Multifocal Tubercular Dactylitis: A Rare Presentation of Skeletal Tuberculosis in an Adult
Pravat Thatoi1, Manoj Parida2, Rakesh Barik3, Bidyut Das4
1 Assistant Professor, Department of Medicine, SCB Medical College, Cuttack, Odisha, India.
2 Senior Resident, Department of Medicine, SCB Medical College, Cuttack, Odisha, India.
3 Postgraduate Student, Department of Medicine, SCB Medical College, Cuttack, Odisha, India.
4 Professor, Department of Medicine, SCB Medical College, Cuttack, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pravat Thatoi, Flat-104, Aryabhatta Complex, College Square, Cuttack-753003, Odisha, India.
E-mail: drpravatthatoi@yahoo.co.in
Tubercular dactylitis is an uncommon form of osteo-articular tuberculosis seen in children. Multifocal involvement, simultaneously involving hands and feet is extremely uncommon. Here we report an adult patient with tubercular dactylitis involving multiple digits of both hands and second digit of right foot in absence of any risk factors like immunodeficiency or any debilitating condition. The patient was successfully treated with anti-tubercular drugs for six months. Mycobacterium tuberculosis infection of bones and joints can present in an unusual way but early diagnosis and treatment caries a good prognosis.
Mycobacterial infection, Osteo-articular tuberculosis, Spina ventosa
Case Report
A 30-year-old male presented with pain and swelling of right second toe followed by pain and swelling of thumb, index and little fingers of left hand, and index and little fingers of right hand for six months. The patient was apparently asymptomatic six months back when he noticed mild pain and swelling of right second toe for which he took symptomatic treatment from a local doctor without improvement. After one month, he developed multiple swellings involving thumb, index and little fingers of left hand and index and little fingers of right hand simultaneously for which he took multiple analgesics and antibiotics from local doctors without any improvement. The swellings were progressively increasing in size. He developed a sinus over right index finger which was due to attempted fine needle aspiration at a local hospital. He denied any history of cough, expectoration, chest pain, anorexia, loss of weight or night sweats. He had no history of intravenous drug abuse, prior blood transfusion or high risk behaviour. None of his family member was suffering from tuberculosis.
On general examination, he was afebrile (temperature <37°C), with no pallor, icterus and lymphadenopathy. He had pulse rate of 72/minute and blood pressure of 120/80 mmHg. The swellings were fusiform in shape and firm to hard in consistency involving proximal half of right second toe, thumb, index and little fingers of left hand and also involving index and little fingers of right hand [Table/Fig-1]. There was mild increase in local temperature and tenderness on deep palpation along with restricted movement of the affected fingers. His cardiovascular, pulmonary, abdominal and neurological examinations revealed no abnormality.
Image showing swelling of right second toe, index and little fingers of both hands and left thumb.

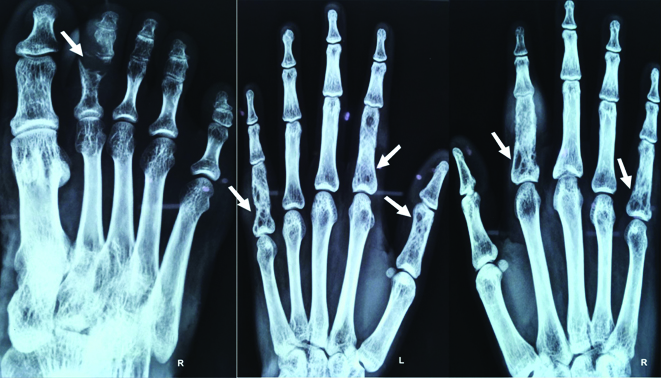
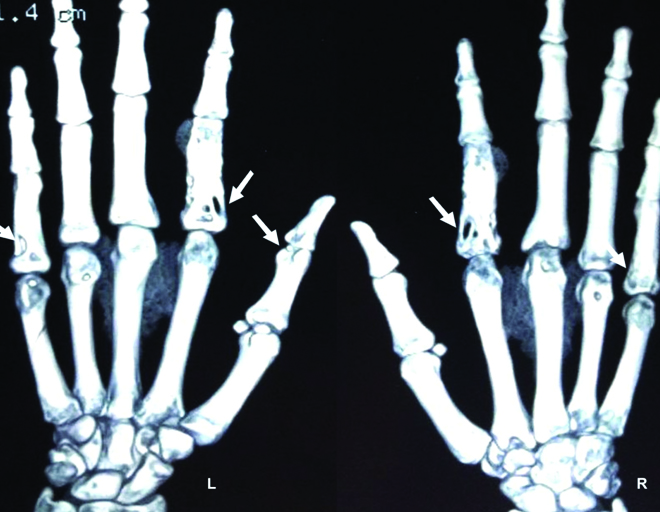
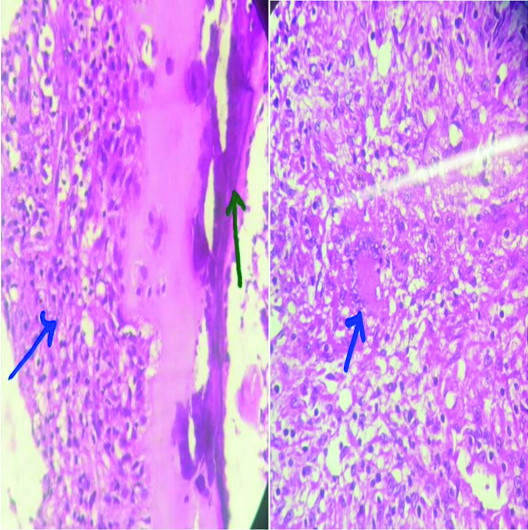
His complete blood count showed a hemoglobin of 12.2 gm/dl, total leukocyte count 6800/ mm3 with 56% polymorphonuclear cells, 40% lymphocytes and 4% eosinophils, and platelet count 2,25,000/mm3. Red blood cells were normocytic and normochromic. His Erythrocyte Sedimentation Rate (ESR) was 42 mm in first hour and C - Reactive Protein (CRP) was 22 mg/L. Mantoux test was 18 mm induration. Liver function tests revealed normal bilirubin and normal enzymes. HIV serology was negative with a normal chest x-ray. X-ray of right foot showed soft tissue swelling, involvement of PIP joint and lytic lesions involving proximal and middle phalanges of right second toe with no periosteal reaction. Hand radiographs showed soft tissue swelling and cystic cavities with internal septations involving proximal phalanges of index and little fingers of both hands, and soft tissue swelling and a lytic lesion over proximal phalanx of left thumb [Table/Fig-2]. The CT-scan of hands showed similar changes and a lytic lesion over proximal phalanx of left thumb [Table/Fig-3], suggestive of dactylitis. Histopathology study from incisional bone biopsy of right second toe demonstrated caseating granulomas, chronic inflammatory cellular infiltrations, epithelioid cells and Langhans type of giant cells suggestive of tubercular infection [Table/Fig-4]. The Ziehl-Neelsen (Z-N) staining from the lesion was positive for Acid Fast Bacilli (AFB) and the Polymerase Chain Reaction (PCR) test from incisional bone biopsy was positive for Mycobacterium tuberculosis which confirmed tubercular dactylitis.
Radiographs of right foot and both hands showing lytic lesions involving proximal and middle phalanges of second toe (arrow) and cystic cavities with septations involving proximal phalanges of index and little fingers of both hands (arrow), a lytic lesion over proximal phalanx of left thumb (arrow).
CT scan of both hands showing cystic cavities and septations involving proximal phalanges of index and little fingers of both hands (arrow). A lytic lesion over proximal phalanx of left thumb (arrow).
Histopathology study showing (right) lamellar bone with underlying chronic inflammatory cellular infiltration and (left) Langhans type of giant cell with epithelioid histiocytes and lymphocytes in the background.
The patient was treated with a four-drug anti-tubercular therapy consisting of isoniazid (300 mg daily), rifampicin (600 mg daily), ethambutol (800 mg daily) and pyrazinamide (1500 mg daily) for two months followed by two drugs i.e., isoniazid (300mg daily) and rifampicin (600 mg daily) for another four months, based on his body weight.
He was followed up every month for first six months and then final follow up after one year. There was substantial decrease in swelling and restriction of finger movements after two months of anti-tubercular treatment and complete remission of symptoms and signs after six months of therapy [Table/Fig-5]. No adverse drug reaction was noted during the course of treatment.
Completely healed lesions after six months of anti-tubercular treatment.

Discussion
Musculo-skeletal tuberculosis is uncommon, involving only 1%-3% of all cases of tuberculosis [1]. Tubercular dactylitis is an uncommon form of osteo-articular tuberculosis due to Mycobacterium tuberculosis infection of short and tubular bones of hands and feet usually seen in children [2]. There are areas of bone destruction in one or more phalanges that expand from within giving appearance of a wind filled sail called ‘spina ventosa’. Radiologic pictures typically show soft tissue swelling, periosteal reaction and bone destruction. Sequestration, sinus tracts, spina ventosa and multifocal involvement are typically seen in children and are rare in adults [3]. In our case, a 30-year-old patient was having multifocal dactylitis involving both hands and right foot which is extremely uncommon. Literature search showed only four cases had tubercular dactylitis involving both hand and foot [4]. The diagnosis of tubercular dactylitis is often delayed due to its close resemblance with other causes of dactylitis clinically and radiologically. But early diagnosis and treatment can cause complete cure of the disease. In tubercular dactylitis, proximal phalanges and metacarpals of hands are more often involved followed by short bones and phalanges of feet. Pain and swelling of digits are the most common clinical presentations [5].
Tubercular dactylitis has to be differentiated from pyogenic dactylitis where local temperature is increased with severe tenderness of the affected digits associated with high fever. Psoriatic dactylitis is another differential diagnosis where sausage shaped fingers, presence of typical skin lesions, nail changes and asymmetrical polyarthritis is observed [6]. In reactive arthritis, dactylitis is also sausage shaped associated with enthesopathy, sacroiliitis and asymmetric oligo-arthritis. There may be eye changes like episcleritis, scleritis and anterior uveitis seen in reactive arthritis patients [7]. Primary bone tumors like multiple enchondromas can have multiple swellings involving hands and feet with unique histopathology study and there may be evidence of pathological fractures [8]. Fungal dactylitis is a rare condition, where there is fungal infection of hands and feet with cellulitis, skin ulcers and draining sinuses [9]. Diagnosis of tubercular dactylitis needs to be confirmed by biopsy, histopathology study, and demonstration of AFB by Z-N stain or culture and also by Mycobacterium tuberculosis PCR. The treatment with appropriate anti-tubercular drugs for six months i.e., combination of rifampicin (R), isoniazid (H), pyrazinamide (Z) and ethambutol (E) for two months and combination of rifampicin (R) and isoniazid (H) for another four months leads to complete remission [10].
Conclusion
Tubercular dactylitis is an uncommon form of osteo-articular tuberculosis seen in children. Multifocal involvement of both hands and foot in an adult is extremely rare. Proper clinical examination, high index of suspicion and routine x-rays of the affected sites provide clues to the diagnosis which needs to be confirmed by histopathological examination or demonstration of AFB by Z-N stain or PCR. Tubercular dactylitis is completely curable with proper anti-tubercular therapy, which was evident in our patient.
[1]. Davidson P, Horrowitz I, Skeletal tuberculosisAm J Med 1970 48:77-84. [Google Scholar]
[2]. John BM, Muthuvel S, Gupta S, Multicentric tubercular dactylitisMJAFI 2007 63:186-87. [Google Scholar]
[3]. Chowdhary V, Aggarwal A, Misra R, Multifocal tubercular dactylitis in an adultJ Clin Rheumatol 2002 8(1):35-37. [Google Scholar]
[4]. Ali N, Bhat A, Fatima A, Muzzafar K, Latoo IA, Singh R, Tuberculous dactylitis: a case series and review of literatureJ Pioneer Med Sci 2014 4(4):184-90. [Google Scholar]
[5]. Subasi M, Bukte Y, Kapukaya A, Gurkan F, Tuberculosis of the metacarpals and phalanges of the handAnn Plast Surg 2004 53(5):469-72. [Google Scholar]
[6]. Kavanaugh A, Helliwell P, Ritchlin CT, Psoriatic arthritis and burden of disease: patient perspectives from the population-based multinational assessment of psoriasis and psoriatic arthritis (MAPP) surveyRheumatol Ther 2016 3:91-102. [Google Scholar]
[7]. Lozada C, Schwartz R, Carpintero M, Reactive arthritisMedscape [Internet] 2015 Oct[cited 2016 Wed 19]Available from: http://emedicine.medscape.com/article/331347-treatment [Google Scholar]
[8]. Sun TTT, Keung IF, Wong TC, Leung POY, Chan JSY, Enchondroma of the hand: result of surgery curettage and grafting and possible factors affecting the outcomeJournal of Orthopaedics, Trauma and Rehabilitation 2017 22:13-17. [Google Scholar]
[9]. Gelman M, Everts C, Blastomycotic dactylitisRSNA [Internet] 1973 May[cited 2016 Sat 15]107(2)Available from: http://pubs.rsna.org/doi/abs/10.1148/107.2.331 [Google Scholar]
[10]. Sandher D, Al-Jibury M, Paton R, Ormerod L, Bone and joint tuberculosisJ Bone Joint Surg [Br] 2007 89-B:1379-81. [Google Scholar]