Atraumatic Acute Compartment Syndrome of Forearm Following Artificial Mehndi (Henna) Dermatitis – A Rare Case Report
Abhinav Sinha1, Lakshay Goel2, Rahul Ranjan3, Sahil Gaba4, Arvind Kumar5
1 Senior Resident, Department of Orthopaedics, Lady Hardinge Medical College, New Delhi, India.
2 Junior Resident, Department of Orthopaedics, Lady Hardinge Medical College, New Delhi, India.
3 Senior Resident, Department of Orthopaedics, Lady Hardinge Medical College, New Delhi, India.
4 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, Chandigarh, India.
5 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sahil Gaba, House No. 165, Sector 33 A, Chandigarh, India.
E-mail: drsahilgaba@gmail.com
Atraumatic compartment syndrome of the forearm is a rare entity. There are several papers available in the literature on the adverse effects of mehndi application; however Acute Compartment Syndrome (ACS) following mehndi application has never been reported. We present the case of a 25-year-old female, who presented with sudden onset swelling and pain in the left forearm. The patient had applied mehndi all over her left palm and forearm just two days prior to presentation. The patient had stretch pain and other clinical features suggestive of compartment syndrome of forearm and was hence taken up for an emergency fasciotomy. The fasciotomy wound healed without skin grafting and the patient achieved near normal range of movement of the affected elbow, wrist and fingers.
Fasciotomy, Hypersensitivity, Nerve decompression
Case Report
A 25-year-old female presented to Orthopaedic Emergency with sudden onset of swelling and pain in the left forearm of six hours duration. Pain was disproportionate to the swelling and continuously increasing. There was no history of trauma or fever. The patient had artificial henna applied all over her left palm and forearm, as she had been to a wedding just two days prior to presentation. On detailed history, the patient stated that she had a minor superficial cut (incised wound) over her wrist (volar aspect) due to a broken glass (bangle) just two days prior to application of mehndi. There was no significant past medical history and no history of allergic reaction to henna in the past.
The physical examination of the forearm revealed it to be firm and oedematous, and tender on palpation. There was a superficial cut wound on the volar crease of wrist. The local temperature however was not raised. Wound that was present on the volar aspect of wrist appeared in healing phase and there were no signs of inflammation around the wound. The mid forearm circumference was 2 cm larger than the right side. The patient kept her wrist in a flexed attitude and passive dorsiflexion of wrist and fingers was painful. Paraesthesia was present in the median nerve distribution and 2-point discrimination was increased in comparison to right palm. However, the radial pulse was palpable (albeit weak in comparison to opposite side) and capillary refill was nearly three seconds. Distal oxygen saturation was recordable in all fingers and was fluctuating between 97-99%.
Her initial laboratory evaluation showed a total leucocyte count of 0.5 X 109/l and a C-Reactive Protein (CRP) of 11.1mg/l. ESR and coagulation profile were normal. X-Rays of wrist, forearm and arm were normal. Venous and arterial duplex ultrasound studies of the extremity were performed. The arterial duplex demonstrated no evidence of arterial thrombosis, stenosis, or occlusion. The venous study showed normal flow and compressibility with continuous waveforms. Informed written consent was obtained from the patient for reporting this case.
As the clinical picture was consistent with ACS, the patient underwent immediate fasciotomy of the forearm. A single incision volar fasciotomy was done as only the volar compartment appeared involved. Median nerve decompression was also done in the carpal tunnel. Flexor muscles appeared to bulge during the fasciotomy, but fortunately were pink and contractile. Intraoperative wound cultures were taken, which were sterile. Postoperative period was uneventful. Daily aseptic dressings were done and empirical antibiotics were prescribed. There was no sign of infection in the wound during recovery period. Secondary closure was achieved using serial tightening of a silicon vascular loop applied at the margins of the fasciotomy [Table/Fig-1].
Showing fasciotomy incision along with vascular loop that was gradually tighten to close the wound. Decorated tattoo of mehndi can be very well marked in this figure

Gentle passive and active assisted range of motion exercises of elbow, wrist, and fingers were started in the first few days after fasciotomy even before wound closure. Once the wound healed and pain reduced, the intensity of physiotherapy was increased with a focus on muscle strengthening and regaining joint motion (especially of wrist and fingers). Patch test for dermatitis was done, which came out to be positive. Fexofenadine (oral anti-allergic) was started on first postoperative day. At final follow up, elbow, wrist and hand function was good with near normal range of motion [Table/Fig-2a-c], the wound had healed with secondary intention without the use of any graft [Table/Fig-3]. There was no residual nerve dysfunction.
Showing range of movement at wrist and elbow after healing of the fasciotomy wound.

Showing healed fasciotomy scar.

Discussion
ACS is an Orthopaedic Emergency that develops when the pressure within a closed fascial space rises to the point that it compromises the perfusion to that compartment [1]. It is typically associated with high energy trauma, commonly occurring as a result of long bone fractures or severe crush injury. Atraumatic compartment syndrome is uncommon [2]. The common atraumatic aetiologies for ACS include recreational drug use, intravenous infiltration injuries, snake envenomation, infections etc., [2]. There is no case report in the available literature showing application of mehndi (henna) leading to forearm compartment syndrome. [Table/Fig-4] enlists the common and uncommon causes of ACS.
Common and uncommon causes of ACS.
| Common causes | Fractures (closed/open) (overall most common cause)Tibial diaphyseal (most common)Distal radius (2nd most common)Forearm bones diaphysealAnkle fracture, Pilon fracture, etc.,Soft tissue injury (Crush injury) |
| Rare causes | Arterial injurySnake biteRhabdomyolysisBurnsFluid extravasation (after IV cannulation or arthroscopy)Infection (e.g., Acute osteomyelitis)Exercise inducedNephrotic syndromeDrug/Alcohol abuse/ComaPost ischemia (revascularization injury)Rupture Baker cystVasculitis |
Application of mehndi or henna over palm and forearm is a common practice among women, especially on weddings and certain festivals. It is widely used in Indian subcontinent and now its use has also spread to the west. Although, several skin reactions occurring as a consequence of additives of artificial henna have been reported in the literatures [3-9], but there are no published reports of severe reaction leading to compartment syndrome endangering the involved limb. We report the case of a compartment syndrome of forearm resulting from a minor skin puncture wound and subsequent artificial mehndi application.
ACS is primarily a clinical diagnosis. The signs associated with compartment syndrome have traditionally been referred to as the ‘Five ‘P’s’’, namely pain, pallor, paraesthesia, pulselessness and pain with passive stretch of muscles [10]. Pulselessness is regarded as a late finding and does not always accompany compartment syndrome [10]. If a limb is pulseless, it means that the diagnosis has been delayed and the result will be poor even after fasciotomy [11]. Several theories have been proposed regarding the pathophysiology of ACS [12]. The arteriovenous gradient theory is arguably the most popular. It states that, the increasing tissue pressure eventually leads to decreased tissue perfusion. Muscle ischemia resulting from decreased oxygen delivery, eventually progresses to muscle death. Over time the muscle is replaced with dense fibrous tissue, which results in limb contracture [1].
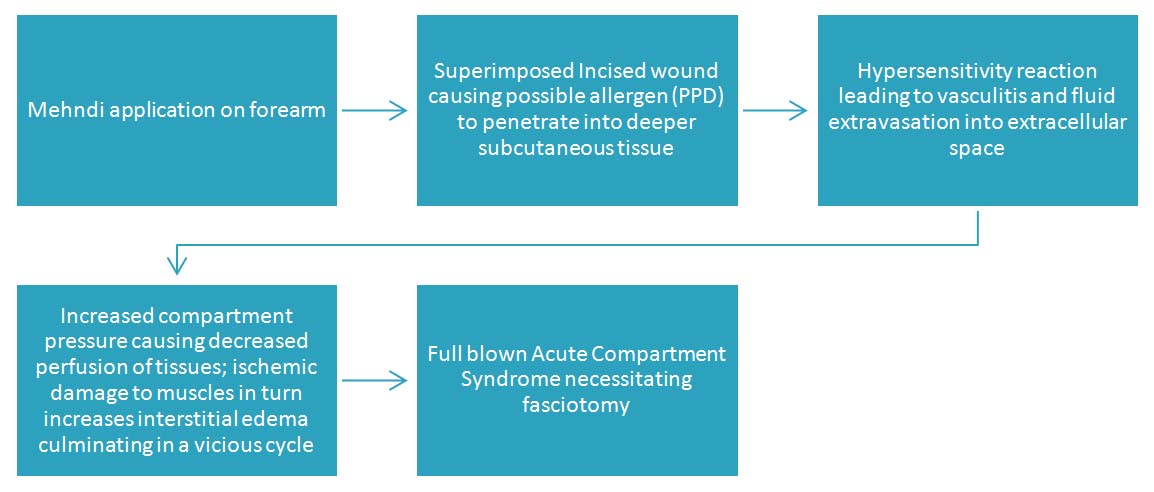
Natural Mehndi or henna dye is prepared by grinding the fresh leaves of a plant, Lawsonia inermis. The resulting brown dye is extensively used as decorative skin paint, for nail colouring and as hair dye and conditioner. The use of this natural cosmetic is a common tradition in India. For instance, wedding ceremonies in many parts of the country would be incomplete without the ritual of creating intricate designs on the hands and feet of the bride with henna. Allergic reaction to pure Henna is rare. Henna is commonly mixed with para-Phenylenediamine (PPD), also known as black henna. PPD condenses the dark colour, speeds up the colouring process and makes the patterns last longer [3,4]. PPD is known to be a potent skin and respiratory tract sensitizer and believed to cause allergic contact dermatitis, a type IV delayed hypersensitivity reaction [5,6]. PPD has also been known to cause severe vesicular erythema multiforme like reaction, bullous contact dermatitis, post inflammatory hypo or hyperpigmentation, lichenoid reaction, keloid formation etc., [7-9]. However, these are relatively innocuous. The probable cause of such a severe reaction in our patient was likely due to the cut wound, which allowed the allergen (PPD) to gain access to deeper tissues, coupled with hypersensitivity to PPD. The probable sequence of events can be summarized as in the flowchart below [Table/Fig-5].
Probable sequence of events.
Henna has also been used as a skin marker prior to surgery or interventional procedures for marking stoma sites, aspiration of liver abscess, varicose vein surgery, marking vertebral level in spinal surgery, etc., [13,14]. No adverse reaction was reported, although the authors did caution against using it in Glucose 6 phosphate dehydrogenase deficient patients, owing to the risk of haemolysis [15-17].
Although the practice of using henna for colouring has been used since ages, it is only since late 90’s that several papers regarding adverse effects of henna use have been coming up. These side effects are mostly due to PPD and certain other additives which are added to the henna to speed up the colouring process. Although several skin reactions occurring as a consequence of these additives in henna are well known in literature, there are no published reports of such severity of reaction leading to compartment syndrome and endangering a limb. Also, in the presence of a dark coloured background, superficial skin changes were difficult to pick in our case and hence we had to rely on the disproportionate pain, tense swelling and stretch pain to make the diagnosis of ACS. The differential diagnosis included infection and dermatitis. Early fasciotomy led to minimal residual contracture and good overall hand function. The use of silicon loop led to early closure of the fasciotomy wound without the need of skin graft.
Conclusion
The use of artificial henna leads to many adverse skin reactions. But none is as severe as ACS, because a delay in fasciotomy can endanger the limb as well as life of the patient. It is better to use natural henna instead of synthetic alternatives, as presence of unknown chemicals can increase the risk of adverse events. A prompt and judicious fasciotomy is the only way of achieving a satisfactory outcome. It is a huge diagnostic dilemma as the initial picture might be similar to cellulitis. High index of suspicion in necessary.
[1]. McQueen MM, Duckworth AD, The diagnosis of acute compartment syndrome: A reviewEur J Trauma Emerg Surg 2014 40(5):521-28. [Google Scholar]
[2]. Hope MJ, McQueen MM, Acute compartment syndrome in the absence of fractureJ Orthop Trauma 2004 18(4):220-24. [Google Scholar]
[3]. Wolf R, Wolf D, Matz H, Orion E, Cutaneous reactions to temporary tattoosDermatology online journal 2003 9(1):3 [Google Scholar]
[4]. Redlick F, DeKoven J, Allergic contact dermatitis to paraphenylendiamine in hair dye after sensitization from black henna tattoos: A report of six casesCanadian Medical Association Journal 2007 176(4):445-46. [Google Scholar]
[5]. Uzuner N, Olmez D, Babayigit A, Vayvada O, Contact dermatitis with henna tattooIndian Pediatr 2009 46(5):423-24. [Google Scholar]
[6]. Kazandjieva J, Grozdev I, Tsankov N, Temporary henna tattoosClinics in dermatology 2007 25(4):383-87. [Google Scholar]
[7]. Sidwell RU, Francis ND, Basarab T, Morar N, Vesicular Erythema Multiforme-like Reaction to Para-Phenylenediamine in a Henna TattooPaediatric dermatology 2008 25(2):201-04. [Google Scholar]
[8]. Jung P, Sesztak-Greinecker G, Wantke F, Götz M, Jarisch R, Hemmer W, A painful experience: Black henna tattoo causing severe, bullous contact dermatitisContact Dermatitis 2006 54(4):219-20. [Google Scholar]
[9]. Gunasti S, Aksungur VL, Severe inflammatory and keloidal, allergic reaction due to para-phenylenediamine in temporary tattoosIndian Journal of Dermatology, Venereology, and Leprology 2010 76(2):165 [Google Scholar]
[10]. Taylor RM, Sullivan MP, Mehta S, Acute compartment syndrome: Obtaining diagnosis, providing treatment, and minimizing medicolegal riskCurr Rev Musculoskelet Med 2012 5(3):206-13. [Google Scholar]
[11]. Raza H, Mahapatra A, Acute compartment syndrome in orthopedics: Causes, diagnosis, and managementAdv Orthop 2015 2015:1-8. [Google Scholar]
[12]. Mabvuure NT, Malahias M, Hindocha S, Khan W, Juma A, Acute compartment syndrome of the limbs: Current concepts and managementThe Open Orthopaedics Journal 2012 6:535-43. [Google Scholar]
[13]. Thora A, Bhatnagar N, Tiwari A, Lingaiah P, Rustagi N, Use of henna as a durable preoperative skin marker for accurate localisation of vertebral level in spine surgeryInternational Journal of Research in Orthopaedics 2017 3:3 [Google Scholar]
[14]. Mehendale VG, Chaudhari NC, Shenoy SN, Mehendale AV, Henna as a durable preoperative skin markerWorld Journal of Surgery 2011 35(2):311-15. [Google Scholar]
[15]. Raupp P, Hassan JA, Varughese M, Kristiansson B, Henna causes life threatening haemolysis in glucose-6-phosphate dehydrogenase deficiencyArch Dis Child 2001 85:411-12. [Google Scholar]
[16]. Ilkhanipur H, Hakimian N, Henna: A cause of life threatening hemolysis in G6PD-deficient patientPak J Med Sci 2013 29(1 Suppl):429-31. [Google Scholar]
[17]. Seyedzadeh A, Hemmati M, Gheiny S, Henna – induced severe hemolysis: In Glucose 6 – Phosphate Dehydrogenase DeficiencyPak J Med Sci 2007 23(1):119-21. [Google Scholar]