Large Isolated Major Aortopulmonary Collateral Artery Causing Severe Pulmonary Hypertension in an Infant: A Rare and Challenging Diagnosis
Brajesh Kumar Kunwar1, Snigdha Paddalwar2, Mahesh Ghogare3
1 Senior Consultant Interventional Cardiologist and Head, Department of Cardiology, Fortis Hiranandani Hospital, Navi Mumbai, Maharashtra, India.
2 Pediatric Cardiac Anaesthetic, Department of Cardiology, Seven Hills Hospital, Mumbai, Maharashtra, India.
3 Consultant Cardiologist, Department of Cardiology, Seven Hills Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Brajesh Kumar Kunwar, Senior Consultant Interventional Cardiologist and Head, Fortis Hiranandani Hospital, Mini Sea Shore Road, Sector 10, Vashi - 400703, Navi Mumbai, Maharashtra, India.
E-mail: kunwar_brajesh@yahoo.com
Major Aortopulmonary Collateral Artery (MAPCA) as an isolated congenital anomaly, without evidence of any structural heart disease, is a very rare observation. Previously published reports indicate that symptomatic infants with large isolated MAPCA usually present with congestive heart failure or recurrent respiratory tract infections. To the best of our knowledge, the present case of an infant with large isolated MAPCA is a unique case with a diagnostic dilemma due to presentation with severe pulmonary hypertension as a predominant sign. The infant was managed successfully by percutaneous obliteration with amplatzer vascular plugs, along with perioperative and postoperative sildenafil.
Amplatzer vascular plug, Computed tomography angiogram, Sildenafil
Case Report
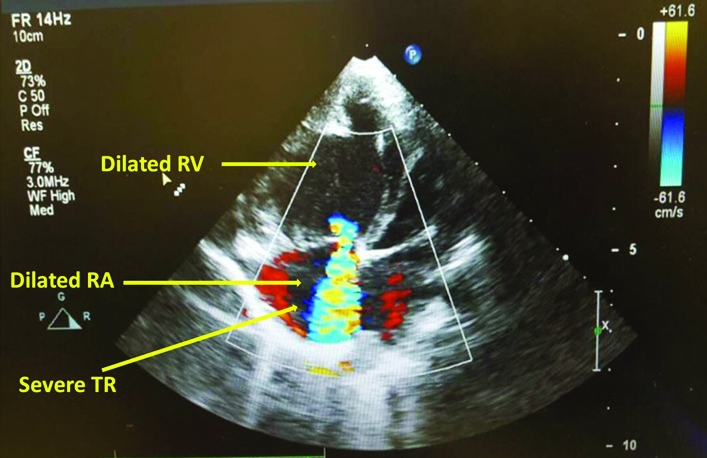
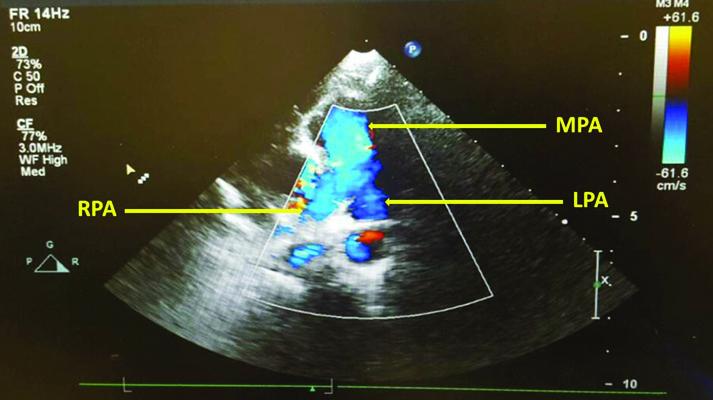
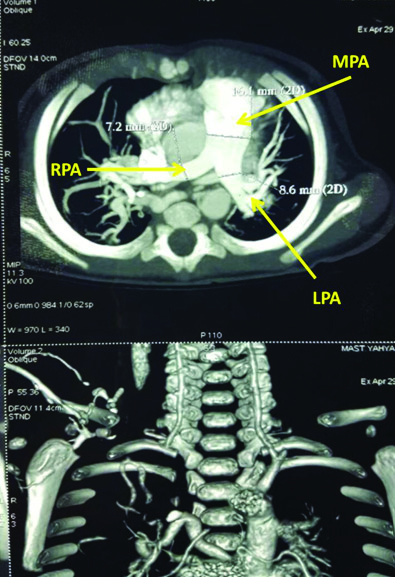
A five-month-old male baby (weight: 4 kg) was presented with chief complaints of recurrent respiratory tract infection, shortness of breath, and failure to thrive. He was born by a normal vaginal delivery with birth weight of 2.3 kg. He became symptomatic at the age of 2 months with suck-rest–suck cycles, respiratory tract infection, and failure to thrive. A month back, he was hospitalized for pneumonia and repeated respiratory failure. He was kept on anti-failure medications comprising furosemide 2 mg twice daily and ramipril 0.2 mg once daily. On clinical examination, he displayed tachypnoea, irritability, excessive crying, intercostal and subcostal retractions, and tachycardia, with no signs of congestive cardiac failure. He had loud P2 with harsh continuous murmur dominantly heard on right interscapular, infrascapular, and right parasternal area. Chest X-ray showed cardiomegaly and pulmonary plethora of moderate severity mainly in the right lung. Echocardiography showed severe tricuspid regurgitation and severely dilated right atrium, right ventricle, and pulmonary arteries [Table/Fig-1,2]. Pulmonary artery pressure, derived by tricuspid regurgitation jet velocity, was suprasystemic (111 mmHg). No other structural abnormality was seen. Computed Tomography (CT) angiogram showed a large MAPCA, arising from the descending thoracic aorta and supplying blood to the right upper and middle lobes [Table/Fig-3,4]. In view of worsening symptoms, we decided to carry out percutaneous closure of MAPCA.
Echocardiography showing severe tricuspid regurgitation (TR) and dilated right atrium (RA) and right ventricle (RV).
Echocardiography showing dilated confluent pulmonary artery with normal branching pattern - left pulmonary artery (LPA), main pulmonary artery (MPA) and right pulmonary artery (RPA).
CT angiogram showing normal branching left pulmonary artery (LPA), main pulmonary artery (MPA) and right pulmonary artery (RPA).
CT angiogram showing a large major aortopulmonary collateral artery (MAPCA), arising from the descending thoracic aorta and supplying blood to upper and middle lobe of right lung.
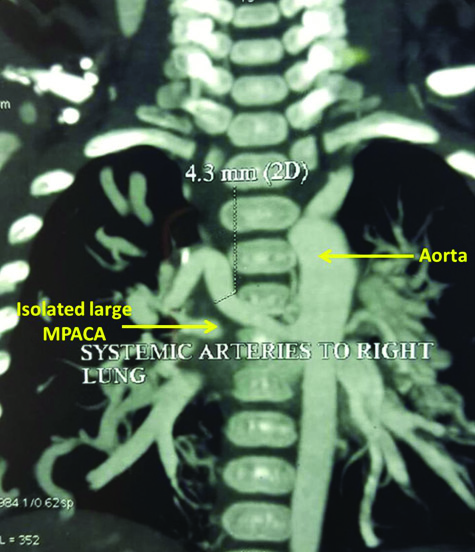
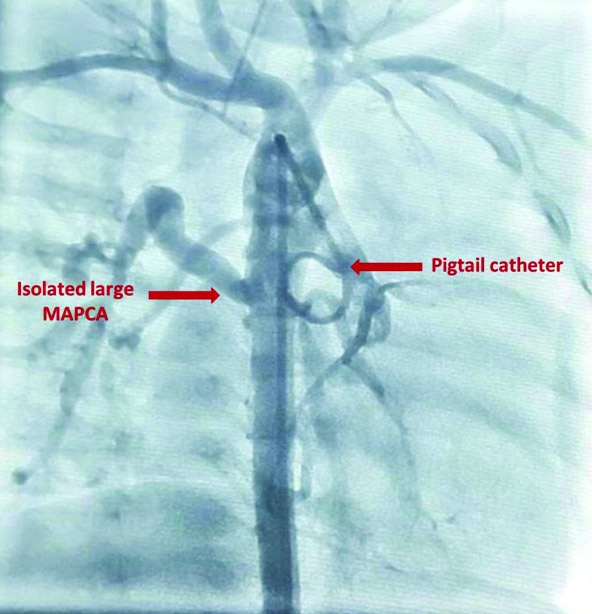
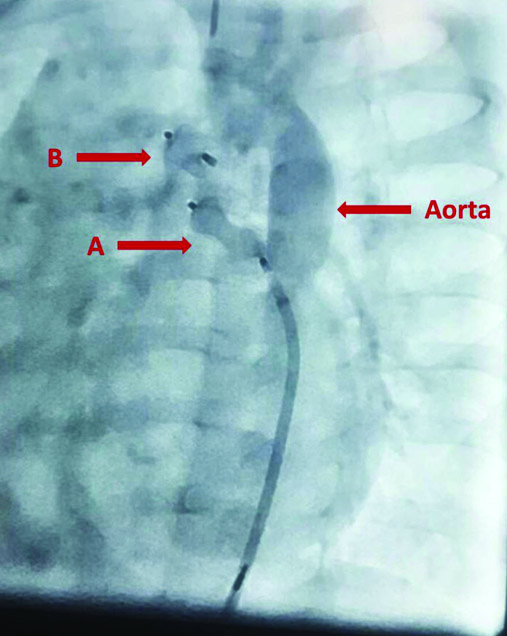
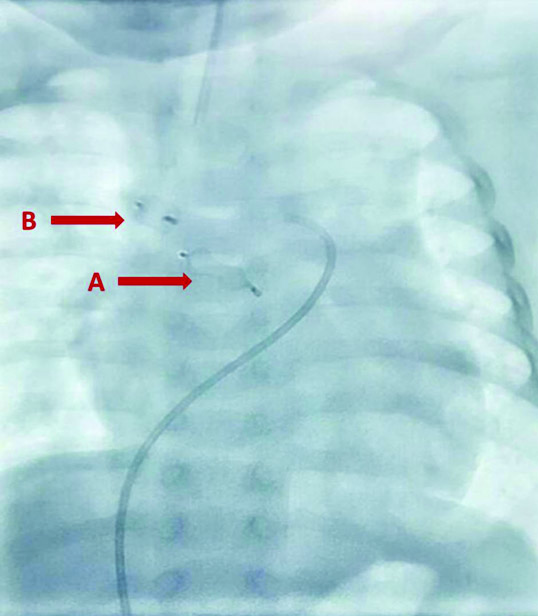
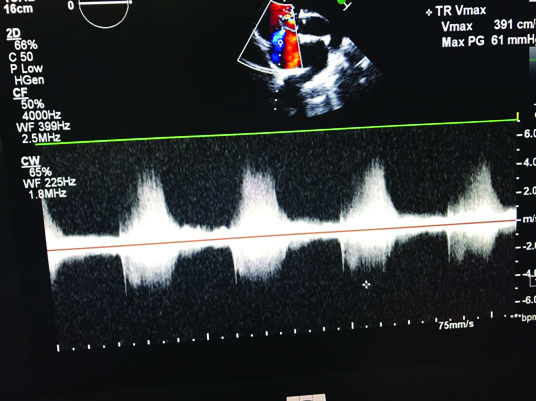
Considering the presence of severe pulmonary hypertension, the procedure was performed under general anaesthesia using ketamine 10 mg and midazolam 0.5 mg and was maintained with sevoflurane 2%. The airway was secured with 4F endotracheal tube. Sildenafil infusion was started at 70 µg/kg/hour. Right femoral vascular access was obtained. Descending aortic angiogram and subsequent selective angiogram in antero-posterior and lateral views showed a large MAPCA of 5 mm diameter at T7-8 level and dual blood supply to right upper and middle lobes [Table/Fig-4]. The levo-phase of pulmonary angiogram showed pulmonary venous drainage to the left atrium [Table/Fig-5]. Subsequently, the MAPCA was engaged and obliterated by delivering Amplatzer vascular plugs (St. Jude Medical, Minnesota, USA) of 6 mm and 8 mm sizes sequentially [Table/Fig-6,7]. Anaesthesia was reversed and the baby was extubated at the end of successful procedure. Sildenafil infusion was stopped on next day and oral sildenafil 1 mg/kg thrice daily was started along with anti-failure therapy comprising furosemide syrup 2 mg twice daily and ramipril 0.4 mg once daily. On follow-up after a week, the baby remained symptom free with normal breathing pattern and improved acceptance of feeds. Echocardiography revealed that sizes of right atrium and right ventricle were significantly reduced and pulmonary artery pressures were subsystemic [Table/Fig-8].
Aortogram image in cathlab showing large isolated major aortopulmonary collateral artery (MAPCA) arising from descending thoracic aorta.
Successful delivery of (A) Proximal vascular plug of 8 mm size and (B) Distal vascular plug of 6 mm size.
Vascular plugs in-situ (A) Proximal vascular plug (post-release), (B) Distal vascular plug (post-release).
Follow-up echocardiography showing significant reduction in right atrium and right ventricle sizes and subsystemic pulmonary artery pressures.
Discussion
Major Aortopulmonary Collateral Artery (MAPCA) is an anomalous blood vessel that develops from aorta or its main branches and connects with pulmonary arteries [1]. It causes increase in pulmonary blood flow and serves as an additive or the only source of blood supply to lungs [2]. MAPCA are usually seen in association with cyanotic congenital heart diseases like pulmonary atresia or tetralogy of fallot, where pulmonary arteries do not develop and collaterals continue to grow to become the main supply of blood to the lungs [1]. In very rare cases, MAPCA are seen in ‘isolation’ without any congenital heart disease [1-5]. Although isolated MAPCA regress spontaneously in majority of cases [2], surgical intervention in initial few weeks of life becomes essential as large isolated MAPCAs may cause pulmonary hypertension, broncho-pulmonary dysplasia, recurrent lower respiratory tract infections, and congestive cardiac failure [1]. Here, we describe a case of large isolated MAPCA in an infant presenting with severe pulmonary hypertension and recurrent respiratory tract infection, which was creating a case of diagnostic dilemma initially. Presence of MAPCA in absence of any structural abnormality of heart is one of the distinctive clinical features in the present case. It should also be noted that MAPCAs without congenital heart disease are generally seen in preterm babies [1]. Further, a study had reported that 66% of premature infants with very low birth weight (<1500 gm) had MAPCA [4]. In contrast, infant in the present case with large MAPCA was born at full-term through a normal delivery. Aetiology of isolated MAPCA remains a matter of investigation in the present case. Majority of such published cases on isolated MAPCA presented with predominant symptoms of congestive heart failure or recurrent respiratory tract infections [1-4]. In this case, infant with similar anomaly had severe pulmonary hypertension as predominant clinical sign. To the best of our knowledge, this is the rarest case of an infant with a large isolated MAPCA, presenting with severe pulmonary hypertension, and managed successfully with percutaneous intervention using vascular plugs.
Birth history, course after birth, and clinical investigations ruled out other likely causes of pulmonary hypertension. In the present case, the MAPCA suspicion was there in echo because of the presence of severe pulmonary arterial hypertension and dilated pulmonary arteries with absence of intra cardiac shunts. However, it was not appreciated probably because of its large size and probably because the flow was not producing turbulence, causing echo jet. The presence of MAPCA lower down in descending thoracic aorta might be the reason for missing it in echocardiogram. Further, the absence of structural heart disease upon echocardiographic examination made us look for rare causes. Subsequently, CT angiogram indicated the presence of large isolated MAPCA. The most important differential diagnosis of isolated MAPCA includes anomalous right pulmonary artery arising directly from aorta. However, echocardiogram and CT pulmonary angiogram clearly demonstrated normal origins of right, left and main pulmonary arteries. Here, we recommend CT angiography over conventional angiography in cases indicative of aortopulmonary collaterals. It is reported that CT is valuable in the assessment of MAPCAs as it provides details about their sites of origin, their varying diameters, their courses, and the areas of the lungs they supply, which may offer an efficient road map for safe and successful selective catheterization [6].
While conservative management is usually sufficient in majority of cases [4], infant in the present case required percutaneous closure of MAPCA in view of worsening symptoms. Although embolization coils are generally used to manage aortopulmonary collaterals [1,3-5], they are likely to fail in cases of large-sized MAPCA [7]. Amplatzer vascular plug device is found safe and effective for percutaneous closure of aortopulmonary collaterals, specifically of large dimensions [7]. Considering this, the infant was managed successfully by deploying two Amplatzer vascular plugs. We believe that this is the first such case of multiple vascular plugs deployed sequentially. In addition, we used sildenafil to prevent pulmonary hypertensive crises and acute right ventricular failure. We suggest that differential diagnosis for isolated MAPCA should be considered in infants with severe pulmonary hypertension and symptoms suggestive of aortopulmonary collaterals. Early diagnosis and intervention can prevent further damage to the lungs leading to irreversible pulmonary hypertension.
Conclusion
In neonates or infants with severe pulmonary hypertension, all secondary or treatable causes of pulmonary hypertension are required to be ruled out. Early recognition of treatable causes can improve survival. The present case of an infant with large isolated MAPCA is a unique case with a diagnostic dilemma due to presentation with severe pulmonary hypertension as a predominant sign. The infant was managed successfully.
[1]. Tinmaswala MA, Saple PP, Gupta A, Isolated major aortopulmonary collateral artery causing CCF in a newborn: a case reportInt J Med Res Health Sci 2015 4:471-73. [Google Scholar]
[2]. Patra S, Srinivas SK, Agrawal N, Jayaranganath M, Isolated major aortopulmonary collateral artery in an infant presenting with recurrent lower respiratory tract infectionBMJ Case Rep 2013 2013:bcr2013200421 [Google Scholar]
[3]. Padhi SS, Bakshi KD, Shastri RK, Multiple coil closure of isolated aortopulmonary collateralAnn Pediatr Cardiol 2010 3:65-67. [Google Scholar]
[4]. Acherman RJ, Siassi B, Pratti-Madrid G, Luna C, Lewis AB, Ebrahimi M, Systemic to pulmonary collaterals in very low birth weight infants: color Doppler detection of systemic to pulmonary connections during neonatal and early infancy periodPediatrics 2000 105:528-32. [Google Scholar]
[5]. Holzer R, Ladusans E, Malaiya N, Aortopulmonary collateral arteries in a child with trisomy 21Cardiol Young 2002 12:75-77. [Google Scholar]
[6]. Maeda E, Akahane M, Kato N, Hayashi N, Koga H, Yamada H, Assessment of major aortopulmonary collateral arteries with multidetector-row computed tomographyRadiat Med 2006 24:378-83. [Google Scholar]
[7]. Tissot C, Da Cruz E, Beghetti M, Aggoun Y, Successful use of a new amplatzer vascular plug for percutaneous closure of a large aortopulmonary collateral artery in a pulmonary atresia with ventricular septal defect prior to complete repairInt J Cardiol 2007 116:e39-41. [Google Scholar]