on ofloxacin 0.3% eyedrops and ointment, tear film substitutes (carboxymethyl cellulose 0.5%) and anti-inflammatory eyedrops (nepafenac 0.3%). He reviewed with us after three days and was symptomatically better; ulcer size had decreased to 2.9 x 1.5 mm. Treatment was continued for two more weeks, ulcer size progressively decreased and healed [Table/Fig-2]. The symptoms had completely resolved.
Above: Left eye showing congested temporal conjunctiva with elevated, irregular, nodular yellow lesion 2 mm away from limbus, surrounded by dilated and tortuous conjunctival and episcleral vessels. Below: Raw surface of lesion as demonstrated by staining with fluorescein dye mea-suring 3.4 x 2 mm. Cornea shows superficial punctate erosions inferiorly.
Above: After two weeks of treatment, conjunctival congestion decreased, lesion size significantly reduced. Below: Fluorescein staining demonstrates decrease in size of raw surface of lesion and healed corneal erosions.
Nodular lesions at the limbus and bulbar conjunctiva have a variety of differential diagnoses. The exhaustive list includes pinguecula, early pterygium, limbal dermoid, granuloma, nodular episcleritis and scleritis, phlyctenulosis, ocular surface squamous neoplasia and conjunctival ulcer [1,2]. This case very closely resembles phlyctenular ulcer. Phlyctenulosis is more commonly seen in a younger age group and associated with hypersensitivity to tubercular protein. The nodule is almost always located at the limbus with marked elevation and a localised leash of vessels feeding the nodule [3]. The points in favour of ulcer in this case were the presence of pain and corneal erosions, tenderness, location away from the limbus, diffuse temporal congestion and a raw surface evident from fluorescein staining. Mahendradas P et al., reported a similar case of conjunctival ulceration which responded to quinolones and co-trimoxazole [2]. Other known infective associations with conjunctival ulcer include tuberculosis and herpetic conjunctival ulcer [1,4]. Documented non-infective causes include Behcet’s disease [5] and Crohn’s disease [6]. Hence, systemic evaluation is also warranted in such cases.
Rare occurrence of conjunctival ulcers have also been reported post cataract extraction, which responded to corticosteroids [7]. The fact that scraping from the ulcer did not yield any growth supports a non-infective cause for ulceration in this case; however it must be borne in mind that the patient was already on topical antibiotics which might have led to the result. The rare presentation of a conjunctival ulcer may therefore often elude diagnosis and successful treatment, without assessment of the probable causes.
[1]. Roy FH, Ocular Differential Diagnosis 2007 8th edUSAFEP International:212-213. [Google Scholar]
[2]. Mahendradas P, Avadhani K, Anandula V, Shetty R, Unilateral conjunctival ulcer due to Stenotrophomonas maltophilia infectionIndian J Ophthalmol 2012 60(2):134-36. [Google Scholar]
[3]. Kankski JJ, Bowling B, Kanski’s Clinical Ophthalmology-A Systematic Approach 2016 8th edLondonElsevier:200:201 [Google Scholar]
[4]. Jain AK, Sukhija J, Chopra I, Sachdev N, Primary conjunctival herpetic geographic ulcer in an immunocompetent patientAnn Ophthalmol 2007 39(1):67-69. [Google Scholar]
[5]. Zamir E, Bodaghi B, Tugal-Tutkun I, See RF, Charlotte F, Wang RC, Conjunctival ulcers in Behçet’s diseaseOphthalmology 2003 110(6):1137-41. [Google Scholar]
[6]. Hegab SM, al-Mutawa SA, Conjunctival ulcer in a patient with Crohn’s diseaseOphthalmic Surg 1994 25(9):638-39. [Google Scholar]
[7]. Salamon SM, Mondino BJ, Zaidman GW, Peripheral corneal ulcers, conjunctival ulcers, and scleritis after cataract surgeryAm J Ophthalmol 1982 93(3):334-37. [Google Scholar]