Assessing the Viability of Hadad Flap by Postoperative Contrast-Enhanced Magnetic Resonance Imaging
Hegde Jyotirmay1, Sunil Kumar Saxena2, AS Ramesh3, K Nagarajan4, Shreshta Bhat5
1 Assistant Professor, Department of Ear, Nose and Throat, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
2 Professor and Head, Department of Ear, Nose and Throat, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
3 Assistant Professor, Department of Neurosurgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
4 Additional Professor and Head, Department of Radiodiagnosis, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
5 Assistant Professor, Department of Radiodiagnosis, Pondicherry Institute of Medical Sciences, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyotirmay S Hegde, Assistant Professor, Department of Ear, Nose and Throat, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry-605006, India.
E-mail: jshegdesirsi@gmail.com
Introduction
The Expanded Endonasal Approaches (EEAs) have been widely used for various skull base lesions. The reconstruction of the skull base defects is of vital importance to prevent postoperative complications. The vascular pedicled-nasoseptal flap (Hadad-Bassagasteguy flap) is used as a workhorse in reconstruction of majority of the defects.
Aim
The purpose of this study was: (a) To assess the postoperative MRI appearance of vascularised pedicled nasoseptal flap for its viability; (b) To determine the variations in MRI that may suggest potential flap failure.
Materials and Methods
A prospective study of 13 patients was done, who underwent endoscopic skull base surgery with reconstruction using the Hadad-Bassagasteguy flap. Pre-operative MRI was done to assess the size, extent and location of the lesion and a postoperative MRI was done to evaluate flap configuration, enhancement patterns, location, flap thickness and signal intensity characteristics.
Results
The postoperative MRI of all patients showed a detectable flap covering over the skull base defects forming an “open cup” appearance. They were uniformly isointense on T1-weighted/ fat suppressed images to the adjacent nasal mucosa and hyperintense on T2-weighted images. On the MRI scans done after four weeks, all 13 of our patients had enhancing flaps. One flap migrated slightly to the left side; however, there was no Cerebrospinal Fluid (CSF) leak.
Conclusion
Vascular pedicle nasoseptal (Hadad) flaps are being widely used. MRI is a very useful tool in assessing the viability of the flap postoperatively and to evaluate for variations that may suggest potential flap failure.
Endonasal approach, Endoscopic surgery, Hadad-bassagasteguy flap, Nasoseptal flap, Reconstruction, Skull base surgery
Introduction
The vascularised nasoseptal (Hadad-Bassagasteguy) flap has revolutionised the reconstruction of the skull base defects after endonasal endoscopic skull base surgeries. The incidence of postoperative CSF leak has reduced substantially from 20% to 5%. It was originally described by Hadad G and Bassagasteguy L in 2006. It is a vascularised pedicled nasoseptal flap based on the nasoseptal artery. It is considered as the workhorse for the reconstruction of skull base defects because it has a broad arc of rotation with an extensive blood supply with a wide coverage of various skull base defects [1].
The healing process is faster and complete if vascularised flap is used. Hence, the pedicled flaps like pericranial, temporo-parietal fascia and galeo-cranial flaps were used to reconstruct the skull base after craniofacial resection. However, these flaps require an external incision which will make it inappropriate for use in minimal access techniques [2]. This has made the vascularised nasoseptal flap a suitable choice for endoscopic reconstruction of skull base defects. The goals of ideal reconstruction are to separate the nasal from the intracranial cavity along with preservation of the neurovascular function and elimination of the dead space [3].
The purpose of this study was to assess the postoperative MR imaging appearance of vascularized pedicled nasoseptal flap for its viability and failure, and determine the variations in MRI that may suggest potential flap failure.
Materials and Methods
A prospective study was conducted from November 2014 to October 2016 in all the patients who underwent reconstruction of the skull base defects using the vascularised nasoseptal flap after EEAs. The exclusion criteria included all patients in whom MRI was contraindicated and postoperative MRI could not be done due to severe morbidity or very rare mortality conditions. The protocol for this study was approved by Scientific and Ethical Review Board of JIPMER (Jawahar Institute of Postgraduate Medical Education and Research). All the patients had a preoperative MR imaging examination followed by a postoperative MR imaging examination after four weeks. All imaging criteria were in accordance with that of the radiologist. The sequences included on MRI were axial, sagittal and coronal T1 and T2, pre and post contrast fat saturation T1 images and further; all examinations were performed on a 1.5 Tesla MR unit (Seimens, GMBH, Germany). Preoperative and postoperative MR imaging features that were evaluated included flap configuration, enhancement patterns, location, flap thickness and signal intensity characteristics. The reconstruction site was also visualised postoperatively by diagnostic nasal endoscopy.
Results
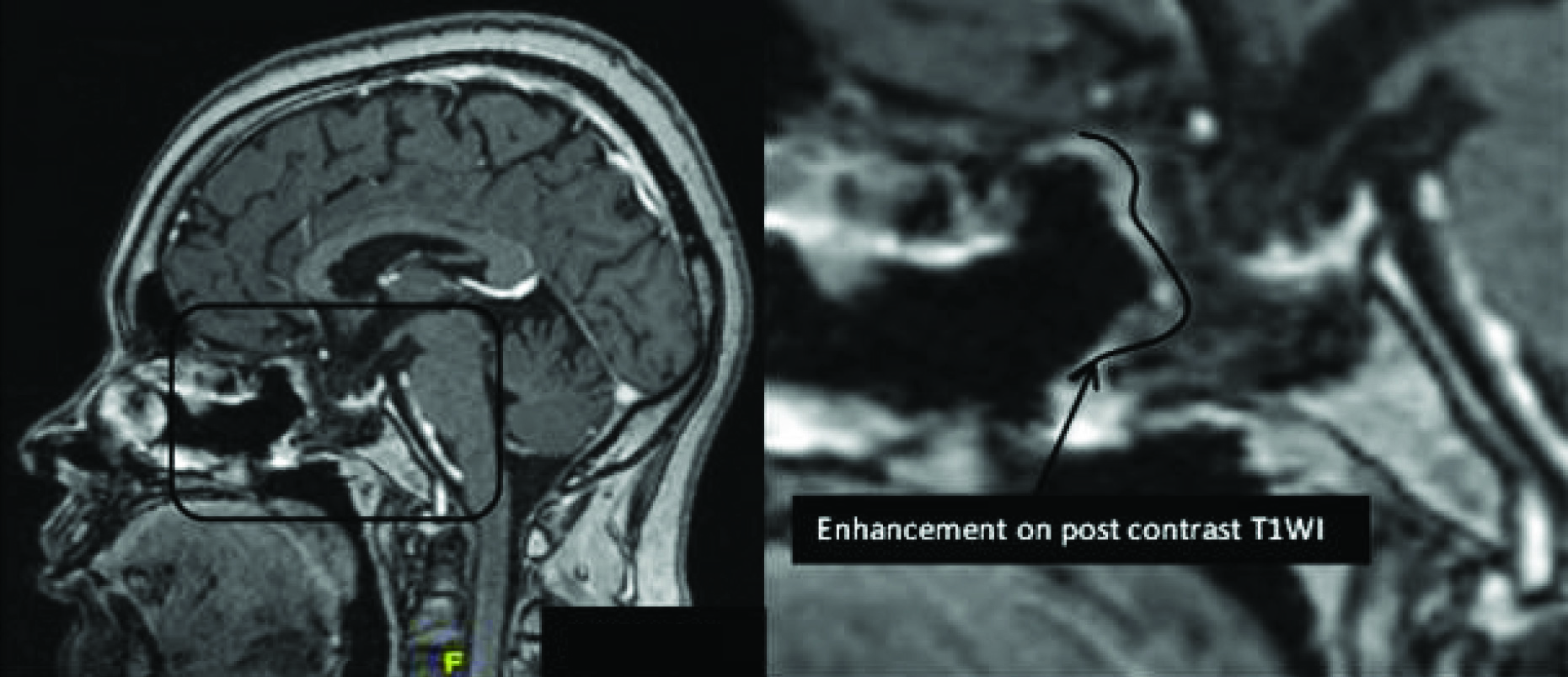
The postoperative MRI of the 13 patients done after four weeks, 12 had detectable flap covering the skull base defects, one of them showed that the flap had migrated slightly to the left. However, there was no detectable CSF leak. On the postoperative MRI scans, the nasoseptal flap in all 13 of our patients showed uniform intensity and enhancement patterns [Table/Fig-1].
The flap shows uniform enhancement on post-contrast T1 WI.
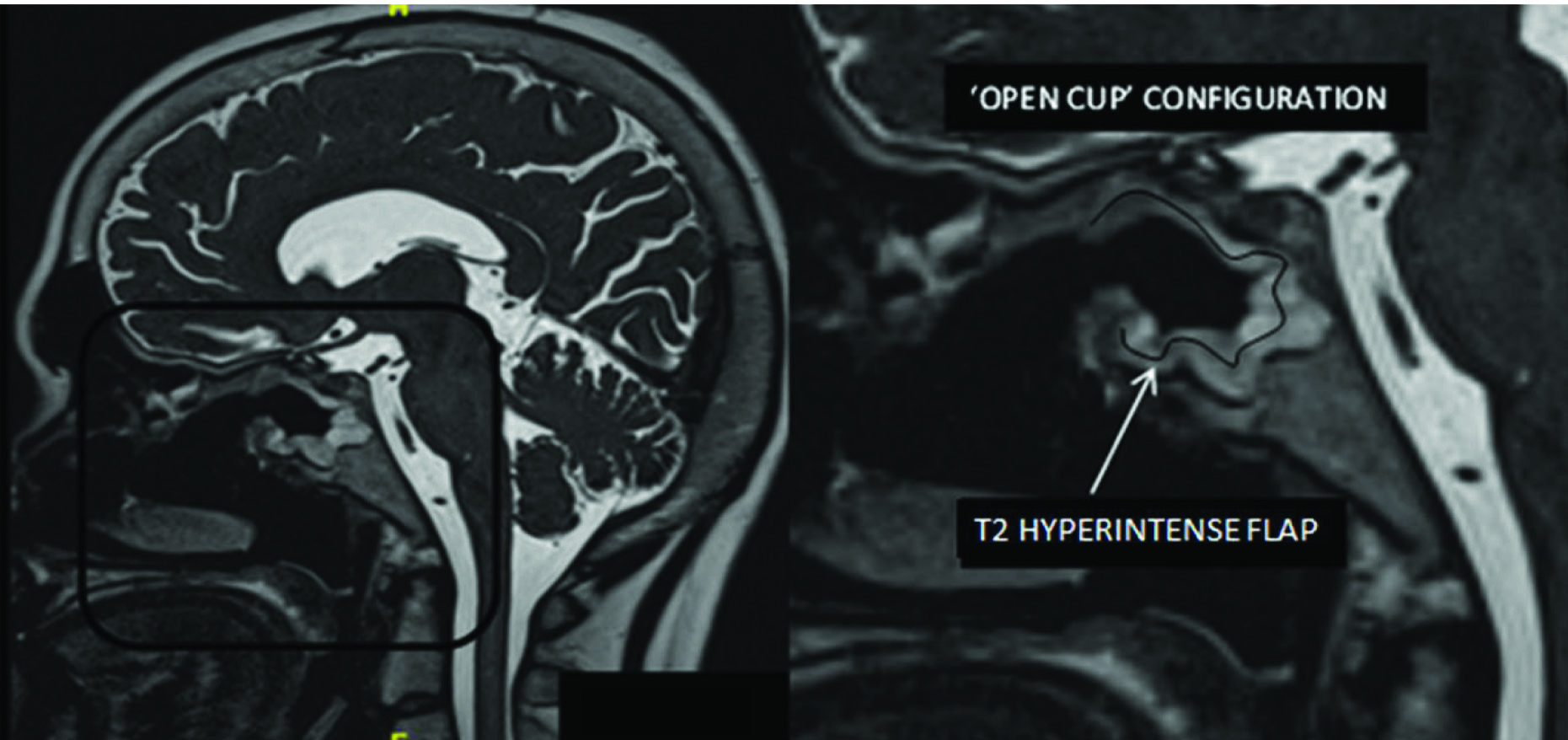
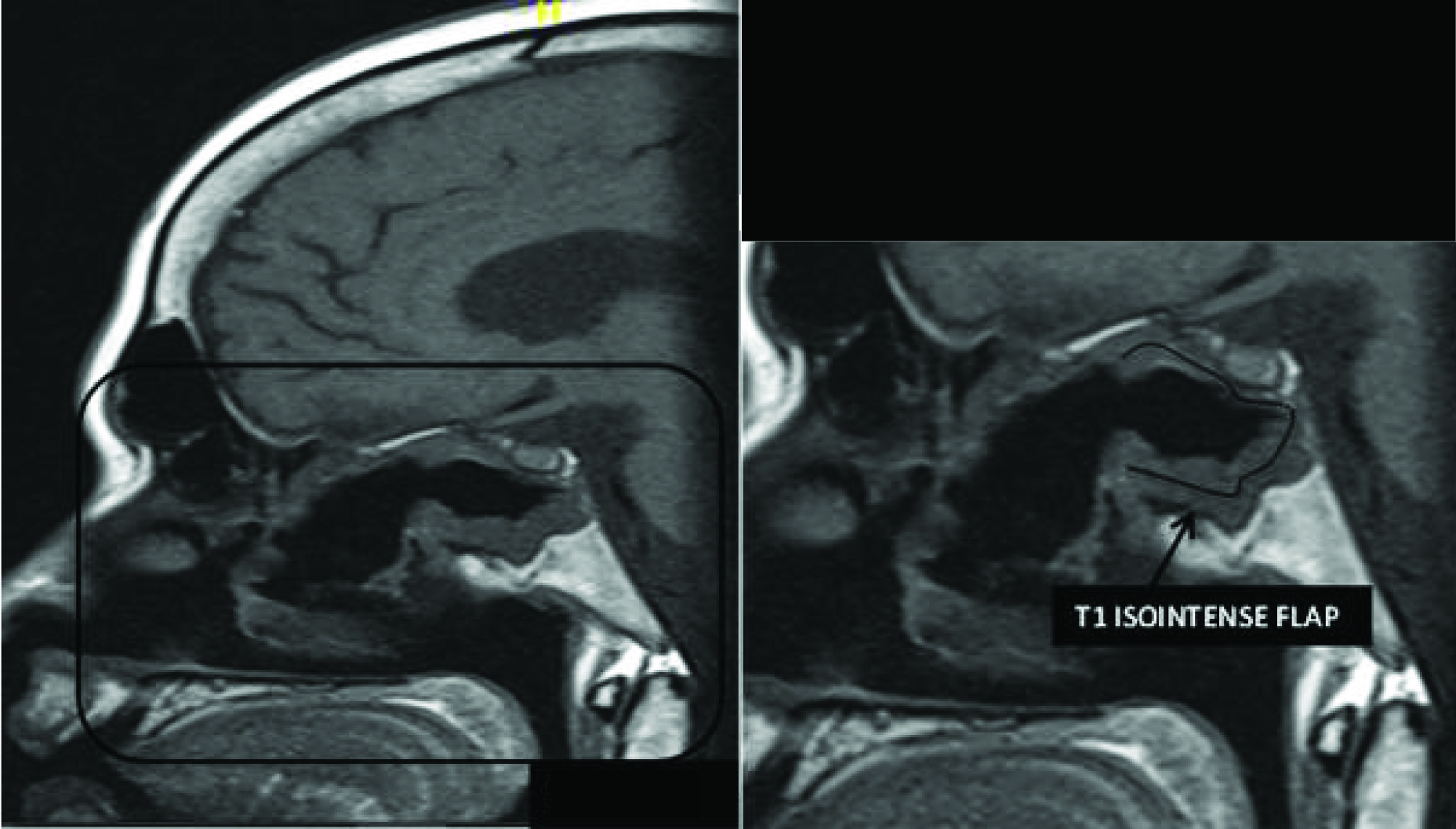
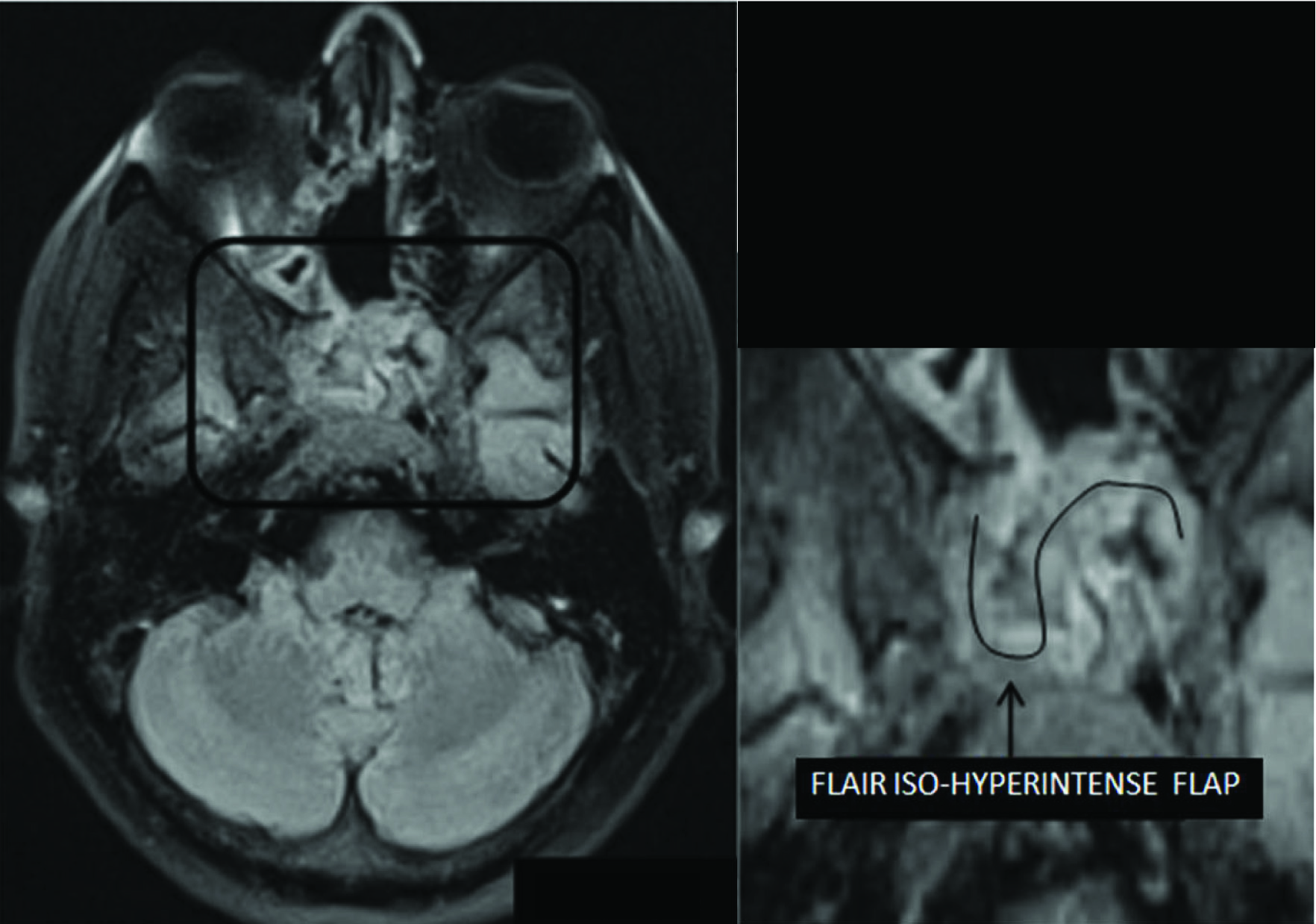
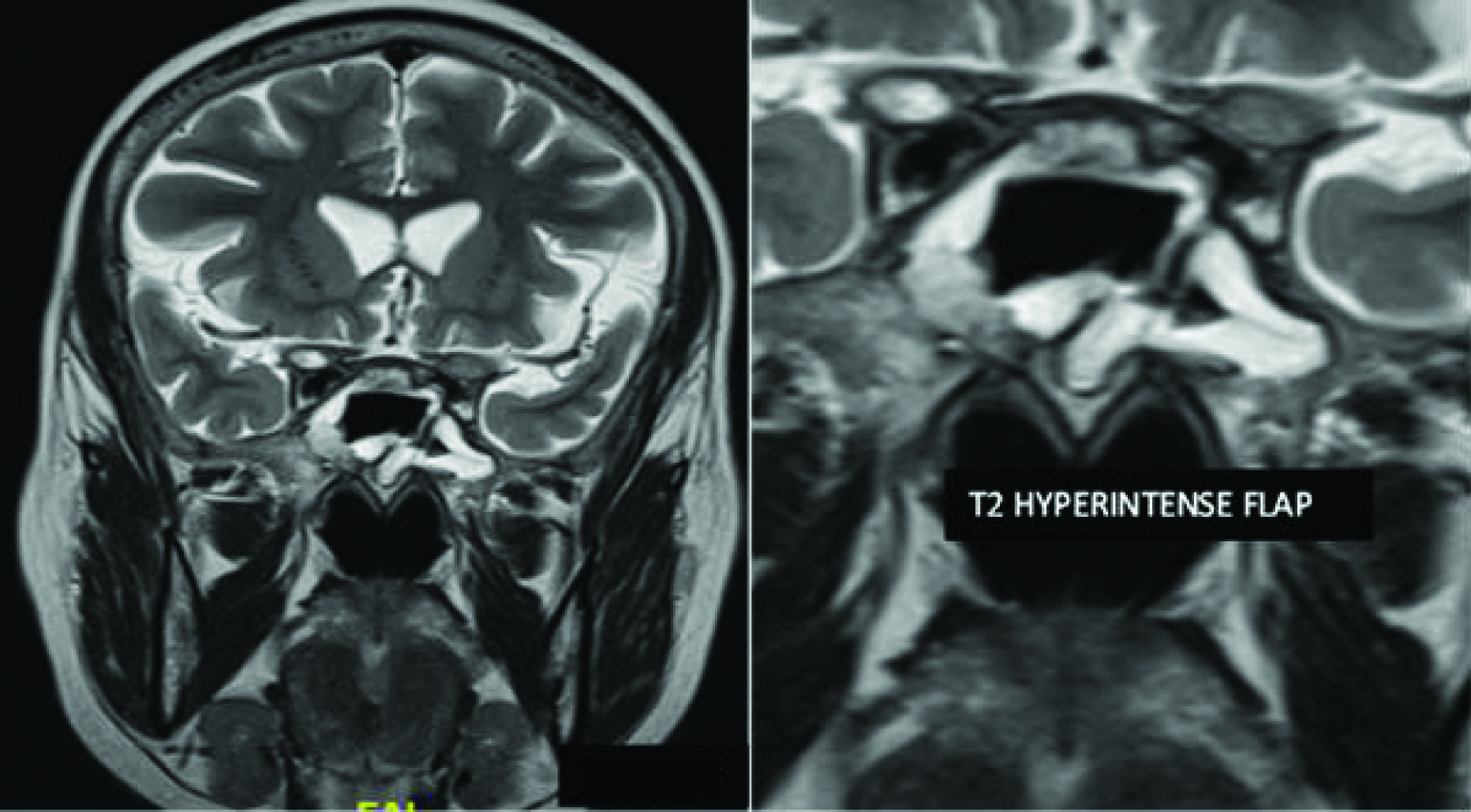
They were hyperintense on T2-weighted images to the adjacent nasal mucosa [Table/Fig-2] isointense on T1-weighted images and iso to hyperintense on FLAIR images [Table/Fig-3,4].
Sagittal T2WI showing the flap along the walls, roof and floor of the sphenoid in an “open cup” configuration along the bony defect.
Sagittal T1WI showing that the flap appears isointense on T1WI.
Flair axial images showing the iso to hyperintense flap outlining the posterior wall of the sphenoid sinus.
They were observed to cover the operative defect, extending along the roof, posterior wall and floor of the sphenoid sinuses forming an “open cup” appearance. Twelve of the thirteen patients who were followed up with a diagnostic nasal endoscopy showed the flaps in situ. One had the flap migrated slightly to the left [Table/Fig-5].
Coronal T2WI at the sphenoid showing the flap migrated to the left lateral wall.
However, previous studies have shown that complications of flap failures or sphenoidal mucocele formation scan occur. This must be kept in mind when assessing a Hadad-Bassagasteguy flap [4].
On the MRI, the thickness of the flaps ranged between 2-7 mm with an average thickness of 3.42 mm [Table/Fig-6]. The length of the flaps ranged between 9.3-12.7 cm with an average length of 10.4 cm. The width of the flaps ranged between 4.4-6.2 cm with an average of 5.3 cm.
Imaging characteristics and enhancement pattern of the vascular pedicle nasoseptal flap on postoperative MR images
| Sl. No. | Pathology For Which Surgery Was Done | Enhancement Postcontrast MRI | Flap Thickness in mm. | Flap Length in cm. | Flap Width in cm. |
|---|
| 1. | Pituitary Macroadenoma | E | 7 | 11.5 | 5.2 |
| 2. | Pituitary Macroadenoma | E | 6 | 12.7 | 4.7 |
| 3. | Pituitary Macroadenoma | E | 3.5 | 10.8 | 4.4 |
| 4. | Pituitary Macroadenoma | E | 3 | 9.8 | 6.2 |
| 5. | Pituitary Macroadenoma | E | 3 | 11.2 | 5.5 |
| 6. | Pituitary Macroadenoma | E | 4 | 10.4 | 6 |
| 7. | Pituitary Macroadenoma | E | 2.5 | 9.7 | 6.1 |
| 8. | Pituitary Macroadenoma | E | 4 | 10 | 5 |
| 9. | Pituitary Macroadenoma | E | 2 | 10.8 | 5.8 |
| 10. | Pituitary Macroadenoma | E | 3 | 10.3 | 4.9 |
| 11. | Pituitary Macroadenoma | E | 2.5 | 9.3 | 4.6 |
| 12. | Craniopharyngioma | E | 2 | 9.6 | 5.1 |
| 13. | Tuberculum sellae meningioma | E | 2 | 10.4 | 5.5 |
E- Uniform enhancement on post contrast images.
The thickness and intensity of the flaps varied with the degree of oedema. Few appeared thicker than the others with increased hyperintensity on T2 weighted images as compared to others due to postoperative oedema.
Discussion
The expanded endoscopic approaches are being increasingly used for the resection of skull base lesions. They can provide access not only to the lesions in the sagittal plane of the skull base and the parasellar region, but to those extending intracranially, as well. The defects created in the skull base leading to communication between subarachnoid space and the nasal cavity have to be reconstructed effectively to avoid postoperative CSF leak [5-8].
Numerous reconstructive techniques have been used to close the defects after EEAs which involve the use of autologous tissue and synthetic substitutes [9-12]. A simple multilayered closure of the defect will suffice in cases of small defects. However, in those cases where the defect is quite big or in cases of high pressure leaks or those cases where significant amount of dura has been excised, a vascularised pedicled flap along with multi-layered reconstruction causes significant reduction in the incidence of postoperative CSF leaks [2].
The use of a septal rotation flap (Hadad flap) for endonasal repair of a CSF leak was first described in the year 1952 by Hirsch O [13]. The vascular pedicled nasoseptal flap or the HB flap is supplied by the posterior nasoseptal arteries which arise from the posterior nasal artery, which is one of the terminal branches of the internal maxillary artery [2]. Its use has led to a sharp decrease in the incidence of postoperative CSF leaks after expanded endoscopic surgery [2,14].
According to Kang MD et al., the enhancement patterns on the immediate (within 48 hours) and delayed postoperative (after 3-7 months of surgery) MRI images can vary [4]. On comparison of the two MRI scans done for the patients, majority of the enhancement flaps were thinner and only few got thicker in the delayed scans. This can thought to be due to contraction/fibrosis or proliferation of granulation tissue in the operative bed or due to increased mucosalization of the flap, respectively. Therefore, enhancement of flap can be evaluated more accurately in an immediate postoperative image than on a delayed image.
Conclusion
Vascular pedicle nasoseptal (Hadad) flaps have been widely used in reconstruction of defects during endoscopic skull base surgeries. MRI is a very useful tool in assessing the viability of the flap postoperatively. It is important to recognize its viability and to evaluate for variations that may suggest potential flap failure.
To the best of our knowledge, this is the first prospective study of assessment of viability of vascularized nasoseptal flap using postoperative MRI.
E- Uniform enhancement on post contrast images.
[1]. Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH, A novel reconstructive technique after endoscopic expanded endonasal approaches:Vascular pedicle nasoseptal flapLaryngoscope 1882–1886 2006 116 [Google Scholar]
[2]. Kassam AB, Thomas A, Carrau RL, Synderman CH, Vescan A, Prevedello D, Endoscopic reconstruction of the cranial base using a pediclednasoseptal flapNeurosurgery 2008 63(1 Suppl 1):ONS44-52.discussion ONS52–3 [Google Scholar]
[3]. Zanation AM, Thorp BD, Parmar P, Harvey RJ, Reconstructive options for endoscopic skull base surgeryOtolaryngol Clin North Am 2011 44(5):1201-22. [Google Scholar]
[4]. Kang MD, Escott E, Thomas AJ, Carrau RL, Snyderman CH, Kassam AB, The MR imaging appearances of the vascular pedicle nasoseptal flapAJNR Am J Neuroradiol 2009 30(4):781-86. [Google Scholar]
[5]. Choby GW, Pinheiro-Neto CD, de Almeida JR, Ruiz-Valdepenas EC, Wang EW, Fernandez-Miranda JC, Extended inferior turbinate flap for endoscopic reconstruction of skull base defectJ Neurol Surg B Skull Base 2014 75(4):225-30. [Google Scholar]
[6]. Carrau RL, Snyderman CH, Kassam AB, The management of cerebrospinal fluid leaks in patients at risk for high pressure hydrocephalusLaryngoscope 2005 115(2):205-12. [Google Scholar]
[7]. Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH, A novel reconstructive technique after endoscopic expanded endonasal approaches:vascular pedicle nasoseptal flapLaryngoscope 2006 116(10):1882-86. [Google Scholar]
[8]. Kassam A, Carrau RL, Snyderman CH, Gardner P, Mintz A, Evolution of reconstructive techniques following endoscopic expanded endonasal approachesNeurosurg Focus 2005 19(1):E8 [Google Scholar]
[9]. Freidberg SR, Hybels RL, Bohigian RK, Closure of cerebrospinal fluid leakage after transsphenoidal surgery (Technical note)Neurosurgery 1994 35:159-60. [Google Scholar]
[10]. Kubota T, Hayashi M, Kabuto M, Takeuchi H, Fuji T, Ohhashi M, Reconstruction of the skull base using a silicone plate during transsphenoidal surgerySurg Neurol 1991 36(5):360-64. [Google Scholar]
[11]. Lee HY, Kim HU, Kim SS, Son EJ, Kim JW, Cho NH, Surgical anatomy of the sphenopalatine artery in lateral nasalwallLaryngoscope 2002 112(10):1813-18. [Google Scholar]
[12]. Seiler RW, Mariani L, Sellar reconstruction with resorbable vicryl patches, gelatine foam, and fibrin glue in transsphenoidal surgery:A 10-year experience with 376 patientsJ Neurosurg 2000 93(5):762-65. [Google Scholar]
[13]. Hirsch O, Successful closure of cerebrospinal fluid rhinorrhea by endonasal surgeryJAMA Arch Otolaryngology-Head & Neck Surgery 1952 56(1):1-12. [Google Scholar]
[14]. Pinheiro-Neto CD, Prevedello DM, Carrau RL, Snyderman CH, Mintz A, Gardner P, Improving the design of the pediclednasoseptal flap for skull base reconstruction:a radio anatomic studyLaryngoscope 2007 117(9):1560-69. [Google Scholar]