Ovarian epithelial type tumour of testis are extremely rare tumours that resemble ovarian surface epithelial tumours. They usually present as testicular or paratesticular tumours and can be serous, mucinous, endometrioid or Brenner tumour. Serous and mucinous types account for the majority of tumours. The tumours are benign, borderline or malignant, commonly borderline.
Here, we report a case of high grade serous cyst adenocarcinoma of testis which manifested as extensive metastasis in supraclavicular, mediastinal and abdominopelvic groups of lymph nodes, lung and adrenal gland without clinical evidence of an overt primary tumour. We report this case so as to make clinicians and pathologists aware of this rare entity and to stress on the fact that this rare entity should be kept in mind when evaluating cases of metastatic adenocarcinoma in male patients.
Case Report
A 67-year-old male patient presented to our surgical oncology outpatient department, with lower abdominal pain and right scrotal swelling, gradually increasing in size for two months duration. He gave a history of reduced appetite and weight loss with regular bowel and bladder habits. He was on steroid inhalers and long acting β agonist for more than five years as treatment for Chronic Obstructive Airway Disease (COPD).
On examination, there was a non-tender scrotal swelling appearing clinically as hydrocele. A hard mobile supraclavicular lymph node measuring 2 x 1 cm was also noted. A clinical diagnosis of metastasis of unknown origin was made and further work up was advised.
Biochemical study showed LDH- 521, AFP-2.25 ng/ml, BETA HCG – 1.06, PSA- 3.64, CA 19.9- 548.3 u/ml. Liver function test and renal function test were within normal limits.
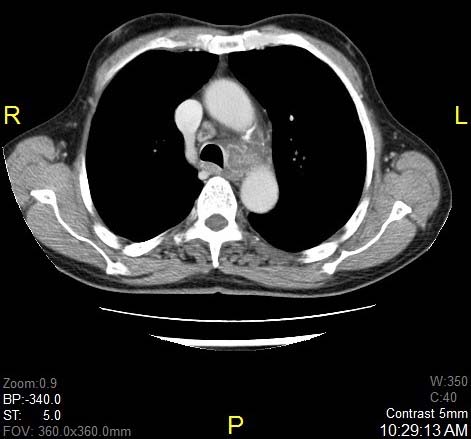
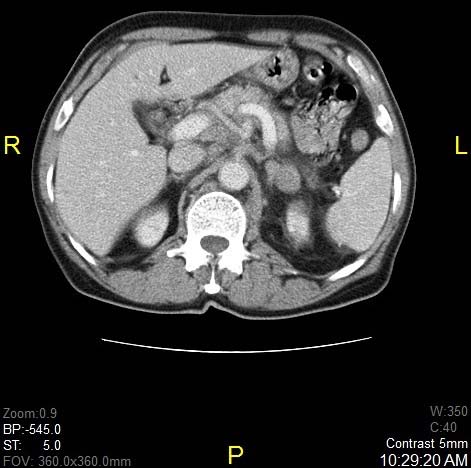
CT scan of thorax and abdomen revealed bilateral pretracheal, paratracheal, aortopulmonary, precarinal and subcarinal lymph nodes, largest measuring 4.6 x 2.9 cm [Table/Fig-1]. Lung nodules suspicious of metastasis was seen. Nodules in left adrenal gland and, necrotic abdominal nodes were also seen [Table/Fig-2]. FDG –F 18 PET/CT scan was performed and it confirmed metabolically active lesion in above sites. Differential diagnosis of lymphoma was also considered.
Axial post contrast CT of thorax showing metastatic aortopulmonary window lymph nodes.
Axial post contrast CT of upper abdomen showing metastasis in left adrenal gland, multiple paraaortic, and retrocaval and peripancreatic lymph nodes.
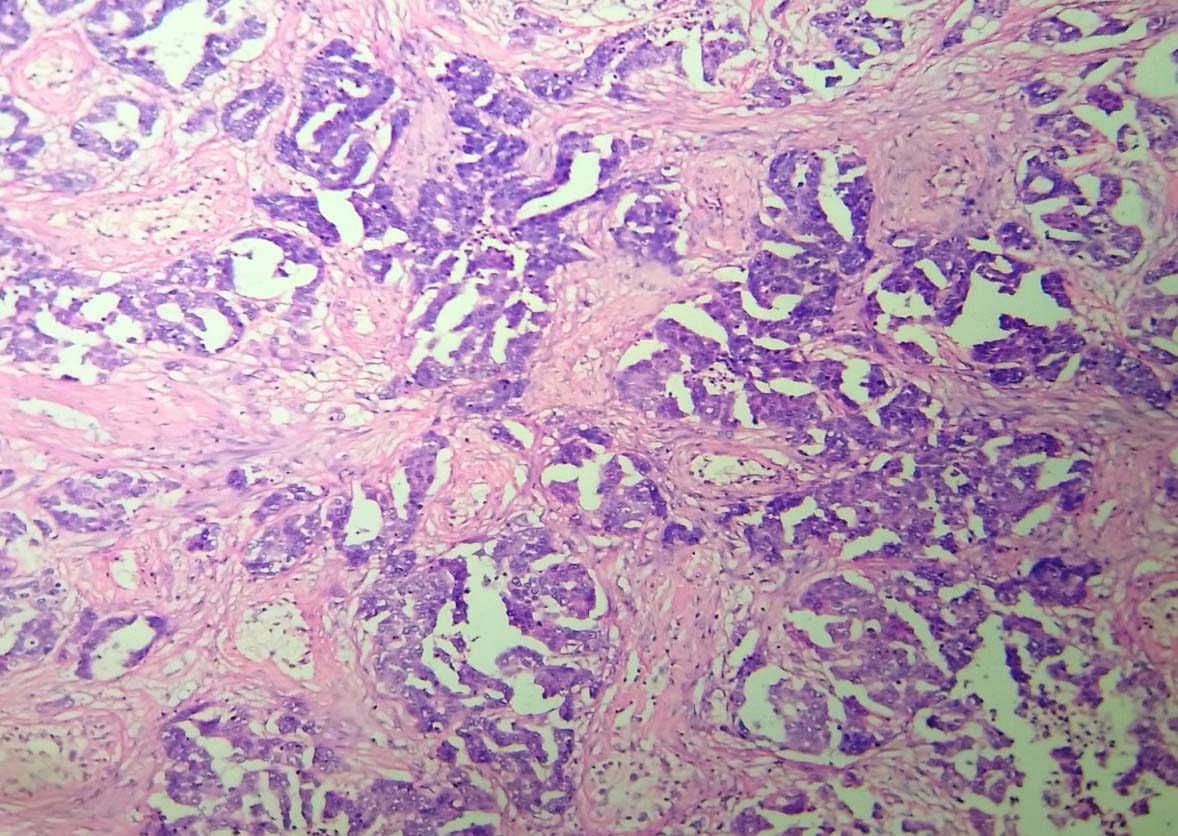
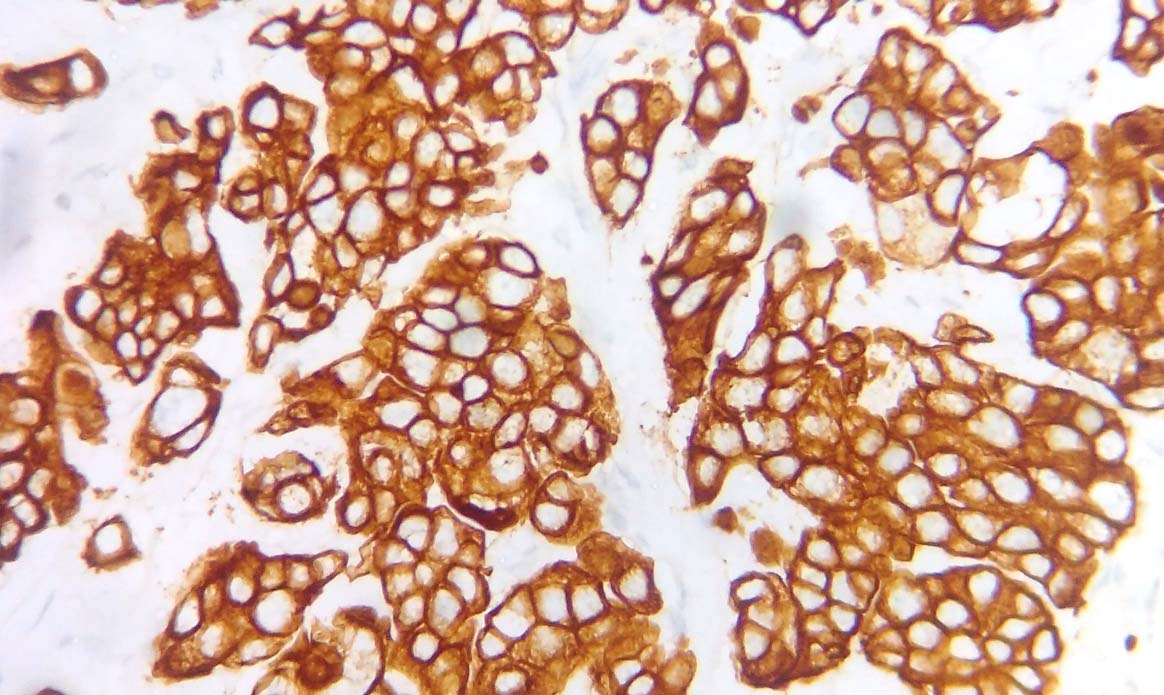
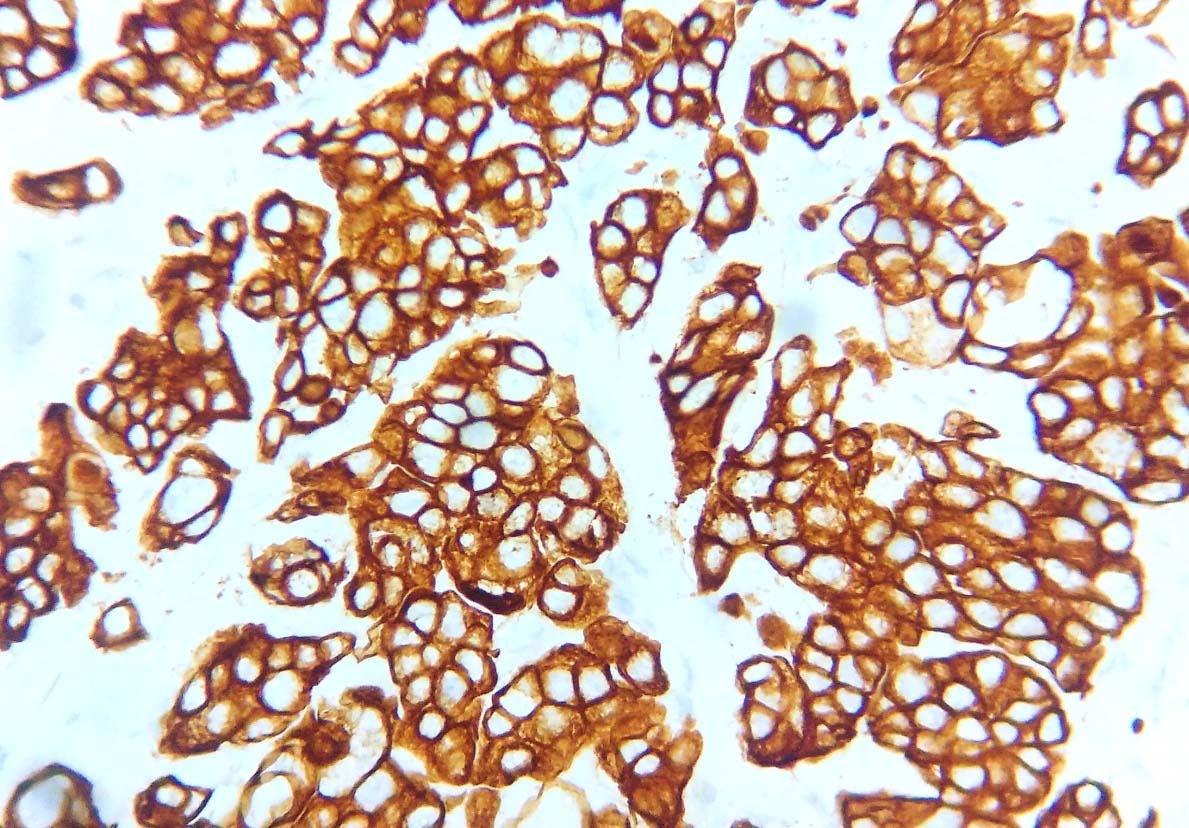
Supraclavicular node trucut biopsy was performed and histo-pathology showed an invasive neoplasm with cells arranged in micropapillary and tubular pattern with cells showing moderate nuclear pleomorphism and abundant mitotic figures suggestive of a metastatic papillary carcinoma [Table/Fig-3] with possible primary sites being lung, prostate, bladder, germ cell tumours of testis and gastrointestinal system. In order to locate the most probable primary, a battery of IHC- CK7 [Table/Fig-4], CK20, TTF1, PSA, HEPAR-1, CDX2, calretinin, CD 30, chromogranin was performed. Except for CK7, all antibodies were found to be negative. IHC and serum markers of germ cell tumours were also found to be negative.
Invasive neoplasm with cells arranged in micropapillary and tubular pattern. (H&E 10X).
IHC shows strong cytoplasmic positivity for CK 7 (IHC 40X).
Meanwhile CT pelvis was done from outside which revealed a 1 x 1 cm testicular swelling.
Right side Chevassue’s procedure was done and the tumour was identified in the right testis and the specimen was sent for frozen section. On gross examination testis measured 5 x 3.5 cm. Cut section showed a grey white firm, ill circumscribed nodule measuring 1 x 1 x 0.5 cm. The frozen section was reported as a high grade carcinoma.
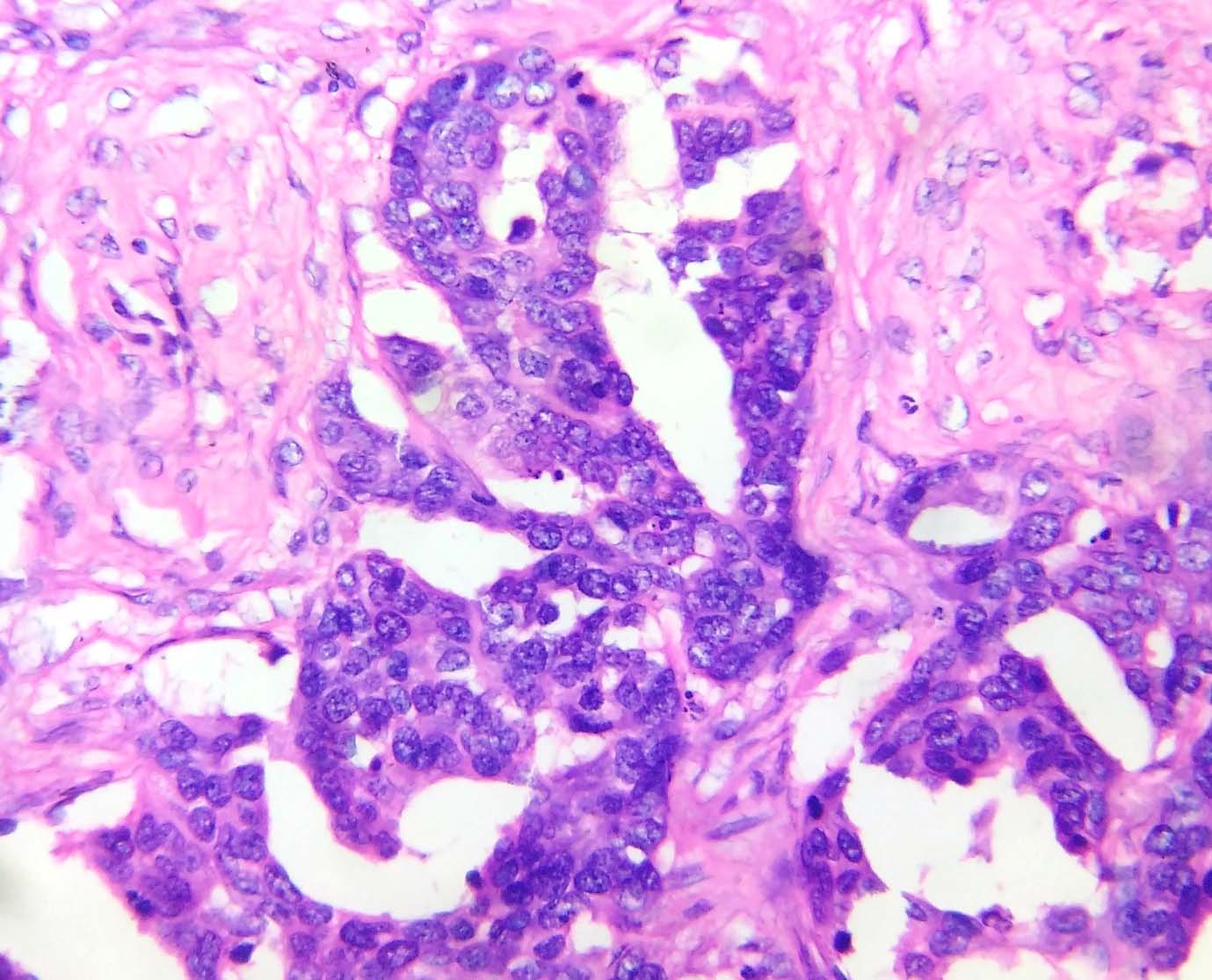
Microscopic examination of permanent sections showed an invasive neoplasm with cells arranged in micropapillary, tubular, nests and cribriform pattern. The cells had moderate cytoplasm and moderate nuclear pleomorphism. Mitotic figures were seen in plenty [Table/Fig-5,6]. Histomorphological picture resembled a high grade ovarian serous carcinoma. IHC markers of CA-125 [Table/Fig-7] and Ki 67 [Table/Fig-8] were performed. Serum Ca-125 was evaluated simultaneously.
Tumour cells with moderate cytoplasm and moderate nuclear pleomorphism. (H&E 40X).
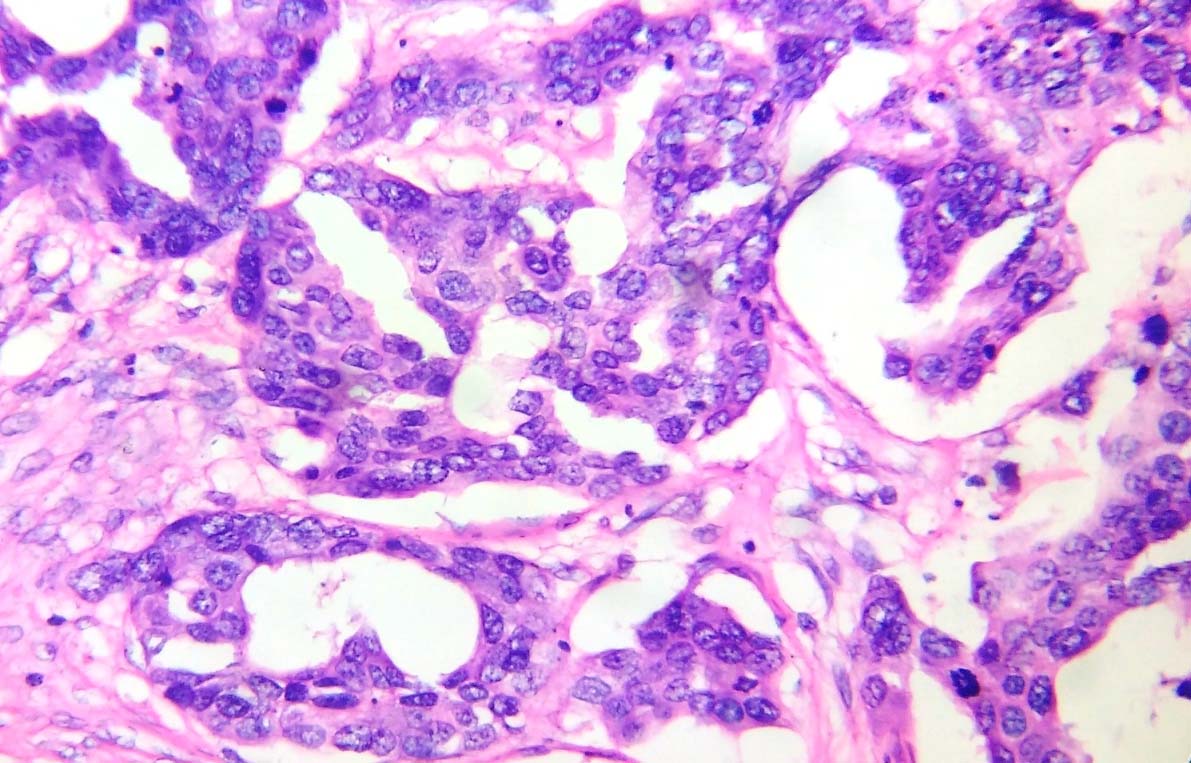
Abundant mitotic figures seen (H&E 40X).
IHC shows strong diffuse positivity for CA125 (IHC 10X).
IHC shows nuclear positivity for KI 67 (IHC 10X).
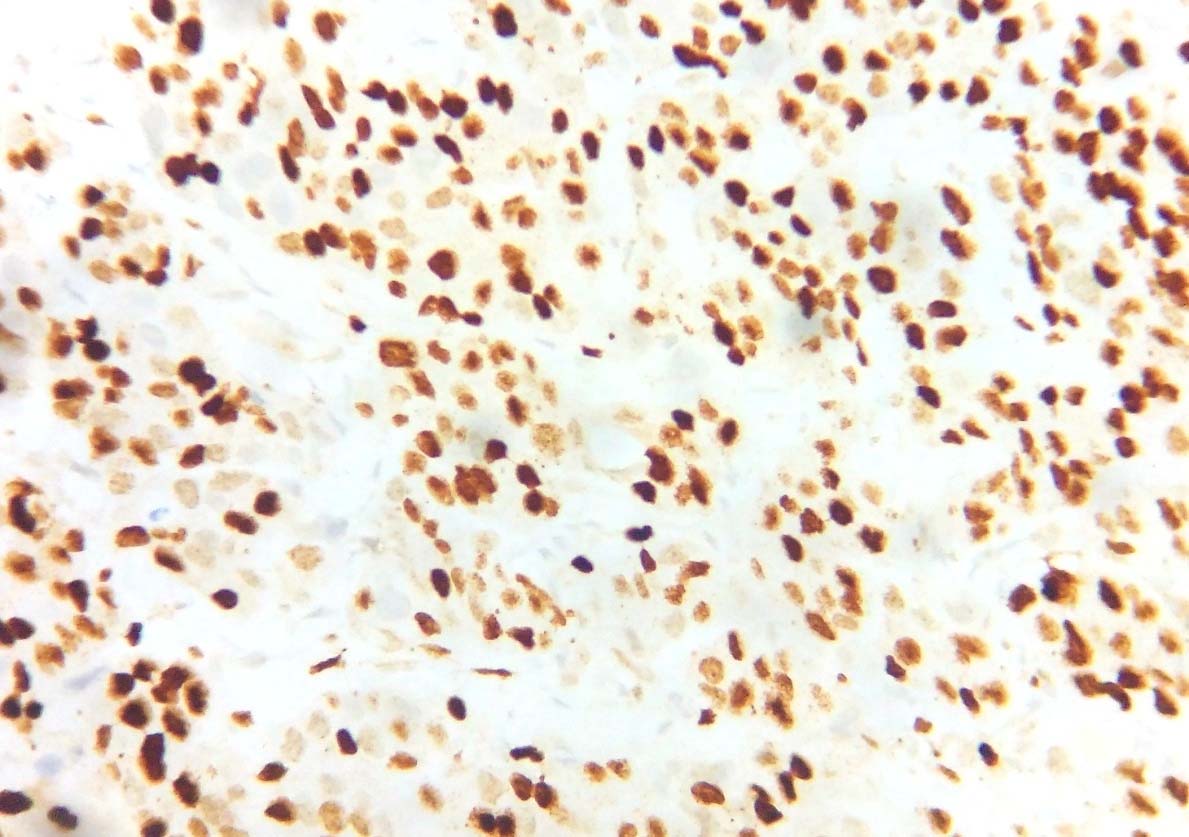
Tumour cells showed a strong diffuse positivity for CA 125 with a high proliferative index- Ki 67- 80%-85%. Serum CA-125 was markedly elevated- 5420 µ/ml. Thus, a final diagnosis of a high grade serous cystadenocarcinoma testis was made.
The patient was offered three cycles of palliative chemotherapy with paclitaxel and carboplatin. Following three cycles, CT scan was done for response assessment. The scan showed partial response to treatment and so three more cycles of chemotherapy were offered. On completion of chemotherapy, patient was kept on monthly follow up. The last visit was two weeks back. His general condition deteriorated with an ECOG personal score 3-4 and was advised best supportive care. He succumbed to disease last week.
Discussion
Though literature search reveals plenty of information regarding testicular germ cell tumours and metastatic carcinomas, there is little information about tumours of ovarian epithelial type of the testis and paratesticular tissue. Described in the WHO Male Genital Organs’ classification 2004 and 2016, under the heading miscellaneous tumours of testis as ovarian type epithelial tumours, this entity is encountered in a wide age range of 14-68 years. The lesions are usually paratesticular, though testicular tumours are rarely described. Patient usually presents with scrotal enlargement [1].
A high degree of suspicion and awareness about this entity is essential for diagnosis. These tumours can histologically be serous, mucinous, endometrioid or Brenner tumour; most common being serous type. The tumours are benign, borderline or malignant, commonly borderline [2-4].
Cell of origin of ovarian type epithelial tumours of the testis is still a matter of dispute. Several postulates have been put forward. They are supposed to originate either from the remnants of Müllerian ducts in paratesticular connective tissue, epididymis, and spermatic cord or from the mesothelium of the tunica vaginalis of testis that has undergone Müllerian metaplasia [5]. Another line of thought suggests their origin from Müllerian metaplasia of intratesticular mesothelial inclusions, possibly triggered by injury during embryogenesis [6].
This entity usually occurs in patients within a wide age range of 14-68 years. The lesions are usually paratesticular though testicular tumours are described [1]. The usual presenting complaint is testicular enlargement [7].
Clinico-radiological features do not distinguish this tumour from other similar tumours in this region [8]. Usual radiological appearance of the tumour is as a 2.0-3.5 cm paratesticular mass, associated with a hydrocele [9].
Normal serum levels of AFP, BHCG, CEA like germ cell tumour markers together with a very high value of serum CA125, should raise the suspicion of this tumour [10].
In our experience, serum marker CA125, is helpful both as a diagnostic and prognostic marker just as in ovarian serous carcinomas.
An important differential diagnosis of this serous carcinoma with papillary features is metastatic deposits from sites like lung, prostate, bladder and GIT. IHC panel including CK7, CK20, TTF1, PSA, HEPAR-1, CDX2 etc., with radiological support helps in ruling out a metastatic carcinoma. A second differential diagnosis is mesothelioma [11] which was ruled out using the IHC marker Calretinin.
Chromosomal aberrations, of which the most common are gains of chromosomes 2q, 6q, 5, 8q and 12 and losses of 1p, 17p, 19 and 22q are encountered especially in sets of borderline serous tumours [12,13]. Though BRAFV600E mutation is common in ovarian borderline and low grade serous carcinomas, till date, only one very recent study has shown a mutation of BRAF V600E in a serous borderline tumour of the testis [14].
As serous carcinomas of the testis and para-testis are extremely rare tumours, there has been minimal clinical experience with management of these types of tumours worldwide. No consensus has been reached yet regarding specific guidelines for treatment. Literature review shows that same treatment protocol for ovarian serous carcinomas in women is a reasonable approach [15]. Long term follow up of the patient with close monitoring is advisable, as this high grade tumour has a rapid rate of progression and can commonly have late metastases [15].
Conclusion
We report this case so as to make clinicians and pathologists aware of this rare entity in the male genital system and to stress on the fact that ovarian epithelial type tumour of the testis and paratesticular area should be kept in mind when evaluating a case of metastatic adenocarcinoma with unknown primary.
[1]. Moch H, Humphrey PA, Ulbright TM, Reuter V, WHO Classification of Tumours of the Urinary System and Male Genital Organs 2016 Lyon, FranceInternational Agency for Research on Cancer [Google Scholar]
[2]. Axiotis CA, Intratesticular serous papillary cystadenoma of low malignant potential: an ultrastructural and immunohistochemical study suggesting mullerian differentiationAm J Surg Pathol 1988 12(1):56-63. [Google Scholar]
[3]. Abdullah LS, Gupta R, Arnst A, Intratesticular borderline serous tumourInt J Urol 2006 13(12):1536-38. [Google Scholar]
[4]. Remmele W, Kaiserling E, Zerban U, Hildebrand U, Bennek M, Jacobi-Nolde P, Serous papillary cystic tumour of borderline malignancy with focal carcinoma arising in testis: case report with immunohistochemical and ultrastructural observationsHum Pathol 1992 23(1):75-79. [Google Scholar]
[5]. Michal M, Kazakov DV, Kacerovska D, Kuroda N, Lovric E, Wachter DL, Paratesticularcystadenomas with ovarian stroma, metaplastic serous Mullerian epithelium, and male adnexal tumour of probable wolffian origin: A series of 5 hitherto poorly recognized testicular tumoursAnn Diagn Pathol 2013 17(2):151-58. [Google Scholar]
[6]. Jones S, Wang TL, Kurman RJ, Nakayama K, Velculescu VE, Vogelstein B, Low-grade serous carcinomas of the ovary contain very few point mutationsJ Pathol 2012 226(3):413-20. [Google Scholar]
[7]. Wilmosh M, Neta V, Irina G, Josef K, Serous papillary adenocarcinoma of the rete testis: Unusual ultrasonography and pathological findingsJournal of Cancer Research and Therapeutics 2007 3(1):37-39. [Google Scholar]
[8]. Al-Hussain T, Gordetsky J, Jimenez R, Rane SU, Williamson S, Revised: 20 April 2017(c) 2003-2017, Testis and epididymisPathologyOutlines.com, Inc [Google Scholar]
[9]. Rane SU, Testis and epididymisParatesticular tumours Serous papillary carcinoma. Revised: 1 September 2014, Copyright: (c) 2003-2014PathologyOutlines.com, Inc [Google Scholar]
[10]. Ma YT, Chaudhri S, Cullen MH, Metastatic serous carcinoma of the testis: a case report and review of the literatureCase Rep Oncol 2011 4(1):246-49. [Google Scholar]
[11]. Amin MB, Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumours, mesothelial lesions and secondary tumoursMod Pathol 2005 18(Suppl 2):S131-S145. [Google Scholar]
[12]. Micci F, Haugom L, Ahlquist T, Andersen HK, Abeler VM, Davidson B, Genomic aberrations in borderline ovarian tumoursJ Transl Med 2010 8:21 [Google Scholar]
[13]. Wolf NG, Abdul-Karim FW, Farver C, Schrock E, du Manoir S, Schwartz S, Analysis of ovarian borderline tumours using comparative genomic hybridization and fluorescence in situ hybridizationGenes Chromosomes Cancer 1999 25(4):307-15. [Google Scholar]
[14]. Cundell D, Pawade J, Sohail M, Melegh Z, V600e BRAF mutation in a borderline serous tumour of the testis is genotypic evidence of similarity with phenotypic ovarian counterpartHistopathology 2015 67(1):142-44. [Google Scholar]
[15]. Yeh CH, Hsieh PP, Lin SJ, Hong YC, Tsai TH, Hsueh-Lin Yu L, Testicular serous carcinoma of ovarian epithelial type: A case report and review of the literatureJournal of Cancer Research and Practice 2016 4(2):76-79. [Google Scholar]