Congenital Ectropion Uveae with Glaucoma: A Case Report
Rashmi Kumari1, Bhawesh Chandra Saha2, Bibhuti Prasanna Sinha3
1 Senior Resident, Department of Ophthalmology, Regional Institute of Ophthalmology(RIO), Indira Gandhi Institute of Medical Science, Patna, Bihar, India.
2 Senior Resident, Department of Ophthalmology, AIIMS, Patna, Bihar, India.
3 Additional Professor, Department of Ophthalmology, Indira Gandhi Institute of Medical Science, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rashmi Kumari, House No. O-13, Ashiana Nagar Phase-1, Patna-25, Bihar, India.
E-mail: dr.rchandras08@gmail.com
Congenital Ectropion Uveae (CEU) is a rare anomaly characterised by ectropion uveae, iris hypoplasia, iridotrabecular dysgenesis and glaucoma. Hyperplasia of the iris pigment epithelium and its apparent spread over the anterior surface of the iris is supposed to cause the classic ectropion uveae in CEU. Almost all patients develop open angle glaucoma due to angle dysgenesis, so they should be carefully examined periodically for its early detection. We hereby report a case of isolated unilateral CEU without any systemic association which is quite uncommon. Loss of vision went unnoticed while the facial asymmetry secondary to progressive enlargement of one eye became the presenting complain due to this rare unilateral affliction.
Congenital glaucoma, Iridotrabecular dysgenesis, Neovascularization
Case Report
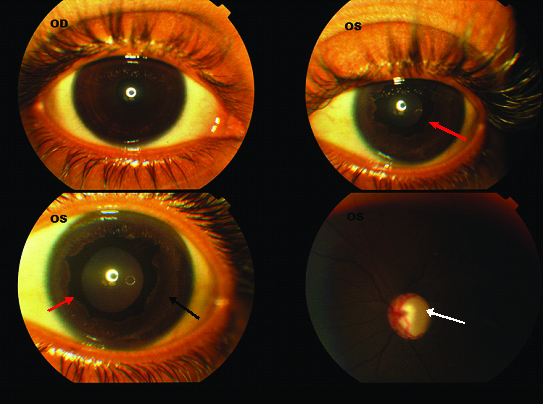
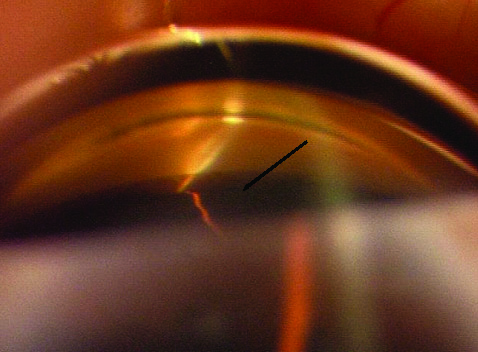
A 12-year-old girl was referred to our tertiary eye care institute for evaluation and management of congenital glaucoma. Her chief complains were progressive loss of vision, drooping of eye lid, enlargement and outward protrusion with occasional photophobia of left eye for the last 5 to 8 years. She was using topical beta blockers prescribed elsewhere on very irregular basis. Visual acuity was 6/6 and Hand Movement (HM) with accurate light projection in right eye (OD) and left eye (OS) respectively. On examination, her left eye was apparently proptosed and Hertel exophthalmometry readings were 17 mm in the left eye and 13 mm in the right with bar reading of 105. She had a ptosis of 2 mm [Table/Fig-1] with good levator function. Slit lamp examination revealed deep anterior chamber and anisocoria of 1.5 mm, the left pupil being larger but round, regular and reacting to light and 360º ectropion uveae with patches of iris atrophy. On fundoscopy, there was near total cupping of the optic disc with a significant pallor of the neuroretinal rim and bayonetting of the vessels in left eye. Anterior segment and fundus were absolutely normal in the right eye [Table/Fig-2]. An abnormal angle with anterior insertion of the iris was noted during gonioscopy examination of left eye [Table/Fig-3]. On applanation tonometry, IOP was 14 mmHg and 48 mmHg in OD and OS respectively. Corneal diameters (Horizontal/Vertical) in OD were 12.0 mm/11mm and OS was 13.5 mm/12.5 mm. Axial length of OD and OS were 22.96 mm and 25.61 mm respectively. No systemic association was noticed.
Mild ptosis in left eye (white arrow) {Photograph shared with permission of the patient};

OD-Normal OS-360º ectropion uveae (red arrow), patches of iris atrophy (black arrow), near total cupping of the optic disc (white arrow). (Images from left to right)
Gonioscopy dipecting anterior insertion of iris (black arrow);
Patient was prescribed oral carbonic anhydrase inhibitor 250 mg three times daily for three days and topical carbonic anhydrase inhibitors three times daily along with a combination of alpha agonist and beta blocker eye drops twice daily to continue. After one week visual acuity, OD was 6/6 and OS improved to 1/60 with IOP of 16 and 32 mmHg respectively. Surgical trabeculectomy with adjunctive mitomycin C was advised under guarded visual prognosis but was refused. She was discharged on medical management. After one month, IOP in LE was 40 mm of Hg on topical medications. Trabeculectomy with mitomycin C (0.2 mg/ml) was performed with proper consent of the patient under guarded visual prognosis.
Three months later on follow up, visual acuity was 6/6 and 2/60 in OD and OS respectively. Refraction was attempted but there was no change probably due to late presentation with advanced glaucomatous optic nerve head damage but the patient was satisfied about her complains of occasional photophobia and progressive enlarging left eye [Table/Fig-4]. IOP was respectively 12 mm and 18 mm Hg in right and left eyes, with low lying and diffuse bleb in the left eye. Corneal diameter and axial lengths remained unchanged. Patient was advised regular follow up.
After three months on follow up.

Discussion
CEU was first described by Wicherkiewicz B in 1891 [1]. It is a rare, non progressive condition with typically unilateral presentation although bilateral cases have also been reported [2]. In contrast to the acquired Ectropion Uveae which is often associated with neovascularization of the iris resulting into tractional force, hyperplasia of the iris pigment epithelium and its apparent spread over the anterior surface of the iris is supposed to cause the classic ectropion uveae in CEU. Failure of regression of the primordial endothelium in the anterior chamber caused by developmental arrest of neural crest tissue in utero is the prime factor inciting this hyperplasia [3]. Although, case reported here is a late presentation of an isolated unilateral CEU, association with systemic diseases like neurofibromatosis and disorders of neural crest origin like Prader-Willi syndrome, Rieger anomaly, and facial hemihypertrophy have been documented [3]. Neural ectodermal origin of muller’s muscle explains the presence of mild ptosis with good levator function in our patient [3].
Glaucoma is a common complication of CEU [4]. Ritch R et al., reported seven out of eight CEU patients developed glaucoma while Dowling JL Jr et al., reported a case series of 10 patients all of which required surgical intervention for IOP control [2,4]. Anterior insertion of the iris causes drainage angle dysgenesis and incomplete formation of trabecular meshwork and schlemm’s canal [5]. Harasymowycz PJ et al., reported presence of a distinct fibrovascular surface membrane covering the anterior aspect of the iris stroma in an infant with CEU on histopathological examination of iris tissue and hypothesized that this membrane might had been responsible for pulling the posterior pigmented layer of the iris anteriorly, creating the ectropion [5].
Visual outcome depends on prompt diagnosis and treatment. Although, medical management may be attempted initially patients with CEU usually requires surgery and the choice of surgery differs from primary congenital glaucoma presumably due to severe angle dysgenesis. Success rate with early goniotomy appears to be much lower in these patients than in primary congenital glaucoma that is greater than 80 percent [6,7]. Glaucoma filtration surgery with or without antimetabolites is necessary [7,8]. Our patient being a girl child was concerned more cosmetically i.e., progressive enlarged eye, ptosis and occasional photopbobia. After intervention patient was benefitted symptomatically and cosmetically with minimal improvement in visual acuity.
Conclusion
Congenital ectropion uvea is mostly associated with refractory glaucoma. Being mostly unilateral and without systemic association contributes to its late detection. Careful periodic examination and early surgical intervention is required to preserve the productive vision.
[1]. Wicherkiewicz B, Contribution to the knowledge of the Ectropion Uveae congenitumGraefe’s Arhiv for Ophthalmology 1891 37:204-07.(Translated from German to English) [Google Scholar]
[2]. Ritch R, Forbes M, Hetherington J, JrHarrison R, Podos SM, Congenital ectropion uveae with glaucomaOphthalmology 1984 91:326-31. [Google Scholar]
[3]. Wilson ME, Congenital iris ectropion and a new classification for anterior segment dysgenesisJ Pediatr Ophthalmology and Strabismus 1990 27(1):48-55. [Google Scholar]
[4]. Dowling JL, JrAlbert DM, Nelson LB, Walton DS, Primary glaucoma associated with iridotrabecular dysgenesis and ectropion uveaeOphthalmology 1985 92:912-21. [Google Scholar]
[5]. Harasymowycz PJ, Papamatheakis DG, Eagle RC, Wilson RP, Congenital Ectropion Uveae and GlaucomaArch Ophthalmol 2006 124(2):271-73. [Google Scholar]
[6]. Mandal AK, Late onset unilateral primary developmental glaucoma associated with iridotrabecular dysgenesis, congenital ectropion uveae and thickened corneal nerves: A new neural crest syndrome?Ophthalmic Surg Lasers 1999 30:567-70. [Google Scholar]
[7]. Wolter JR, Butler RG, Pigment spots of the iris and ectropion uveae with glaucoma in neurofibromatosisAm J Ophthalmol 1963 56:964-73. [Google Scholar]
[8]. Roth H, Shaffer RN, Bellows JG, Neurofibromatosis and glaucomaContemporary Ophthalmology: Honoring Sir Stewart Duke-Elder 1972 Baltimore, MdWilliams and Wilkins:180-189. [Google Scholar]