Materials and Methods
Present study was a prospective clinical study with minimum follow up period of two years providing level of evidence; class V clinical. All the patients with intertrochanteric fractures admitted at a tertiary trauma center in India from April 2010 to March 2012 were treated with long PFN (Bombay Ortho). Informed consent was taken for study with the Ethical standards of the 1964 Declaration of Helsinki as revised in 2000. Fracture classification used for inclusion criteria was modified Evan’s classification [19,20].
Stable
Undisplaced 2 parts
Displaced but reducible
Unstable
Posterolateral instability with communited Greater Trochanter (GT)
Medial instability with communited Lesser Trochanter (LT)
Both
All the fracture which were more than one-week-old and fractures of reverse oblique variety or with completely broken lateral wall were excluded from the study.
Preoperative data sheet included fracture classification, age, mobility, Harris hip score [21] and co-morbidity.
Surgical technique included closed reduction and PFN. Special technique used for all the fractures was provisional fixation by a 3-3.5 mm Steinmann-pin inserted percutaneously after achieving adequate reduction. In all the surgeries; reduction, Steinmann-pin fixation and PFN were done by the same surgical unit. The technique of Steinmann-pin is helpful even in unstable comminuted fractures in achieving equally good results of PFN. It is not useful for Reverse Oblique fractures (AO/OTA 31-A3). Superiority of PFN in those fractures has already been accepted. Therefore, we have excluded such fractures in our study. It can be used in fracture with subtrochanteric extension but it is difficult to use when lateral wall is completely broken. In AP projection, Steinmann-pin passes from lateral cortex to neck and head region being perpendicular to intertrochanteric fracture line. Pin was kept a bit superior in AP projection and in anterior third of trochanteric and neck region in lateral projection.
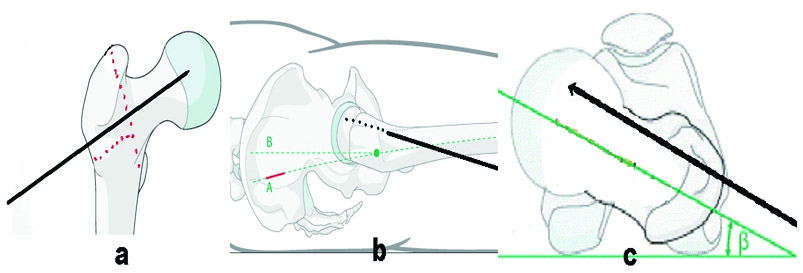
We have learnt over the period that this position of Steinmann-pin avoids collision with reamer or nail by allowing them to pass posteriorly to it due to funnel-shaped geometry of the proximal femoral canal and posterior location of GT in relation to shaft. Steinmann-pin was inserted upto subchondral bone and due care was taken that pin doesn’t pass through fracture or cross anterior or superior neck or subchondral bone. At the site of insertion, anterior placement of Steinmann-pin was ensured clinically by sliding the pin over circumferential surface before deciding final insertion point and radio logically as well. It was withdrawn when inferior lag screw crossed the fracture line [Table/Fig-1,2].
Technique of provisional fixation by Steinman pin [Redrawn from AO Foundation Surgery Reference]: a) Hold the fracture fragments in AP view; b) Keep the pin anteriorly in latoral view; c) Axial view.
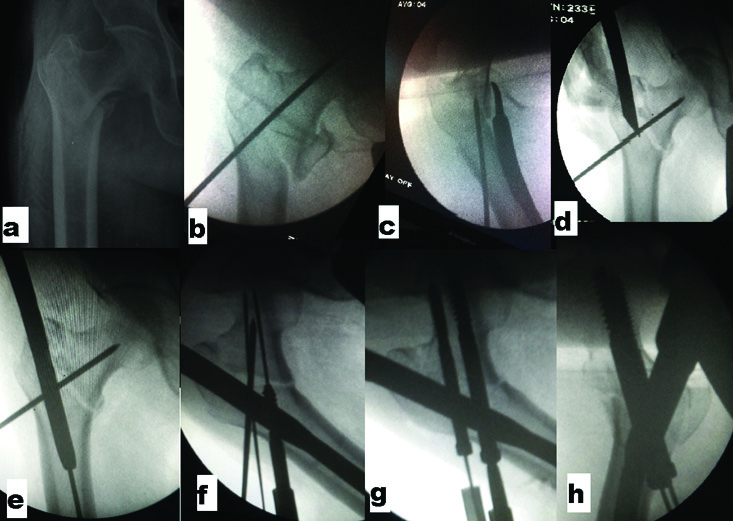
Step by step guide of Steinman pin technique: a) PreoperativeX-Ray; b) Steinman pin fixation in AP view; c) Lateral view; d) Entry by cannulated awl; e) Passage of nail over guide wire behind anteriorly placed pin maintaining reduction; f) Guide pin insertion; g) Lag screw placement after removing Steinman pin; h) Compression by final tightening of screws after releasing traction.
The intraoperative findings recorded were surgical time, blood loss and technical difficulties. Postoperative findings recorded were complications, mobility, shortening, Harris hip score at two years and radiological union, neck shaft angle and implant status.
Statistical Analysis
Statistical analysis was performed using Chi Square statistics for nonparametric data using the two-tailed Fisher-exact test.
Results
Five patients out of 55, died before completing the scheduled 2 years follow up, hence were excluded. Mean age of patients was 71 ranging from 58-95. As per Evan’s classification, there were four type 1 fractures, fifteen type 2 fractures (19 stable), thirteen type 3 fractures, eight type 4 fractures and ten type 5 fractures (31 unstable).
Functional outcome with two year Harris hip score showed almost near return to preinjury score (average 91 versus 97) though preinjury scores are retrograde and not reliable. All fractures showed union within six months except six which united by nine months. A total of 48 out of 50 patients had good abductor strength including those with trochantric communition. Mean neck shaft angle achieved post reduction was 132.4° and at final follow up was 131.1°. Only one patient had shortening of more than 2 cm (20 mm) with an average shortening of 3. 6 mm. Average duration of surgery was 97 minutes. None of the patients developed infection including eight diabetics. Two patients with Colles fracture and one with head injury recovered well with respective treatment.
We compared the results of stable with unstable fractures. Shortening was not significant (Mean 2.2 mm in stable and 4.6 mm in unstable). Neck shaft angle was also well maintained (Mean 133° in stable and 130° in unstable). Average Harris Hip Score in stable fractures was 94 versus 88 in unstable with an average score of 91 [Table/Fig-3].
Comparison of results in stable and unstable fractures.
| Parameters | Stable fracture | Unstable fracture |
|---|
| No. of patients | n=19 | n=31 |
|---|
| Intra operative complications | Difficult reduction | 0 | 5 |
| Varus collapse | 0 | 1 |
| Trochantric translation | 0 | 2 |
| Trochanteric widening | 1 | 1 |
| Trochanteric communition | 1 | 0 |
| Post-operative complications | Superior cortex cut-through | 0 | 1 |
| Varus collapse | 0 | 2 |
| Screw back-out | 0 | 1 |
| Z effect | 0 | 1 |
| Union | All united | All united (3 delayed) |
| Walking | Unaided: 16Stick: 2Walker: 1 | Unaided: 9Stick: 16Walker: 4Not walking: 2 |
| Average difference with preinjury Harris Hip Score | 4 | 10 |
| Mean shortening | 2.2 mm | 4.6 mm |
| Mean neck shaft angle | 133° | 130° |
| Average abductor power | Grade 5 | Grade 4+ |
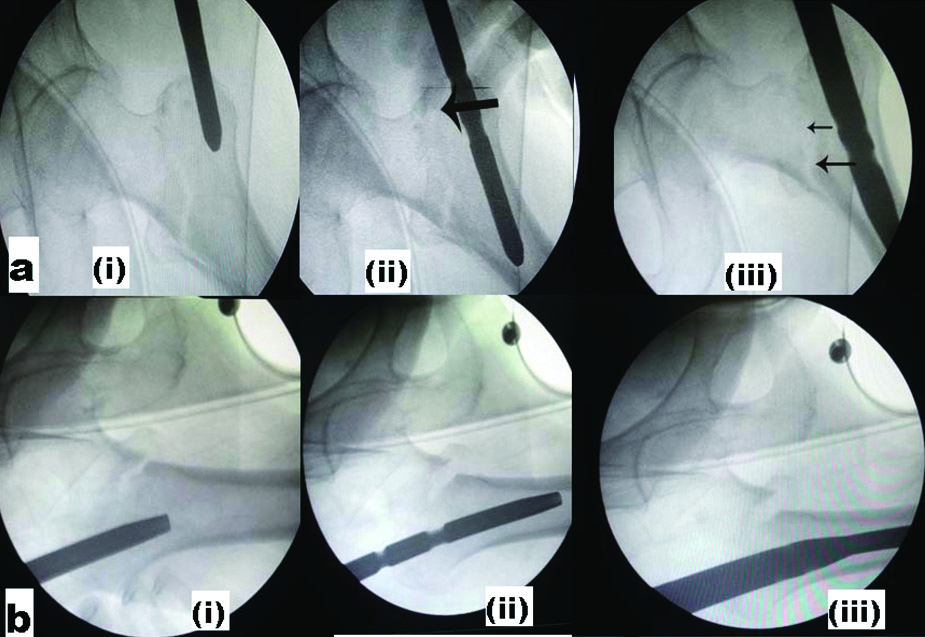
Technical difficulties faced during surgery included difficulty in closed reduction requiring maneuver by spike in five patient, loss of reduction with varus collapse in one patient, intertrochanteric translation (described below) in two patients, widening of intertrochanteric area in two patients, trochanteric communition as a result of surgery in one patient. Immediate postoperative radiograph, 46 screws were in the center or inferior position while four were in the superior part of neck on AP projection. Fracture reduction was good in 46 patients, while in four patients we noticed intertrochanteric translation or widening, although neck shaft angle was above 130° in all except two. There were five complications. Superior screw missing the nail in one patient where 6.5 mm Cannulated Cancellous (CC) screw inserted outside nail for derotation which eventually united with shortening. Two patients had fracture united in varus collapse. Two patients needed a reoperation, one for exchange of screw after union due to backed out screws and another removal of derotation screw due to reverse Z effect [Table/Fig-4].
Common avoidable complications of PFN: a) Z effect; b) Reverse Z effect; c) Varus collapse; d) Shortening.

Discussion
Though PFN is technically challenging, with proper technique, gives excellent results. Three most important technical aspects are achieving good non-varus reduction, inserting nail correctly and accurate placement of lag screws. The technique of provisional fixation of fracture fragments by Steinmann-pin significantly helps in all four major steps of PFN which are reduction, entry, nail passing and locking.
The Technical Problems Faced during Surgery
(1) Reduction: Good reduction can be achieved by fracture table with bilateral boot traction. In grossly comminuted four part fracture, posterior sagging of the trochanteric fragment causing excessive anteversion of neck leading to difficulty in passing the nail as well as subsequent hip screw placement [22,23].
It is important to make sure that the patient’s position and traction is adequate. At the time of provisional fixation of fracture fragments with Steinmann-pin, an assistant can be asked to push the trochanteric fracture up with one hand and then press the distal fragment down from the other hand and provisionally fix it with Steinmann-pin. Spike can be inserted to manipulate reduction from a mini incision at the same site for leg screws.
(2) Entry: Standard entry point for PFN is tip of greater trochanter as per Su ET et al., in simple fracture extending to tip of trochanter, it is easy to put guide pin as fracture itself provides entry [24]. But mostly, there is some communition at tip of trochanter or fracture line is not exactly through tip. In fact we have seen fracture extending 3-4 mm lateral to tip of trochanter. Due to this, awl slips or even if an entry is made in tip of trochanter, due to narrow bone bridge lateral to tip of trochanter and medial to fracture line, guide wire and subsequent reamers fall into fracture line thus making the entry lateral to tip of trochanter. Sometimes, there is an additional coronal split so that there is no lateral support at the entry region. All these things lead to lateral entry of nail and will lead varus fixation [Table/Fig-5].
Difficulty in entry and nail passage: a) Actual entry point; b) Laterally displaced entry through fracture; c) Opening up of trochanter with varus stress at subtroch region.
An important technical aspect here is to start the entry from tip of trochanter and slightly anterior in the lateral plane. Provisional fixation with Steinmann-pin provides a stable proximal fragment for entry.
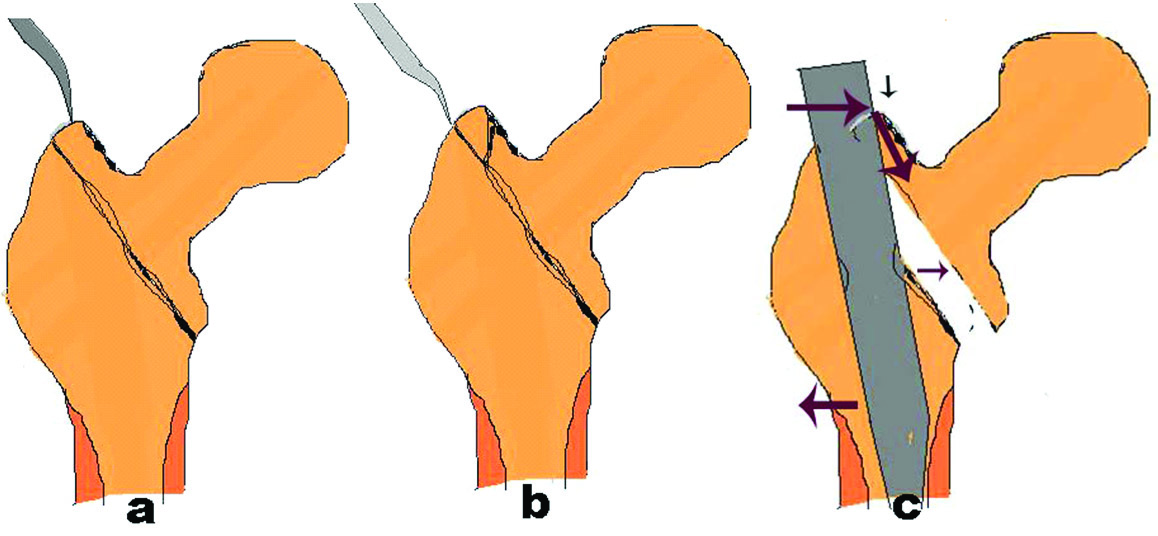
(3) Nail passing: Loss of reduction and possibility of basicervical, subtrochanteric or distal femur fracture while passing the nail is not uncommon. We observed an important phenomenon during nail passage. As the broader portion of nail passes through the intertrochanteric area, loss of reduction occurs. This is a problem not highlighted by any of previous authors although varus reduction due to entry reamer was discussed by Hak DJ et al., [25]. During the passage of the proximal heavy end of nail, the tip of nail hits against medial cortex and manipulating jig medially to pass the nail to central part of canal causes a lever action and pushes the proximal fragment downwards causing some fracture distraction [Table/Fig-6]. This intertrochanteric translation can be associated with varus reduction in one plane and in other plane; it can cause excessive anteversion or parallel anterior sliding of proximal fragment. This phenomenon is likely to cause loss of reduction and may lead to nonunion as well. Although sometimes this translation or distraction can be acceptable in terms of union and seems reducible by compression achieved at the time of final tightening of lag screws, the malreduction in excess of varus or anteversion makes it impossible to place two screws correctly because PFN is a fix angled device unlike different angled barrel option in DHS. Usually it may allow inferior lag screw in proper position but superior one will then be cutting the neck either superiorly in AP or posteriorly in lateral view leading to Z effect later.
Sequential intertrochanteric translation during nail passing a) AP view; b) LAT view (i) Nail entry (ii) Tip touching antero-medial cortex (iii) Passing of broader proximal nail.
Provisional fixation by Steinmann-pin significantly helps in avoiding such loss of reduction. Slightly anterior entry in the lateral projection, adducting the limb and keeping the jig handle as close to flank as possible is helpful. Use of sandbag under buttock and extension device in jig helps in obese patients. Reaming should be adequately done with entry reamer as suggested by Riehl JT et al., [26].
It is recommended to pass small diameters nail (9 mm in our study) except in subtrochanteric extension because diameter of distal part of nail does not affect the stability while proximal is same in all. Continuous C-arm tracking and monitoring the path until complete insertion especially in lateral projection near knee is helpful in avoiding distal femoral fracture of anterior cortex more common in excessive anterior bow. It is recommended to use shorter nail when you are already anticipating unusual anterior femoral bow.
(4) Locking the nail: Ideal position of the lag screws is in the inferior part of neck in AP and in center in the lateral plane keeping appropriate Tip-to-Apex Distance (TAD) by Baumgaertner MR et al., inferior lag screw acts as compression screw so it is inserted first and superior lag acts as derotation screw [27]. Sometimes derotation screw goes too superiorly or posteriorly and even out of cortex of neck of femur. In literature there are no clear consensus on this though some earlier reports of PFN have given very high cut out rates [3,28,29].
Inferior guide pin should be placed first, superior guide pin usually goes posterior to inferior guide pin, so never accept inferior pin in posterior quadrant and try to keep it central in lateral projection. Provisionally fixed Steinmann-pin in anterior part can be used as reference here. When inferior screw crosses the fracture line, Steinmann-pin should be pulled out and traction should be released to achieve adequate compression. We used only small reamer even for compression screw in most cases to achieve better purchase in osteoporotic bone though minimal hammering of screw is required sometimes while crossing fracture line. Derotation screw should be shorter by at least 15 mm in comparison to compression screw otherwise it could take weight and can back out or migrate into joint leading to cut out explained by Morihara T et al., we recommend dynamic distal locking in all and static locking only in unstable fractures [14].
Guide wires for screw might bend slightly as it reaches subchondral bone or even break especially while reaming. Hence one should avoid using threaded or previously damaged guide pins. In such cases partially ream upto bending and then pull the bended guide wire upto reamer tip and reinsert it in a new track and then ream over it.
Due to cases where problem arise while negotiating the reamer for hip screw through the nail, it is recommended to rule out manufacture or assembly related problems by checking it before surgery. Check for jig loosening. Reaming with smaller sized reamer and proceeding with larger.
In literature, after analyzing failures of PFN, we found that most of these are due to improper techniques, unacceptable reduction, surgery done by junior houseman, failure to anticipate nail touching anterior cortex while hammering and usage of larger screws. Pajarinen J et al., observed that use of PFN has a positive effect on the speed of restoration of walking because of restoration of near normal anatomy whereas in DHS, greater impaction at fracture causes shortening [4]. Al-Yassari G et al., and Simmermacher RKJ et al., also found restoration of preoperative mobility in approximately half of the patients treated with PFN [28,29]. Ballal MSG et al., found 5% PFN failures and observed that acceptable reduction and proper technique were not ensured in most of the failed PFN done by residents [9].
Our study supports these findings, as all fractures were united mean shortening of 3.6 mm (p<0.05). Only one patient had a shortening of more than 2 cm which is quite less than shortening observed with DHS (mean 10.8 mm) by Saudan M et al., [30]. Pajarinen J et al. found higher screw failure rate for PFN but it was mentioned that screws were placed more superiorly in such group [4]. In all except one, neck shaft angle greater than 130° was achieved and also maintained in the final follow up with mean of 131.1°(p<0.01). Average Harris Hip Score was 91 after two year. We did not encounter any disastrous complication like Z effect causing migration of derotation screw into joint or acetabulum or total implant failure which was more frequently encountered previously before provisional fixation by Steinmann-pin technique was used in author’s hospital.
Our study highlights the technical details regarding PFN but small sample size and lack of paired comparison with PFN done without provisional fixation techniques are surely the limitations of the study. We also believe that now the era has come that those institutions which exclusively practice PFN in trochanteric fractures come up with more studies based on PFN technique.
Conclusion
From the above results, we conclude that it is more of technical failure rather than failure of implant in case of PFN. If properly done, PFN gives superior results. Although anatomical reduction might not be possible in unstable fracture but even if neck shaft angle and version are maintained with medial continuity and hip screws are placed centrally, irrespective of communition and nonanatomical reduction, fracture will unite with minimal shortening. These two factors are like two sides of a coin as screw placement angle is prefixed, so without proper neck shaft angle and version, it is not possible to insert the lag screws properly. Provisional fixation of fracture by Steinmann-pin technique can be really helpful in addressing these requirements. Provisional fixation of fracture by Steinmann-pin after achieving a good reduction between two main fragments helps significantly in maintaining it without varus malalignment till insertion of lag screws in a proper position and reduces technical complications.