MRI findings of Persistent Mullerian Duct Syndrome: A Rare Case Report
Rambir Singh1, Sunil D Kumar2, Nidhi Aggarwal3
1 Assistant Professor, Department of Radiology, American International Institute of Medical Sciences, Udaipur, Rajasthan, India.
2 Resident, Department of Radiology, Rnt Medical College, Udaipur, Rajasthan, India.
3 Resident, Department of Radiology, Rnt Medical College, Udaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nidhi Aggarwal, RNT Medical College, Chetak Circle, Udaipur, Rajasthan, India.
E-mail: nidskims@gmail.com
Embryologically mullerian duct derivatives lead to formation of female genitalia and wolffian duct derivatives to male genitalia. Presence of mullerian duct derivatives in a chromosomally normal male (XY) leads to male pseudohermaphroditism and is referred to as Persistent Mullerian Duct Syndrome (PMDS). A young male patient with bilateral cryptorchidism presented to our hospital who was subsequently imaged. There are many case reports of persistent mullerian duct syndrome but they focus mainly on surgical aspects. In this article, MRI features of persistent müllerian duct syndrome are presented.
Cryptorchidism, Karyotyping, Mullerian Inhibiting Factor (MIF), Orchid, Pseudohermaphroditism
Case Report
A 22-year-old unmarried male patient presented with undescended testes. Vitals were within normal limits. On clinical examination testes were not palpable in the scrotal sac. Penis and urethra were unremarkable. The secondary sex characters like moustache, beard, pubic and axillary hair were found to be well developed. The patient had a history of left orchidectomy for undescended testis done 15 years back. The details of the surgery were not available.
Ultrasonography of pelvis showed a hypoechoic structure, posterior to the urinary bladder. Right testis was not visualized in right scrotal sac. Left testis was not visualized (history of orchidectomy).
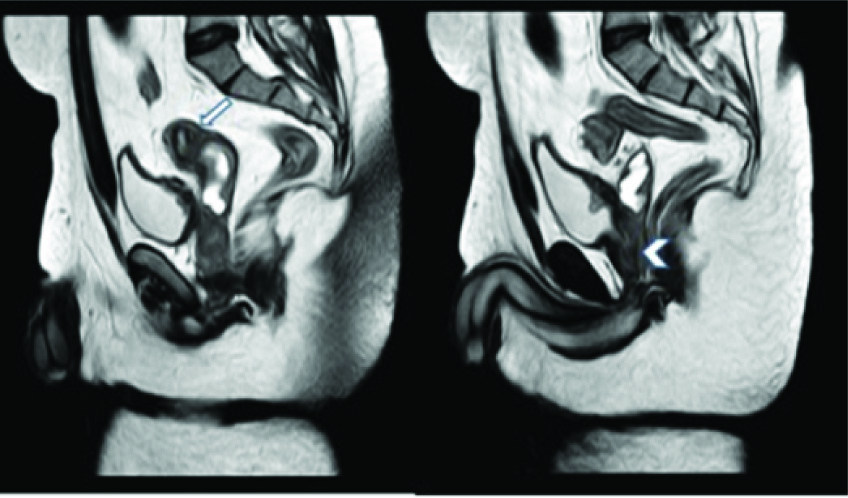
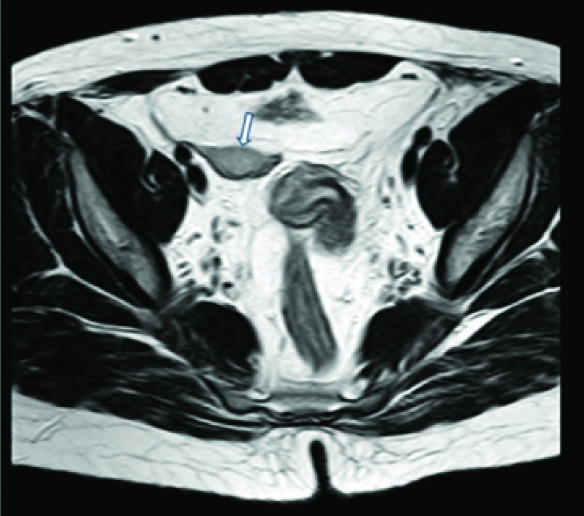
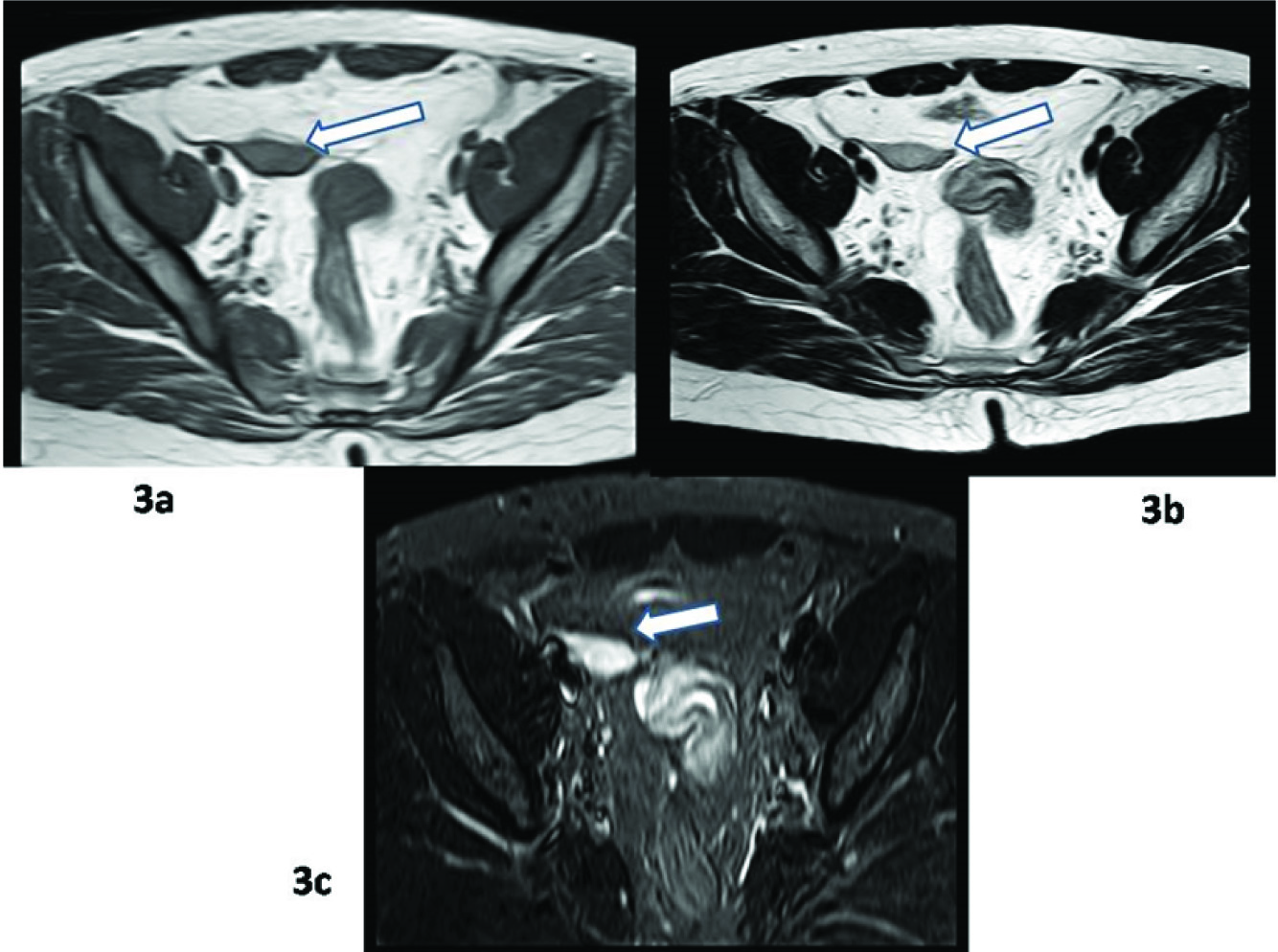
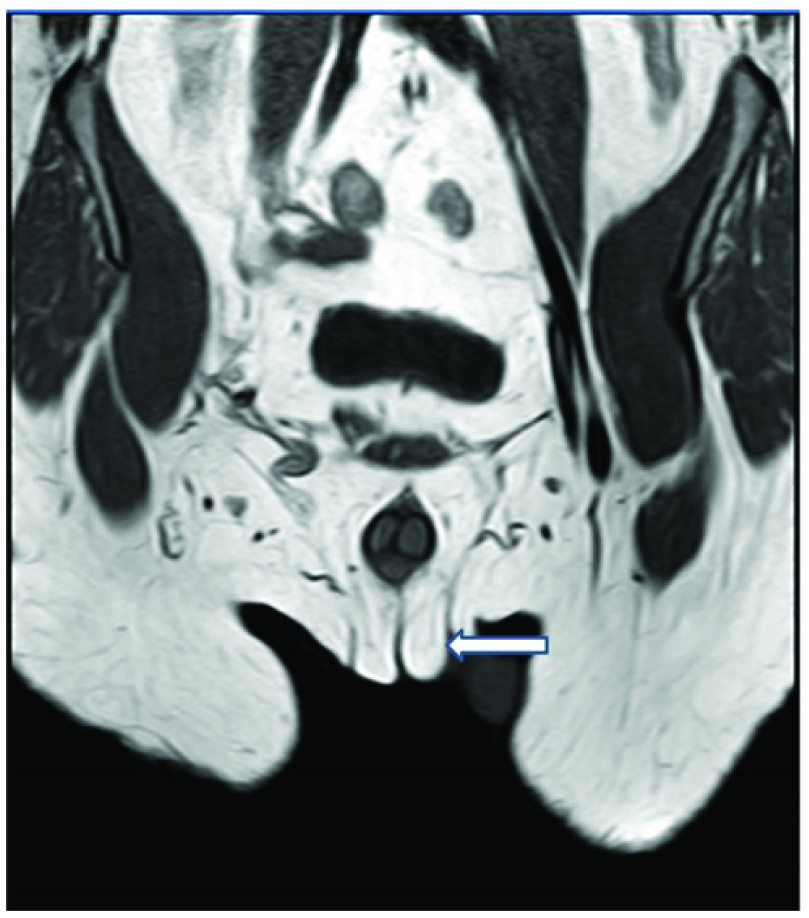
Patient was referred for MRI. MRI showed a well formed uterus and cervix with well defined three zones and blind ended upper third of vagina posterior to bladder. The vaginal part and endocervical canal were distended with fluid. Minimal amount of fluid was seen in endometrial cavity. The upper third vagina appeared to be attached to posterior surface of prostate [Table/Fig-1a,b] [Table/Fig-2]. An oval structure measuring 33 x 21 x 13 mm with morphology and signal intensity consistent with testis appearing hypointense on T1WI [Table/Fig-3a], intermediate on T2WI [Table/Fig-3b] and hyperintense on STIR [Table/Fig-3c], was seen in the right hemipelvis, lateral to the uterus and medial to the iliac vessels. Left testis was not visualised. A fluid filled small sac like structure was seen in the right inguinal canal [Table/Fig-4]. No structure consistent with ovarian morphology was seen. Prostate appeared normal in size and morphology. There was agenesis of bilateral seminal vesicles. These findings in MRI were consistent with PMDS. Patient was referred for surgery. However, patient refused any surgical intervention.
Sagittal T2 weighted MRI Image shows a well formed uterus and cervix (arrow in (a)) with well defined three zones and upper one third of vagina posterior to bladder attached to prostate (arrowhead in (b)). The vaginal part and endocervical canal are distended with fluid.
Axial T2 weighted image shows uterus with three zones and right testis (arrow) lateral to it.
Axial T1 Weighted, T2 weighted and STIR sequence MRI images show well defined oval shaped structure in right hemipelvis (arrow) lateral to uterus consistent with right testis.
Coronal T1 weighted MRI image shows fluid filled sac like structure in right inguinal region. The scrotal sacs were empty (arrow).
Discussion
PMDS is a rare form of internal male pseudohermaphroditism, characterized by the presence of mullerian duct derivatives (uterus and fallopian tubes) in genotypically normal males [1]. The cause is either absence of Antimullerian Hormone (AMH), also called as MIF, or abnormal AMH, as well as defects in its receptor. Human gene for AMH has been mapped to Chromosome 19 [2]. PMDS patients are both karyotypically and phenotypically normal with normal development of secondary sexual characters [3]. Our patient also had well developed secondary sexual characters. AMH levels were not measured as they are known to be undetectable after puberty.
Two anatomic variants of PMDS have been described. The more common variant is the male form, encountered in 80-90% of cases and characterized by one normally descended testis with herniation of either ipsilateral fallopian tube and uterus (hernia uteri inguinalis) or contralateral testis and tube (crossed testicular ectopia) into the hernial sac. The second less common female type, is seen in only 10-20% of cases and is characterized by bilateral cryptorchidism, with the uterus fixed in pelvis and both testis embedded in round ligaments [3]. In our case, with left orchidectomy done for cryptorchidism and now MRI detection of right testis and uterus in pelvis suggest female type of PMDS.
Although, PMDS was first described by Nilson in 1939, till now only 100 cases are described in literature partly due to underreporting [4]. MRI with its multiplanar capabilities has enabled identification of different structures and their relationship to adjacent pelvic organs. Imaging features are characteristic of PMDS. When an elongated tubular structure is identified behind the urinary bladder in a male with normal external genitalia, the diagnosis of this rare syndrome can be made [5]. In our case also, MRI showed a well formed uterus and cervix with well defined three zones and blind ended upper third of vagina posterior to bladder. Right testis was seen in the right hemipelvis and lateral to the uterus. Prostate was normal but attached to upper vagina posteriorly. There was agenesis of bilateral seminal vesicles. This was a rare associated finding.
Early recognition of PMDS is important as there is overall 18% incidence of malignant transformation similar to abdominal testis in otherwise healthy men [6]. After confirming diagnosis, most clinicians recommend removal of persistent mullerian structures with orchidopexy in children or orchidectomy in adults. Care is taken not to damage the vas deferens, if there is some spermatogenesis. These patients are then put on long term follow up. In the present case, patient was advised surgical intervention which he refused. Patient was put on follow up. This case was unique in terms of female variant of PMDS with bilateral agenesis of seminal vesicles which has not been reported earlier.
Conclusion
To conclude, PMDS is a rare disorder usually discovered incidently during operative management of inguinal hernia or undescended testis. Preoperative imaging and familiarity with this disorder in a patient with unilateral or bilateral cryptorchidism will lead to adequate preoperative planning and prevention of complications.
[1]. Yuksel B, Saygun O, Hengirmen S, Persistent müllerian duct syndrome associated with irreducible inguinal hernia, bilateral cryptorchidism and testicular neoplasia: A case reportActa Chir Belg 2006 106:119-20. [Google Scholar]
[2]. Clemente N, Belville C, Anti-Müllerian hormone receptor defectBest Pract Res Clin Endocrinol Metab 2006 20:599-610. [Google Scholar]
[3]. Dekker HM, de Jong IJ, Sanders J, Wolf RF, Persistent Mullerian duct syndromeRadiographics 2003 23:309-13. [Google Scholar]
[4]. Sheehan SJ, Tobbia IN, Ismail MA, Kelly DG, Duff FA, Persistent mullerian duct syndrome: review and report of 3 casesBr J Urol 1985 57:548-51. [Google Scholar]
[5]. Di Cesare E, De Vincentiis VDB, Maffey MV, Splendiani A, Masciocchi C, US and MRI in a case of persistent müllerian duct syndromePediatr Radiol 1998 28:865-67. [Google Scholar]
[6]. Shamim M, Persistent Mullerian duct syndrome with transverse testicular ectopia presenting in an irreducible recurrent inguinal herniaJ Pak Med Assoc 2007 57:421-23. [Google Scholar]