Upper Gastrointestinal Bleed as a Manifestation of Poorly Differentiated Metastatic Squamous Cell Carcinoma of the Lung
Richa Bhardwaj1, Gaurav Bhardwaj2, Arun Gautam3, Raffi Karagozian4
1 Resident, Department of Internal Medicine, University of Connecticut, Farmington, Connecticut, USA.
2 Research Student, Department of Internal Medicine, University of Connecticut, Farmington, Connecticut, USA.
3 Resident, Department of Internal Medicine, University of Connecticut, Hartford, Connecticut, USA.
4 Attending Physician, Department of Gastroenterology and Hepatology, University of Connecticut, Farmington, Connecticut, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Richa Bhardwaj, 24 Park Place apt B6E, Hartford, Connecticut, USA.
E-mail: dr.richabhardwaj@gmail.com
Gastrointestinal (GI) metastasis from primary lung cancer is a rare clinical finding. Lung cancer most often metastasizes to the brain, bone, liver, and adrenal glands; with gastrointestinal involvement being very rare. We report a case of a 39-year-old female with a diagnosis of poorly differentiated Squamous Cell Carcinoma (SCC) of the lung presenting with dizziness and melena. Esophagogastroduodenoscopy (EGD) showed a bleeding mass in the stomach. Final biopsy report and Immunohistochemistry (IHC) of the specimen were consistent with SCC lung metastasis. While it is imperative to have a high clinical suspicion for GI metastasis in patients with primary lung cancer presenting with GI symptoms, it may be challenging to establish diagnosis. Endoscopy along with pathology and immunohistochemistry play a crucial role in differentiating primary GI malignancies from metastasis.
Gastrointestinal hemorrhage, Lung neoplasm, Metastasis, Non-small cell carcinoma lung
Case Report
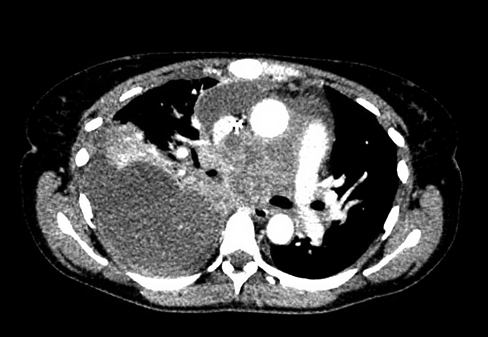
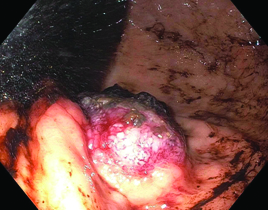
A 39-year-old female presented to the Emergency Department (ED) with complaints of dizziness and black tarry stools for one day. The patient had a significant smoking history (23 pack-year). Six weeks ago she was diagnosed with stage IV (T2N3M1) squamous cell carcinoma of the lung with extensive bone and lymph nodes metastases [Table/Fig-1]. The patient was started on a chemotherapy regimen of paclitaxel and carboplatin, along with denosumab and dexamethasone at the time of diagnosis. Her last chemotherapy session was held due to development of thrombocytopenia for which she had a platelet transfusion three days prior to ED arrival. On admission, initial workup revealed a haematocrit of 23.7%, hemoglobin of 7.9 gm/dL, and platelet count of 14,000/µl. She had a dark brown nasogastric tube output. Patient received two units of packed red blood cells and five units of platelets. At this point the gastroenterology team was consulted and they recommended an EGD to evaluate for upper G.I. bleed. Initial EGD revealed dark blood in the stomach with poor visualization of the fundus. No active bleeds were noticed and no source was identified. Patient continued to receive supportive care for the next two days with a continued drop in her hematocrit values. At that point a decision was made to perform a second EGD, which demonstrated a large ulcerated, friable mass measuring 6 cm × 6 cm in gastric fundus along with coffee-ground material in in the stomach [Table/Fig-2]. Biopsy samples were taken with cold forceps for histology. Oesophagus and duodenum appeared normal on endoscopic examination.
Contrast CT chest shows an extensive mass involving the right lower lobe with lymphadenopathy involving the mediastinum and hila along with a moderate pleural effusion.
Endoscopic imaging showing an ulcerated, friable mass in the gastric fundus.
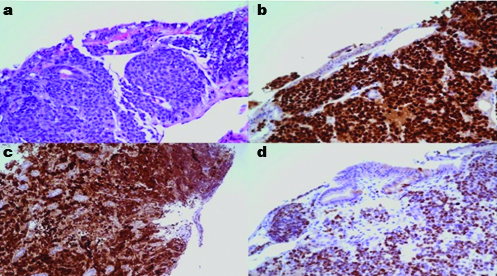
Histopathological examination revealed poorly-differentiated squamous cell carcinoma consistent with the patient’s known non-keratinizing squamous cell carcinoma of the lung [Table/Fig-3]. Immunohistochemical stains showed positive immunoreactivity for pan-keratin, p40, p63, and p16 and these findings were interpreted as metastasis from the patient’s primary lung SCC.
a) A biopsy revealed oxyntic type gastric mucosa showing extensive involvement by poorly differentiated carcinoma with the patient’s known poorly differentiated non- keratinizing squamous cell carcinoma testing positive for Immunohistochemical stains; b) p63; c) p16 and; d) p40.
Given the advanced disease of the patient, a decision was made to switch the patient’s chemotherapy to Nivolumab due to its lower risk of thrombocytopenia. Radiation therapy to the stomach was also recommended. Fifteen cycles of 250 centigray (cGy) were scheduled for a total dose of 3,750 cGy. She received 13 of the intended 15 fractions of radiotherapy, however continued to have progression of disease. Radiotherapy was held after her 13th session due to a significant decline in performance status. Patient subsequently died due to her widely metastatic lung cancer.
Discussion
Lung carcinoma is the leading cause of cancer death in the world and about 50% cases have distant metastasis at the time of diagnosis. Primary lung cancer frequently metastasizes to the nervous system (39%), bone (34%), liver (20%), respiratory system (18%), and adrenal gland (8%), while metastasis to gastrointestinal tract is rare [1]. The incidence of GI metastasis varies from 0.3%-1.77%. Autopsy studies generally have shown much higher incidence as compared to the clinical studies as most of the data comes from the autopsy studies with only rare symptomatic case reports being published [2-4]. Small bowel is the most common site for GI metastasis for all the histopathological types of primary lung cancer [5]. Lung cancer metastasis to the stomach is usually asymptomatic as it metastasizes mostly through hematogenous route in the submucosal plane. GI metastasis can clinically present with symptoms of upper abdominal pain (50%), anorexia (35%), anaemia (27%), nausea and vomiting (23%), occult blood and melena (23%) and hematemesis (19%) [6]. In the present case the patient presented with melena only. Therefore, GI symptoms in a known case of lung cancer should raise suspicion of an advanced metastatic disease.
There is no clear data on the metastatic patterns of the various histopathological types of lung cancer. Studies vary in their findings regarding the most common histopathological type of lung cancer metastasizing to the GI tract [7-9].
Diagnosis is usually established by using modalities like EGD, biopsy and imaging techniques like CT. Endoscopy in lung cancer is limited to those with suspicious symptoms. It is reasonable to speculate that routine endoscopy of all the lung cancer patients will lead to more frequent finding of metastasis to GI tract. This can lead to early diagnosis and accurate staging of the disease. Some studies have also explored the role of positron emission tomography in the diagnosis and management of these cases but it has not been well established [4,10]. Histopathological diagnosis with the use of immunohistochemical stains is the only reliable way to differentiate primary gastric malignancy from a metastatic gastric lesion coming from primary lung cancer [11]. TTF-1, p63, P40 and Napsin-A are the Immunohistochemical markers primarily used to differentiate lung SCC from lung adenocarcinoma [12,13]. These markers have been found to be particularly helpful in establishing histopathological diagnosis in complicated and poorly differentiated lung SCC cases or cases with limited tissue specimen availability [4,6,14,15]. In our case the IHC stain positivity for Pan-Keratin, p40, and p63 helped clinch the diagnosis as that of a metastatic lesion.
Upper GI bleeding in the setting of a metastatic lesion is generally diagnosed and treated by upper GI endoscopy or by surgical intervention. Endoscopic hemostasis can be achieved by using injection, bipolar or heater probe coagulation. Trans-catheter arterial embolization may be considered as a potential intervention to limit GI hemorrhage by selectively clotting the offending artery that feeds the tumor.
Radiotherapy (RT) is an effective modality to manage symptoms of pain and bleeding in patients with advanced primary gastric cancer who are not considered good candidates for palliative surgery or endoscopic procedures [16]. But there is no substantial evidence for the use of RT in gastric metastasis secondary to squamous cell carcinoma lung. RT may achieve hemostasis by inducing aggregation of platelets or by damage to the vascular endothelial cells [17].
Conclusion
In conclusion, initial staging of the primary lung SCC cancer remains an important decisive factor in determining management.
A regular upper GI endoscopy in these patients can lead to more accurate disease staging that can be detrimental in formulating an appropriate therapeutic plan. While IHC remains a critical diagnostic tool in differentiating primary gastric cancer from gastric metastasis we need to understand that the IHC result interpretation should be done in the context of the overall clinical scenario. Gastric metastasis predict a grim prognosis in most lung cancer patients. Palliative treatment remains as the primary recommendation in stage IV disease with multiple organ metastasis.
[1]. Riihimaki M, Hemminki A, Fallah M, Thomsen H, Sundquist K, Sundquist J, Metastatic sites and survival in lung cancerLung Cancer 2014 86(1):78-84. [Google Scholar]
[2]. Ryo H, Sakai H, Ikeda T, Hibino S, Goto I, Yoneda S, Gastrointestinal metastasis from lung cancerNihon Kyobu Shikkan Gakkai zasshi 1996 34(9):968-72. [Google Scholar]
[3]. Capasso L, Iarrobino G, R DA, Carfora E, Ventriglia R, Borsi E, Surgical complications for gastric and small bowel metastases due to primary lung carcinomaMinerva chirurgica 2004 59(4):397-403. [Google Scholar]
[4]. Rossi G, Marchioni A, Romagnani E, Bertolini F, Longo L, Cavazza A, Primary lung cancer presenting with gastrointestinal tract involvement: clinicopathologic and immunohistochemical features in a series of 18 consecutive casesJournal of Thoracic Oncology 2007 2(2):115-20. [Google Scholar]
[5]. Berger A, Cellier C, Daniel C, Kron C, Riquet M, Barbier JP, Small bowel metastases from primary carcinoma of the lung: clinical findings and outcomeThe American Journal of Gastroenterology 1999 94(7):1884-87. [Google Scholar]
[6]. Gao S, Hu XD, Wang SZ, Liu N, Zhao W, Yu QX, Gastric metastasis from small cell lung cancer: a case reportWorld Journal of Gastroenterology 2015 21(5):1684-88. [Google Scholar]
[7]. Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W, Gastrointestinal metastases from malignant tumors of the lungCancer 1982 49(1):170-72. [Google Scholar]
[8]. McNeill PM, Wagman LD, Neifeld JP, Small bowel metastases from primary carcinoma of the lungCancer 1987 59(8):1486-89. [Google Scholar]
[9]. Yamada H, Akahane T, Horiuchi A, Shimada R, Shibuya H, Hayama T, A case of lung squamous cell carcinoma with metastases to the duodenum and small intestineInternational Surgery 2011 96(2):176-81. [Google Scholar]
[10]. Yang CJ, Hwang JJ, Kang WY, Chong IW, Wang TH, Sheu CC, Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcomeLung Cancer 2006 54(3):319-23. [Google Scholar]
[11]. Gonzalez-Tallon AI, Vasquez-Guerrero J, Garcia-Mayor MA, Colonic metastases from lung carcinoma: a case report and review of the literatureGastroenterology Res 2013 6(1):29-33. [Google Scholar]
[12]. Nobre AR, Albergaria A, Schmitt F, p40: A p63 isoform useful for lung cancer diagnosis – a review of the physiological and pathological role of p63Acta Cytologica 2013 57(1):1-8. [Google Scholar]
[13]. Gurda GT, Zhang L, Wang Y, Chen L, Geddes S, Cho WC, Utility of five commonly used immunohistochemical markers TTF-1, Napsin A, CK7, CK5/6 and P63 in primary and metastatic adenocarcinoma and squamous cell carcinoma of the lung: a retrospective study of 246 fine needle aspiration casesClinical and Translational Medicine 2015 4:16 [Google Scholar]
[14]. Okazaki R, Ohtani H, Takeda K, Sumikawa T, Yamasaki A, Matsumoto S, Gastric metastasis by primary lung adenocarcinomaWorld Journal of Gastrointestinal Oncology 2010 2(10):395-98. [Google Scholar]
[15]. Brunnström H, Johansson L, Jirström K, Jönsson M, Jönsson P, Planck M, Immunohistochemistry in the differential diagnostics of primary lung cancer. An Investigation Within the Southern Swedish Lung Cancer StudyAm J Clin Pathol 2013 140(1):37-46. [Google Scholar]
[16]. Kondoh C, Shitara K, Nomura M, Takahari D, Ura T, Tachibana H, Efficacy of palliative radiotherapy for gastric bleeding in patients with unresectable advanced gastric cancer: a retrospective cohort studyBMC Palliative Care 2015 14:37 [Google Scholar]
[17]. Rosenberg RD, Aird WC, Vascular-bed-specific hemostasis and hypercoagulable statesThe New England Journal of Medicine 1999 340(20):1555-64. [Google Scholar]