Introduction
Various methods have been used for management of equinus deformity. However, stretching gastroc-soleus muscle and achilles tendon is a difficult task. It is labour intensive, which makes the provision of treatment difficult for many patients.
Aim
To study the effectiveness of Tension Bar Tendon Stretch (TBTS) compared to conventional stretching in patients with equinus deformity in terms of improvement in equinus angle and spasticity.
Materials and Methods
A prospective randomised case control study was done on 16 patients of both the sexes in the age group four years to 56 years. Patients were stratified based on presence or absence of spasticity. Patients were further randomly allotted to the study or control group. Study group received stretching with TBTS in addition to the conventional rehabilitation programme. Patients were assessed in terms of improvement in equinus deformity and spasticity (modified Ashworth scale). These indices were measured at 0 month (pre-treatment), 1 month (post-treatment), and 6 months (follow up).
Results
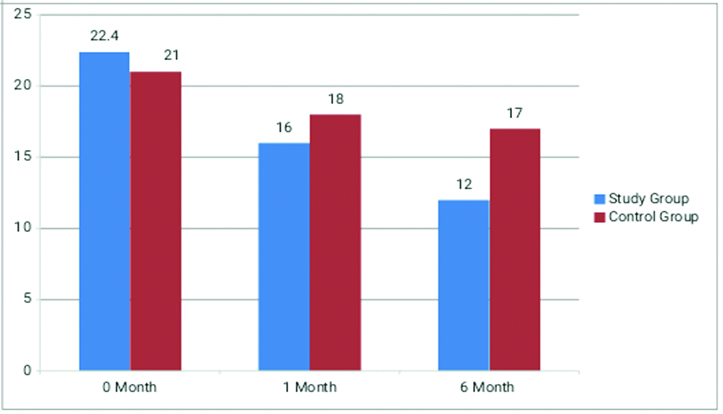
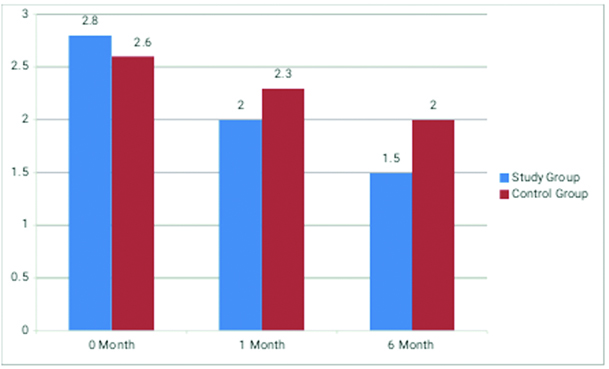
Equinus deformity in patients with spastic equinus changed from 22.4° to 12° in study group while in control group change was from 21° to 17°. The difference was statistically significant with p-value of 0.001. Non-spastic (post accidental) changed from 30° to 15° in study group while in control group change was from 31° to 23° with p-value of 0.001. Modified Ashworth Score (MAS) was assessed only in spastic equinus, while in study group MAS changed from 2.8 to 1.5 and MAS change was 2.6 to 2 in control group; this difference after six months of therapy was statistically significant with a p-value of 0.001.
Conclusion
TBTS can be an effective tool in rehabilitation of patients having equinus deformity; it provides an effective and patient controlled stretching and no need for a physical therapist. TBTS is a novel but simple instrument that can be made locally by the patient or the family.
Introduction
The condition in which ankle dorsiflexion is restricted is known as equinus deformity [1]. There is inconsistency regarding the magnitude of reduction in dorsiflexion required to constitute a diagnosis of equinus deformity [2]. Equinus deformity is a common complication of central and peripheral nervous system disorders [3].
Equinus deformity and gait: Gastrocsoleus muscle is the most consistently active muscle during static stance due to the centre of gravity projecting anterior to the ankle. During ambulation, the ankle must dorsiflex past perpendicular for smooth ambulation and allow heel to contact the supporting surface. Equinus decreases stability during walking, causing loss of the smooth translation of the body over the foot during stance phase of gait, and often leads to inadequate clearance of the foot during the swing phase of gait [4].
In the presence of equinus deformity biomechanics of foot is altered resulting in distal and proximal compensations. Common modes of compensation for lack of ankle dorsiflexion include triplanar rearfoot motion (pronation), hypermobile flatfoot, an early heel-off (bouncy gait), and abducted gait pattern. Proximal compensatory patterns include lumbar lordosis, hip flexion and genu recurvatum. If equinus deformity is only partially compensated, it results in increased forefoot load causing calluses, metatarsalgia and forefoot ulceration [4].
Various changes have been seen in muscle itself secondary to spasticity including variable muscle fibre size and type, proliferation of extracellular matrix material with inferior mechanical properties [5]. Connective tissue which is composed of loose tissue, tendons, ligaments, bones, cartilage and blood vessels. These tissues are complex and at the same time dynamic structures that are important for structural support, stabilization and movement [6].
Tendons are mostly collagen and elastin. Ligaments are mostly made of collagen. Strength of connective tissue depends on direction and magnitude of mechanical loads. Connective tissue structure and composition changes and responds to change in functional situation, particularly to changes in the applied mechanical stresses. Presence of stretch, weight bearing, joint mobilization and muscle contraction results in synthesis of connective tissue and their absence results in its degradation. Changes in collagen diameter, density and orientation follow Wolff’s law that is “connective tissue orient in form and mass to best resist extrinsic forces”. Proteoglycans are important for lubrication, spacing and gliding. Proteoglycans are responsible for free gliding of tissues. Proteoglycan concentration decreases by immobility and leading to gelling of the joints; causing restriction in range of motion or a fixed deformed contracture [7]. Some other factors like inflammation, haemorrhage, degeneration and ischemia further causes replacement of normal connective tissue with shortened and abnormal connective tissue [8].
Microscopic findings of equinus deformity seen in diabetes mellitus shows many areas of tendon has masses of closely adhering fibrillae. In addition, collagen fibrils appear twisted, curved, overlapped and highly disorganized. Such structural changes contribute to the phenomenon consistent with clinical observations of shortening of the Achilles tendon-gastrocnemius-soleus complex [9].
Most frequently equinus results from two or more processes that cause pathologic changes in the joint and adjacent tissues. It could result from an arthrogenic contracture, soft and dense tissue contracture, myogenic contracture or as a compensation to limb length deficiency or weak quadriceps [4,10].
Management of equinus deformity: Depending on the cause there is a variety of arsenal in the repertoire of physiatrist for management of equinus deformity. The distinction between dynamic and a fixed equinus deformity is critical in clinical decision making. Although dynamic tightness might be addressed by using conservative treatments, fixed muscle contracture represents an indication for surgery [11]. Treatments include stretching [12], strengthening of antagonist muscle group [13], electrical stimulation [14], serial casting [15], splinting [16], oral medications [17], botulinum toxin injections [18], selective dorsal rhizotomy [19] and Intrathecal Baclofen Infusion (ITB) [20].
Patients with fixed equinus deformity end up in some sought of surgery [11,21,22]. The foot and ankle surgeon will determine the type of procedure that is best suited to the individual patient.
As seen contracture can be because of different aetiologies, involving different tissues. Stretch is the main stay of restoring ankle range of motion. Stretch is widely used to treat and prevent contractures. There is variety of methods of stretching of GS and TA that are taught to the patients as shown in [Table/Fig-1].
Types of conventional stretching: a) Step stretch; b) Wall stretch; c) Active stretch; d) Towel stretch; e) Passive stretch; and f) Common Indian relaxing posture.

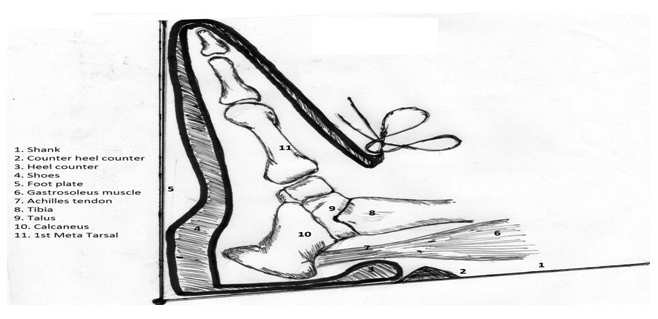
Physiatrist who has knowledge of exercises and orthotics can provide a combination of two disciplines to help the problem, in the form of Tension Bar Tendon Stretch (TBTS) [Table/Fig-2]. It is a mechanical device that stretches the gastrocsoleus complex by lever action. The mechanical advantage of a lever can be determined by considering the balance of Torque, T, about the fulcrum.
Components of TBTS 1-Foot Plate, 2-Hinge, 3-Lever, 4-Shank, 5-Leather strap shin, 6-Leather strap ankle, 7-Leather strap foot, 8-Counter heel;
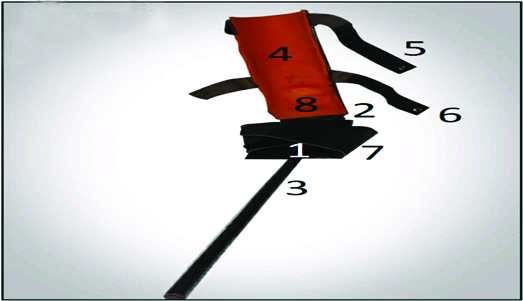
The device is worn like an ankle foot orthosis the foot strap and shin strap provide the two points while the ankle strap and the counter heel provide the third point to provide the three point correctional force. Long rod provides the lever action for additional correction.
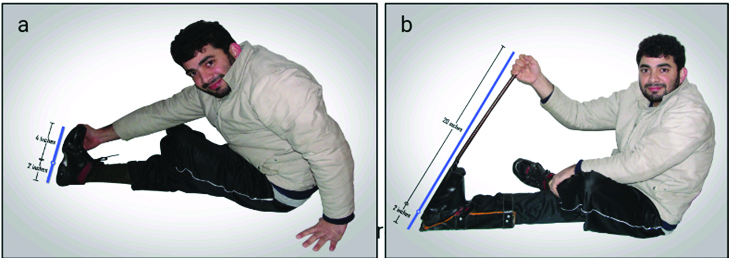
Principle of action of the device TBTS: To stretch a powerful muscle like GS or a strong tendon like TA by conventional methods, the lever action arm is in the ratio of 2:4 however the lever action arm ratio increases to 2:20 using TBTS so five times greater torque is generated by same amount of stretch [Table/Fig-3].
a) Lever arm ratio of stretching with TBTS as 2:4; b) Lever arm ratio of stretching with TBTS as 2:20.
Using TBTS stretching occurs by the overriding of the Golgi tendon reflex over the stretch reflex causing further inhibition of the muscle spindles of the stretched gastroc-soleus muscle allowing stretch to a greater limit.
An alternative explanation can be the observation of Flower KR et al., in which they tested the Total End Range Time (TERT) theory. This theory claims that the amount of increase in Passive Range of Motion (PROM) of a stiff joint is proportional to the amount of time the joint is held at its end range, or total end range time; according to this theory the tissue is lengthened by creeping of the molecules rather than stress relaxation [23].
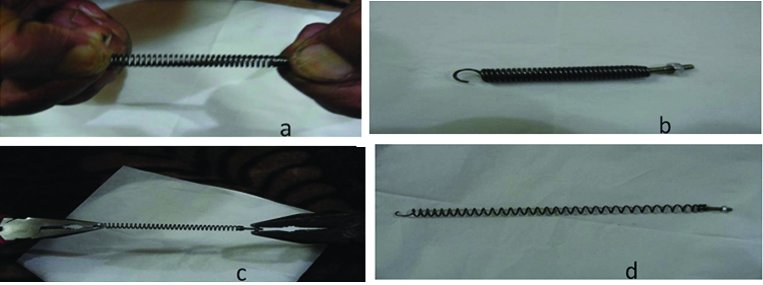
Usual stretching therapy for equinus deformity operates by stress relaxation of deformed connective tissue and realigning the connective tissue in the direction of stretching and the tissue recoils back to original shape ones the stretch is released. TBTS attempts to stimulate continuous lengthening by creep rather than stress relaxation as seen by Flower KR et al., [23]. A metaphor can be seen in [Table/Fig-4].
(a) and (b) Stretching a spring with hands lengthens but then recoils to original shape when the tension is released. (c) and (d) Stretching the same spring with pliers a class 2 lever permanently deforms the spring and it creeps to new length.
Materials and Methods
A prospective stratified randomized case control study was conducted in Department of PMR of a tertiary care hospital from July 2014 to July 2016. Patients of both genders and all age groups were included in the study. Patients were stratified based on presence of spasticity; further the included subjects were randomly allotted in study or control group. Study group was given 30 minutes of TBTS therapy [Table/Fig-5,6] in addition to the conventional stretching exercises. Ethical committee approval was taken before initiating the study and informed consent was taken from all patients.
a) front view of the inside of TBTS showing counter heel just above the hinge that locks the shoes when doing the stretching; b) lateral view of TBTS showing long lever created by the extension rod.
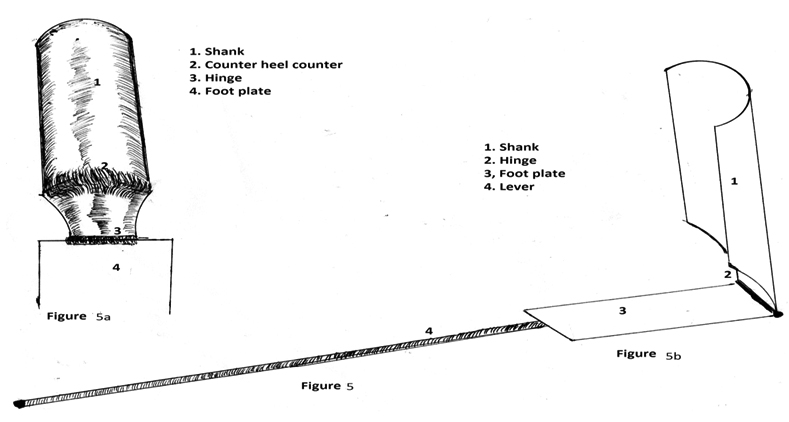
Shows the lateral view of the device with gastroc-soleus and tendo-achillis being stretched, clearly showing how heel counter gets locked by the counter heel from upward translation.
Patients with spasticity were assessed in terms of angle of equinus deformity and spasticity. Those patients who did not have spasticity were assessed only in terms of angle of equinus deformity. Spasticity was assessed in terms of Modified Ashworth Scale (MAS). The patients were assessed at 0 month, 1 month and 6 months. Inclusion criteria was; equinus only due to soft tissue shortening and good hand function. Equinus due to bony deformity was excluded from the study.
Results
Sixteen patients with equinus deformity were enrolled in the project; eight were included in the study group and eight in control group. Six patients had spinal cord injury, two had stroke, four were post accidental foot injury causing equinus, and four had cerebral palsy. Age varied from four years to 56 years. There were 10 males and six females patients.
All patients completed six months of therapy. Males were more common in both the study (83.3%) and control (76.7%) groups. Educational status of the patients varied from no education to post-graduation level in both study and control groups. Majority of patients were of poor socio-economic status, 65% and 70% in study and control groups respectively. Other baseline characteristics have been shown in the [Table/Fig-7].
Baseline characteristics.
| Characteristic at Baseline | Study Group (n=8) | Control Group (n=8) | p-value |
|---|
| Mean age in years | 27.97±13.99 | 29.13±10.69 | 0.73 |
| Mean duration in months spastic equinus | 18.37± 10.88 | 22.80 ± 11.96 | 0.61 |
| Mean duration in months non spastic equinus | 4.67± 1 | 4.8±1 | 0.66 |
| Spastic equinus | 22.4° ± 0.805° | 21° ± 0.847° | 0.98 |
| Non spastic equinus | 30° ± 2.5° | 31° ± 2° | 1.06 |
| Modified Ashworth score spastic equinus | 2.8 ± 0.34 | 2.6 ± 0.45 | 0.782 |
Equinus deformity [Table/Fig-8,9]: In spastic equinus after one month of therapy and exercise programme in study group and control group, there was a statistically significant decrease in equinus within 95% confidence interval (p<0.001 by t-test) at one month (16.0° ± 1.088° vs 18.23° ± 0.679°) and six months (12.0°±1.08 vs 17°±1.21°).
Average degree of equinus in spastic equinus (n=10).
Average degree of equinus in non spastic (n=6).
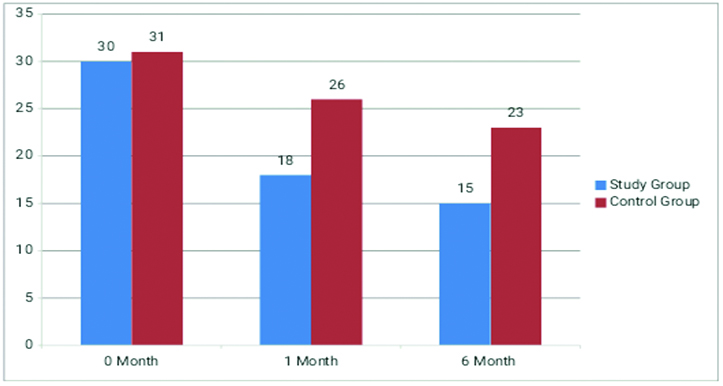
In non spastic equinus after one month of therapy and exercise programme in study group and control group, there was a statistically significant decrease in equinus 95% confidence interval (p<0.001 by t-test) at one month (18.0°±1° vs 26°±2°) and six months (15.0°±1° vs 23°±2.1°).
Modified Ashworth score [Table/Fig-10]: MAS was analysed only in the spastic equinus deformity, one month after the exercise and TBTS therapy; there was a statistically significant improvement in spasticity in study group (mean MAS 2±0.11) compared to the control group (mean MAS 2.3±0.60), p-value 0.04. Improvement further increased in the study group to 1.5±0.23 vs 2±0.55, p-value <0.001 on six months follow up.
Average Modified Ashworth Scale in spastic equinus (n=10).
Discussion
This study showed that stretching is an important component after most of the interventions that needs to be given to the patients with equinus deformity and further found that the stretching with TBTS was far more effective than conventional methods of stretching.
Grady et al., had a mean (±SD) increase in ankle dorsiflexion of 2.15°±3.25° after 30 seconds of daily stretching for six months, 2.30°±2.98° with a 2-minute daily program, and a third group demonstrated a mean (±SD) increase of 2.70°±3.90° with a 5-minute daily stretching program. Only the increase shown by the third group (five minutes of daily calf stretching) was statistically significant. Showing that stretching causes increase in range of motion however this increase is dependent on amount of time spent for stretching and the change may not be statistically significant [24].
Giovannelli M et al., compared patients of multiple sclerosis who received botulinum toxin A with stretching regimens (study group) and botulinum toxin A alone (control group). Two weeks post injection MAS was 2.73 in study group compared to the control group with MAS of 3.22, the difference was statistically significant (p <0.01 by t-test). This difference continued at 4 week and 12 week follow up. The combined treatment proved also to be more effective by patient perceived symptomatic improvement on visual analogue scale (p < 0.01) at week 4 (6.95 versus 5.50) and at week 12 (7.86 versus 6.56) but not at week 2 (5.18 versus 5.50; p = 0.41). They concluded that stretching in combination with botulinum toxin type A injection can improve overall response to botulinum toxin [25].
Surgical treatment in equinus deformity is not required in dynamic equinus. It is needed in those patients with fixed deformity and contractures. Joo SY et al., found a moderate rate of recurrence (43.8%) of equinus after surgery and recurrence risk factors were age at primary surgery and pattern of CP. Recurrence can occur at any age while the child is still growing; therefore, it is advised to follow those patients until they reach skeletal maturity [26]. In our setup, patients are advised to use Ankle Foot Orthosis (AFO) postoperatively and to do regular stretching to prevent relapse.
Katalinic OM et al., did a systemic review to determine the effectiveness of stretching for treatment and prevention of contractures, 25 studies were meta-analysed. They found stretch had small immediate effect, and small or no short term or long term effect on joint mobility. They concluded regular stretch did not produce clinically important changes in joint mobility, pain, spasticity or activity limitation in people with neurological conditions. Limitation of the review was that all the studies meta analysed investigated effect of stretch for less than six months [9]. As discussed in principle of action conventional stretching is far less effective and labour intensive, hence there is small or no sustained effect. Stretching with TBTS is self-directed, easy, less effort needed and more effective, because of lever mechanism and creeping effect [11]. A comparison between the advantages and disadvantages has been tabulated in [Table/Fig-11].
Advantages vs disadvantages of TBTS.
| Advantages of TBTS | Disadvantages of TBTS |
|---|
| TBTS generates 5 times torque. Stretch applied is determined by the user. TBTS and similar devices can be used for stretching of joints with short lever arm. Force generated by lever is transmitted to a large interface. The device is universal. Easy to don and doff. Cost of device. | TBTS needs good upper limb function. Excess of torque might cause pressure on the calcaneus. Upward sliding of heel may happen. Stretching with TBTS needs a device. |
Limitation
Limitation of the study was small number of patients tested in the study, unavailability of the device in the market; researcher had to get it made for each subject.
Conclusion
In our era of instant gratification, the world of rehabilitation seems like an outlier. The path from a promising discovery to an effective treatment often takes a decade or more. TBTS is one such attempt to make a leap towards application of science for patient empowerment. Concern has been raised by the experts that this device might put a pressure on the head of metatarsal and cause a break in foot. One study is in progress in our institute to see its benefits and drawbacks. More studies need to be carried out to study its effectiveness, to improve its design and to explore other areas in which it or similar devices could be applied.
[1]. Digiovanni CW, Holt S, Czerniecki JM, Ledoux WR, Sangeorzan BJ, Can the presence of equinus contracture be established by physical exam alone?Journal of Rehabilitation Research and Development 2001 38(3):335-40. [Google Scholar]
[2]. Charles J, Scutter SD, Buckley J, Static ankle joint equinus: toward a standard definition and diagnosisJ Am Podiatr Med Assoc 2010 100(3):195-203. [Google Scholar]
[3]. Fergusson D, Hutton B, Drodge A, The epidemiology of major joint contractures: a systematic review of the literatureClin Orthop Relat Res 2007 456:22-29. [Google Scholar]
[4]. Johnson CH, Christensen JC, Biomechanics of the first ray part V: The effect of equinus deformity. A 3 dimensional kinematic study on a cadaver modelThe Journal of Foot and Ankle Surgery 2005 44(1):114-18. [Google Scholar]
[5]. Lieber RL, Steinman S, Barash IA, Chambers H, Structural and functional changes in spastic skeletal muscleMuscle Nerve 2004 29:615-27. [Google Scholar]
[6]. Alberts B, Bray D, Lewis J, Johnson A, Raff M, Walter P, Molecular biology of the cell 1983 New YorkGarland Science:673-715. [Google Scholar]
[7]. Harper J, Amiel D, Harper E, Collagenases from periarticular ligaments and tendon: enzyme levels during the development of joint contractureMatrix 1989 9:200-05. [Google Scholar]
[8]. Grant WP, Sullivan R, Sonenshine DE, Adam M, Slusser JH, Carson KA, Electron microscopic investigation of the effects of diabetes mellitus on the Achilles tendonJ Foot Ankle Surg 1997 36(4):272-78. [Google Scholar]
[9]. Karpakka J, Vaananen K, Orava S, Takala TE, The effects of preimmobilization training and immobilization on collagen synthesis in rat skeletal muscleInt J Sports Med 1990 11:484-88. [Google Scholar]
[10]. Halar EM, Kathleen RB, Fontera WR, Delisa JA, Physical Inactivity: Physiological and Functional Impairments and Their TreatmentPhysical Medicine and Rehabilitation Principles and Practice 2010 PhiladelphiaWolters Kluwer/Lippincott Williams and Wilkins:1255 [Google Scholar]
[11]. Svehlík M, Zwick EB, Steinwender G, Kraus T, Linhart WE, Dynamic versus fixed equinus deformity in children with cerebral palsy: how does the triceps surae muscle work?Arch Phys Med Rehabil 2010 91:1897-903. [Google Scholar]
[12]. Katalinic OM, Harvey LA, Herbert RD, Effectiveness of stretch for the treatment and prevention of contractures in people with neurological conditions: a systematic reviewPhys Ther 2011 91:11-24. [Google Scholar]
[13]. Bhakta BB, Management of spasticity in strokeBritish Medical Bulletin 2000 56(2):476-85. [Google Scholar]
[14]. Detrembleur C, Lejeune TM, Renders A, Van den Bergh PYK, Brief report botulinum toxin and short-term electrical stimulation in the treatment of equinus in cerebral palsyMovement Disorders 2002 17(1):162-69. [Google Scholar]
[15]. Pohl M, Ru¨ckreim S, Mehrholz J, Ritschel C, Strik H, Pause MR, Effectiveness of serial castingin patients with severe cerebral spasticity: a comparison studyArch Phys Med Rehabil 2002 83:784-90. [Google Scholar]
[16]. Dursun E, Dursun N, Alican D, Ankle-foot orthoses: eVect on gait in children with cerebral palsyDisability and Rehabilitation 2002 24(7):345-47. [Google Scholar]
[17]. Prakash O, Singh U, Yadav SL, Kishore K, Handa G, Dwivedi SN, Effect of alprazolam in spasticity: a pilot studyIJPMR 2009 20(1):6-12. [Google Scholar]
[18]. Smith P, Turkel C, Walcott JM, Molloy PT, Botulinum toxin type a neuromuscular blockade in the treatment of equinus foot deformity in cerebral palsy: a multicenter, open-label clinical trialPediatrics 2001 108:1062-71. [Google Scholar]
[19]. Buckon CE, Thomas SS, Pierce R, Piatt JH, JrAiona MD, Developmental skills of children with spastic diplegia: functional and qualitative changes after selective dorsal rhizotomyArch Phys Med Rehabil 1997 78:946-51. [Google Scholar]
[20]. Meythaler JM, Guin-Renfroe S, Brunner RC, Hadley MN, Intrathecal baclofen for spastic hypertonia from strokeStroke 2001 32:2099-109. [Google Scholar]
[21]. Lamm BM, Paley D, Herzenberg JE, Gastrocnemius soleus recession a simpler, more limited approachJ Am Podiatr Med Asso 2005 95(1):18-25. [Google Scholar]
[22]. Shore BJ, White N, Graham HK, Surgical correction of equinus deformity in children with cerebral palsy: a systematic reviewJ Child Orthop 2010 4:277-90. [Google Scholar]
[23]. Flower KR, LaStayo PC, Effect of total end range time on improving passive range of motionJ Hand Ther 1994 7(3):150-57. [Google Scholar]
[24]. Grady JF, Saxena A, Effects of stretching the gastrocnemius muscleJ Foot Surg 1991 30:465 [Google Scholar]
[25]. Giovannelli M, Borriello G, Castri P, Prosperini L, Pozzilli C, Early physiotherapy after injection of botulinum toxin increases the beneficial effects on spasticity in patients with multiple sclerosisClin Rehabil 2007 21(4):331-37. [Google Scholar]
[26]. Joo SY, Knowtharapu DN, Rogers KJ, Holmes L, JrMiller F, Recurrence after surgery for equinus foot deformity in children with cerebral palsy: assessment of predisposing factors for recurrence in a long-term follow up studyJ Child Orthop 2011 5:289-96. [Google Scholar]