Pigmented Villonodular Synovitis of Thumb-A Cytological Diagnosis
Kaneeka Bhatnagar1, Akshdeep Singh Bawa2, Vikram Narang3, Pavneet Kaur4
1 Senior Resident, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
2 Senior Resident, Department of Orthopedics, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
3 Assistant Professor, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
4 Professor, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kaneeka Bhatnagar, Senior Resident, Department of Pathology, Dayanand Medical College and Hospital, Tagore Nagar, Ludhiana, Punjab, India.
E-mail: dr.kaneeka@gmail.com
Pigmented Villonodular Synovitis (PVNS) is a unique benign proliferative process of unknown aetiology involving the synovial lined joints diffusely or focally. The entity remains a diagnostic challenge. This condition is attributed to an increased synovial proliferation causing villous or nodular changes of synovial lined joints leading to PVNS, Pigmented Villonodular Bursitis (PVNB) when arising from bursae or Pigmented Villonodular Tenosynovitis (PVNTS) originating from the tendon sheath.
We present a case of a young female with nodular masses on right thumb with cytomorphological features on FNAC suggestive of PVNS which was finally confirmed by histopathology.
Aspiration, Haemosiderin pigment, Nodular masses
Case Report
A 31-year-old lady presented to orthopaedics outpatient department with chief complaint of swelling over the right thumb of hand since one month. The swelling was associated with dull pain and a progressive increase in size [Table/Fig-1]. The complete blood count including ESR were within normal limits and an infective/inflammatory process was ruled out.
Swelling in the proximal phalanx of the right thumb. The change in colour over the skin is evident.

MRI scan of right hand was performed using T1 and T2 weighted sequences in multiple planes [Table/Fig-2]. It revealed a focal lobular soft tissue mass measuring 1.3 x 1.6 x 2.2 cm in anteroposterior, transverse and craniocaudal axis in the right thumb adjoining the anterior cortex of proximal and distal phalanges. These were located under the flexor pollicis longus tendon and causing pressure erosion with excavation of proximal phalanx and proximal portion of distal phalanx. Giant cell tumour of tendon sheath and pigmented villonodular synovitis were kept in differential diagnosis.
MRI of the right hand showing lesion in the proximal and distal phalanx eroding the anterior cortex.
Fine needle aspiration of the lesion was then advised. The patient then came to the pathology department. On examination, a nodular swelling measuring 1.5 x 1 cm was noted on the radial border of the right thumb of hand and it was extending from plantar to palmar surface. The swelling was firm, immobile, tender to touch, with pain radiating to arm and a history of progressive increase in size, however there was no difficulty in gripping or performing daily activities. Fine needle aspiration was performed from the swelling and blood tinged material was aspirated.
Cytology Findings
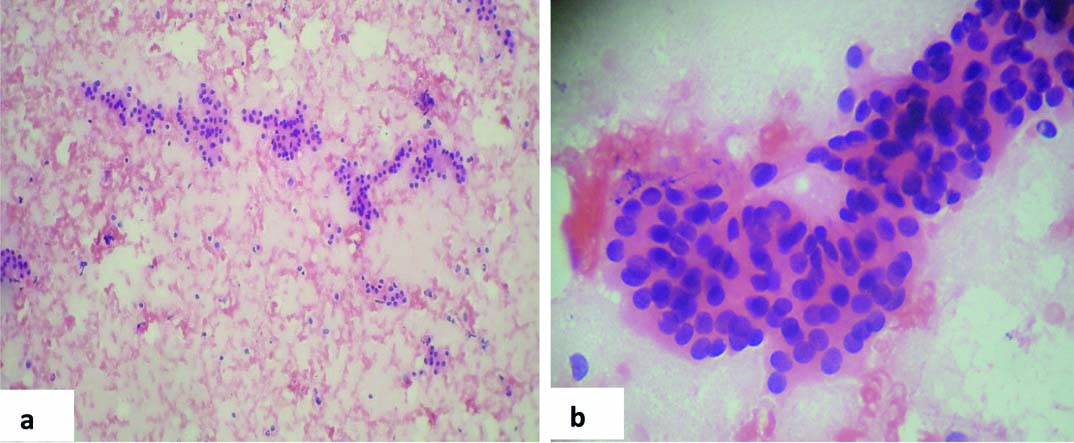
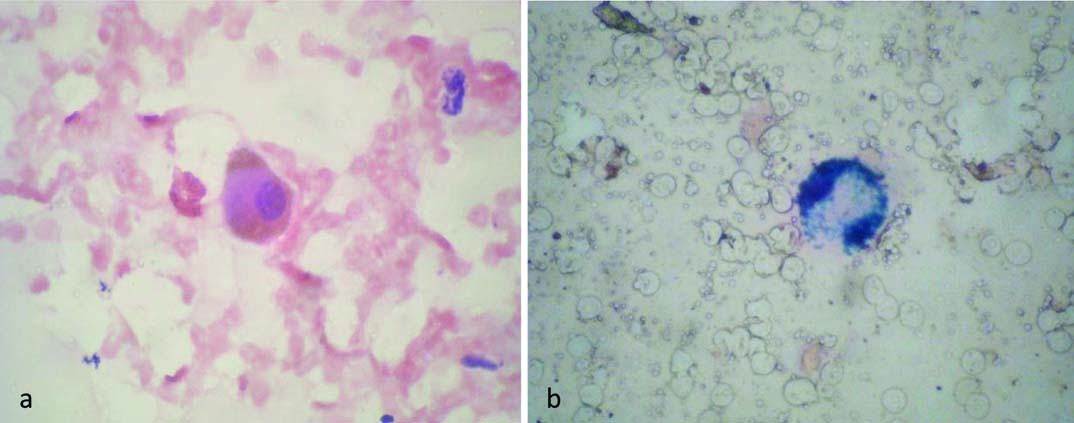
Microscopic examination of aspirates stained with Giemsa and H&E showed cellular smears composed of proliferating synoviocytes seen as tightly cohesive clusters composed of benign cells having round, regular nuclei with bland chromatin, inconspicuous nucleoli and ill-defined granular cytoplasm. Multinucleated giant cells were evident along with singly scattered plump cells having oval pale nuclei with bland chromatin [Table/Fig-3]. Foamy macrophages, few of which were pigment laden were seen in the background. Further, Perl’s stain was done and it was positive for haemosiderin in the macrophages [Table/Fig-4]. A diagnosis of pigmented villonodular synovitis was suggested and biopsy was recommended.
FNAC smears from the lesion show cohesive clusters of cells having bland nuclear features-proliferating synoviocytes. [H&E: a) Low power view, 100X; b) High power view, 400X].
a) Haemosiderin laden macrophage [H&E 400X]; b) Perl’s stain positive for haemosiderin [400X].
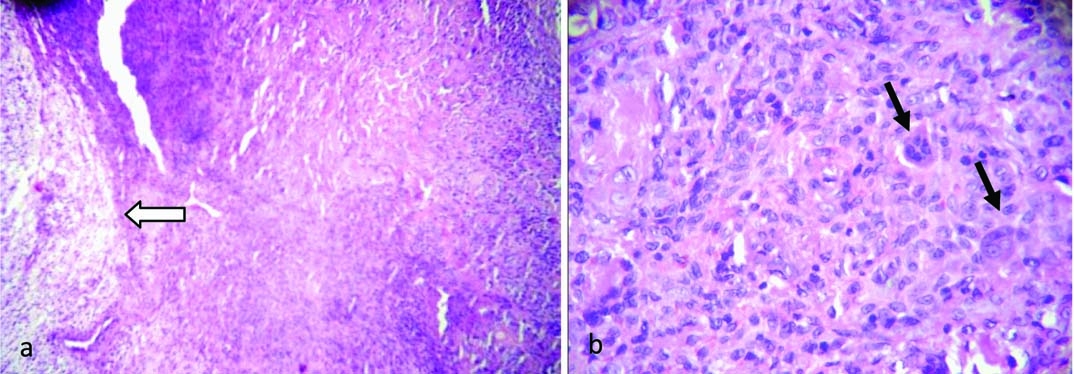
The excision biopsy specimen of the lesion was received as multiple tan coloured soft tissue pieces together measuring 2.5 x 2 x 1.5 cm with areas of calcification. Histopathological examination showed presence of a well circumscribed tumour composed of sheets of cells having oval vesicular nuclei and moderate amount of eosinophilic cytoplasm. Sheets of foamy macrophages with an occasional one having haemosiderin were also identified. Few giant cells with areas of hyalinisation were also noted [Table/Fig-5]. Thus, the histopathological diagnosis of pigmented villonodular synovitis was made, thereby confirming the cytological diagnosis. The follow up was uneventful and there is no recurrence till date.
Photomicrograph showing a cellular mass with: a) Proliferation of synoviocytes along with sheets of foamy macrophages (marked with arrow) [H&E,40X]; b) Multinucleated giant cells (long arrows) and haemosiderin pigment [H&E,400X].
Discussion
Pigmented villonodular synovitis as an entity was first coined by Jaffe in 1941 wherein he used it for fibrohistiocytic tumours of large joints [1]. It is now considered to be a hypertrophic synovial process, benign in nature with villous, nodular, and villonodular proliferation of synovium and haemosiderin pigment [2]. The features vary from lesion to lesion [3]. Pigmented villonodular synovitis is a rare entity, with annual incidence being 1.8 patients per million. Young adults (average age, 35 years) are commonly affected but can be seen in a wide age range with a slight female predominance. Large joints, especially the knee, are commonly affected which accounts for upto 75% to 80% of cases followed by hip, shoulder and ankle although any joint can be involved [4]. Due to the rarity of PVNS as well as the unusual site of presentation i.e., thumb and correct diagnosis being made on cytology the case is being presented.
The pathogenesis of this disease however remains controversial. Clinically, it may resemble common pathologies like tenosynovitis, osteochondral defects, os trigonum injury and tendon tears and therefore leads to a delay in diagnosis [3]. The radiographic images may be normal or show joint effusions, soft tissue masses, which may appear dense if content of haemosiderin deposition is high [5]. Bone mineralization and joint spaces are preserved until quite late in progression and this is characteristic. MRI is the diagnostic modality of choice for PVNS [5]. The Magnetic Resonance (MR) images of PVNS, PVNB, or PVNTS show variable signal intensity and depend on the proportion of lipids, haemosiderin, fibrous stroma, pannus, fluids, and cellular elements. It shows profound hypointense images on both T1- and T2-weighted sequences due to paramagnetic effect of haemosiderin [6].
According to type of presentation, it can be classified into localised, nodular or diffuse type. Extra articular presentation can be seen in diffuse PVNS wherein it is seen in combination with diffuse synovial membrane involvement [3]. Localized PVNS is rather a rare pathology identified by the presence of nodular pedunculated masses protruding into the joint cavity [7]. Diffuse intra-articular PVNS however, is seen as an infiltrating mass extensively involving and causing thickening of synovium of entire joint [8]. According to World Health Organization (WHO) classification, localized PVNS is categorised under the group of giant cell tumour of the tendon sheath, which comprises a group of lesions arising from the synovium of joints, bursae, and tendon sheath. However, diffuse PVNS with diffuse intra-articular involvement is defined under the group of diffuse-type giant cell tumour [9]. FNAC smears are cellular containing sheets of synoviocytes with bland cytological features along with presence of foamy macrophages with pigment in some. Multinucleate giant cells can be seen. Mitosis is rarely seen [10]. Histologically, it is seen as hypertrophy of synovium with irregular papillary/villous projections and nodular or villonodular protrusions. Histiocytic collections along with prominence of foamy macrophages with few containing haemosiderin pigment forming nodules were noted. Scattered multinucleated giant cells are also seen along with areas of hyalinisation and haemorrhage. Mitoses are rarely seen. Ultrastructure and immunohistochemistry studies show these cells sharing the features of synovial cells alternating with fibroblasts and histiocytes [3]. The pathogenetic classification is rather controversial with invasive growth and tendency to recur suggesting a neoplastic origin while considering it as a reactive granuloma would be more logical based on histological findings showing features of granulation tissue [11]. Local destruction leading to significant permanent damage of the joint is seen in PVNS, though it being a benign condition [7]. It tends to recur and can be locally aggressive, if incompletely excised. Surgical resection, with complete synovectomy is the treatment of choice in all cases of PVNS. Adjuvant radiation therapy is given in cases of recurrence [6].
PVNS can be mistaken for common benign tumours such as giant cell lesion of tendon sheath, fibromatosis, cavernous haemangioma and non neoplastic soft tissue lesions as Morton neuroma, ganglion cyst and plantar fasciitis, thus knowledge of this entity is important [3]. Malignant transformation is rarely seen in pigmented villonodular synovitis and occurs de novo or in association with a recurrent disease. These are usually high grade aggressive sarcomas, synovial in origin and associated with a poor outcome [8].
Conclusion
The distinct radiologic appearances along with their pathologic findings help in improving patient assessment and are useful in tailoring proper clinical management. Fine needle aspiration cytology helps in an early accurate detection of PVNS since the cytologic features combined with clinical details are distinctive.
[1]. Nielsen AL, Kiaer T, Malignant giant cell tumor of synovium and locally destructive pigmented villonodular synovitis: ultrastructural and immunohistochemical study and review of literatureHum Pathol 1989 20:765-71. [Google Scholar]
[2]. Bassetti E, Candreva R, Santucci E, Pigmented villonodular synovitis of the knee: A case reportJournal of Ultrasound 2011 14:167-69. [Google Scholar]
[3]. Kinra P, Varghese B, Pigmented villonodular synovitis: dorsum footMedical Journal, Armed Forces India 2007 63:294-96. [Google Scholar]
[4]. Lucas DR, Tenosynovial giant cell tumour: case report and reviewArchives of Pathology & Laboratory Medicine 2012 136:901-06. [Google Scholar]
[5]. Gulia A, Dhanda S, Puri A, Ramadwar M, Pigmented villonodular synovitis of proximal tibiofibular joint: Rare site of involvement treated with medical managementSouth Asian J Cancer 2016 5:211-12. [Google Scholar]
[6]. Kim I-K, Cho H-Y, Cho H-W, Seo J-H, Lee D-H, Peng W, Pigmented villonodular synovitis of the temporomandibular joint - computed tomography and magnetic resonance findings: a case reportJ Korean Assoc Oral Maxillofac Surg 2014 40:140-46. [Google Scholar]
[7]. Kwon JH, Han JH, Almeida VR, Kim SH, Park HJ, Nha K-W, Localized pigmented villonodular synovitis of the proximal tibiofibular jointKnee Surgery & Related Research 2014 26:249-52. [Google Scholar]
[8]. Murphey DM, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA, Pigmented villonodular synovitis: radiologic-pathologic correlationRadioGraphics 2008 28(5):1493-518. [Google Scholar]
[9]. Hong CM, Hing LT, Acute knee pain in a child due to pigmented villonodular synovitisJournal of Orthopaedic Case Reports 2015 5:78-80. [Google Scholar]
[10]. Shapiro SL, McMenomey SO, Alexander P, Schmidt WA, Fine-needle aspiration biopsy diagnosis of “invasive” temporomandibular joint pigmented villonodular synovitisArchives of Pathology & Laboratory Medicine 2002 126:195-98. [Google Scholar]
[11]. Perka C, Labs K, Zippel H, Buttgereit F, Localized pigmented villonodular synovitis of the knee joint: neoplasm or reactive granuloma? A review of 18 casesRheumatology 2000 39:172-78. [Google Scholar]