Idiopathic Granulomatous Mastitis: A Clinical Puzzle in Breast Lump Cases
Vivek G Nath1, Rakesh sahoo2, Avinash sahoo3, Jithendra kumar Barad4, K A Arun5
1 Junior Resident, Department of General Surgery, SCB, Medical College, Cuttack, Odisha, India.
2 Senior Resident, Department of General Surgery, SCB, Medical College, Cuttack, Odisha, India.
3 Junior Resident, Department of General Surgery, SCB, Medical College, Cuttack, Odisha, India.
4 Junior Resident, Department of General Surgery, SCB, Medical College, Cuttack, Odisha, India.
5 Junior Resident, Department of General Surgery, SCB, Medical College, Cuttack, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vivek G Nath, Flat no-4c Gajaraj Apartments 11-b Cantonment Road, Cuttack-753001, Odisha, India.
E-mail: drvivekgnath@gmail.com
Idiopathic granulomatous mastitis (IGM) is a rare benign disease, characterized by chronic inflammation and granulomatous disease process. A middle aged lady with breast lump for six months with equivocal mammographic and ultrasound results underwent lumpectomy and biopsy. Ruling out all other possible granulomatous diseases and malignancy, a diagnosis of IGM was made. IGM becomes clinically significant as it closely mimics carcinoma breast and some inflammatory and infectious pathology.
Benign tumour, Breast, Granulomatous disease, Hyperprolactinemia
Case Report
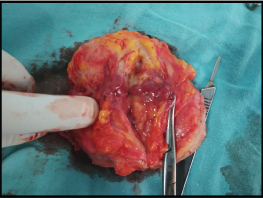
A 37-year-old lady presented with a painless lump in the right breast for duration of six months [Table/Fig-1]. Swelling was insidious in onset and gradually progressed over a period of six months. There was associated serous nipple discharge during the initial period which subsided later. There was no associated history of pain, fever, rapid change in lump size, weight loss, decreased appetite, night sweats, cough, haemoptysis, chest pain, low backache, pain abdomen or jaundice. There was no other history of medical or surgical treatment, substance abuse, OCP use or psychiatric medication. There was no similar illness in the past or history of malignancy in first and second degree relatives. Menstrual and marital history were normal. On physical examination, a swelling of size 8 × 5 cm was found in the upper outer quadrant of right breast with a nipple deviation downwards without retraction [Table/Fig-1]. Skin over the swelling and nipple areola complex were normal. Swelling was mobile with the breast tissue; without any chest wall or skin fixity. The margins were ill defined, surface was smooth, firm in consistency with central fluctuation and was non tender. Both axilla and contra lateral breast were normal. Abdominal examination revealed a non tender, soft abdomen without organomegaly or free fluid. General examination and systemic examinations were within normal limits.
Clinical photograph of breast lump and nipple deviation (right side).

Routine blood investigations, Liver Function Test (LFT) and C-reactive Protiene (CRP) were within normal limits. USG showed heterogeneous ill defined area in the upper outer quadrant of right breast within normal axilla. Mammography reported BIRADS-4, showing asymmetric mass with increased radio density and slight nipple retraction. Chest x -ray did not reveal any lung lesions. A core biopsy was performed which was reported as non specific inflammatory mass without signs of malignancy. Culture was negative for bacteria, fungus and mycobacterium.
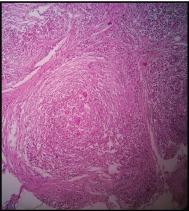
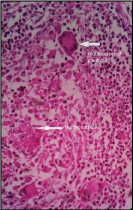
Patient was managed with a course of oral antibiotics suspecting inflammatory pathology; with carcinoma as a differential diagnosis. After a week of antibiotics, patient was subjected for a lumpectomy under general anaesthesia. Gross specimen examination showed an ill defined lump of size approximately 8 × 6 cm with central necrosis and purulent exudates [Table/Fig-2]. Histopathological examination revealed features of granulomatous process with multi nucleated giant cells, epitheloid cells and macrophages; neither evidence of malignancy nor any specific organism was found [Table/Fig-3,4]. Absence of caseous necrosis was marked in the granuloma which was surrounded by micro abscesses. TB-PCR was done which ruled out the possibility of tuberculosis. Anti-nuclear Antibody (ANA) profile was done with negative results. A diagnosis of idiopathic granulomatous mastitis was made by exclusion. Wound healing was normal and patient was discharge on seventh postoperative day. Monthly physical examination was scheduled and there were no signs of recurrence over six months follow up.
Cut section of gross specimen showing necrotic material.
Microscopic picture of granuloma in low power, stained with H&E showing absent central caseation in IGM.
High power (40X) picture showing giant cells and epitheloid cells in IGM (H&E stain).
Discussion
IGM is an extremely rare clinical scenario characterized by chronic inflammation and features of granulomatous disease process. It was first described by Kessler E and Wolloch Y in 1972 [1].
Clinically IGM presents in different forms. It can present as unilateral or bilateral breast mass with or without tenderness, nipple retraction, nipple discharge (serous/bloody), inflammatory skin changes (ulcerations/sinus formation or puckering) and rarely as axillary lymphadenopathy [2,3].
Imaging studies like mammogram and USG will give features closely mimicking a malignant lesion. Definitive diagnosis is made by histopathological examination and demonstration of granuloma formation without any evidence of infection. A mixed chronic inflammatory process containing lymphocytes, plasma cells, epitheloid histiocytes, multinucleated giant cells, and neutrophil infiltration with micro abscess can be found in the granuloma. IGM has become a clinical puzzle as it closely mimics malignancy [9] clinically and a definitive diagnosis can only be established by exclusion of wide spectrum of granulomatous diseases like sarcoidosis, Wegener’s granulomatosis [4], giant cell arteritis, polyarteritis nodosa, tuberculosis, syphilis, corynebacterial infection, cat-scratch disease etc., [5]. Other possibilities include fungal infections, duct ectasia, granulomatous reaction of carcinoma and foreign body granuloma. Sarcoidosis and Wegener’s granulomatosis are systemic diseases with multi organ involvement. Sarcoidosis affects mainly lung and associated lymph nodes, rarely may affect breast also. Wegener’s diseases are a large vessel vasculites that affect upper airway, lungs and kidney [5]. Polyarteritis nodosa and giant cell arterites are medium vessel arterites almost never affecting the breast. Granulomatous response to carcinoma is rare and is restricted in the peripheral stroma, charecterised by multinucleated giant cells [5]. Hence, exclusion of systemic involvement of the common granulomatous diseases along with histological evidences of granulomatous diseases is needed to arrive at a diagnosis of IGM [5,6].
Reported causes of IGM include OCP use, pregnancy, lactation, α-1 antitrypsin deficiency, hyperprolactinemia. A case of IGM due to risperidone induced hyperprolactinemia was reported recently [5]. It has been postulated that IGM results from a localized autoimmune response to the retained or extravasated fat- or protein-rich secretion in the breast ducts during childbearing age due to a previous hyperprolactinemia [7]. To differentiate from TB mastitis, demonstration of granuloma without caseation necrosis and absence of acid fast bacilli in culture may be helpful. Confirmation is attained by performing Polymerase Chain Reaction (PCR) for tubercular bacilli.
Mammogram usually gives features like asymmetric density or ill defined mass mimicking carcinoma. Ultrasound may reveal areas of mixed echogenicity, single/multiple irregular hypoechoic masses [8]. Wide excision is considered as the mainstay of treatment. Delayed healing, ulceration, fistula formation etc may complicate the procedure. Some centres give a course of Anti-tubercular Therapy(ATT) after excision; steroids are used in non responding and recurrent lesions [9].
Conclusion
IGM is an extremely important clinical entity which need focused assessment and management as it may closely mimic carcinoma and wide range of infectious and inflammatory processes. Surgeons, with the help of pathologist and radiologist can diagnose and treat this. Further studies are required to establish the aetiological and pathological factors, relation with lactation and prolactin levels with the development of this disease.
[1]. Kessler E, Wolloch Y, Granulomatous mastitis: a lesion clinically simulating carcinomaAm J Clin Pathol 1972 58(6):642-46. [Google Scholar]
[2]. Fletcher A, Magrath IM, Riddell RH, Talbot IC, Granulomatous mastitis;a report of seven casesJ Clin Pathol 1982 35(9):941-45. [Google Scholar]
[3]. Azlina AF, Ariza Z, Arni T, Hisham AN, Chronic granulomatous mastitis: diagnostic and therapeutic considerationsWorld J Surg 2003 27:515-18. [Google Scholar]
[4]. Veerysami M, Freeth M, Carmichael AM, Wegener’s granulomatosis of the breastBreast J 2006 12:268-70. [Google Scholar]
[5]. Lin CH, Hsu CW, Tsao TY, Chou J, Idiopathic granulomatous mastitis associated with risperidone-induced hyperprolactinemiaDiagnostic Pathology 2012 7:2 [Google Scholar]
[6]. Ergin AB, Cristofanilli M, Daw H, Tahan G, Gong Y, Recurrent granulomatous mastitis mimicking inflammatory breast cancerBMJ case reports 2011 2011:bcr0720103156 [Google Scholar]
[7]. Cserni G, Szajki K, Granulomatous lobular mastitis following drug-induced galactorrhea and blunt traumaBreast J 1999 5(6):398-403. [Google Scholar]
[8]. Lee JH, Oh KK, Kim E, Kwack KS, Jung WH, Lee HK, Radiologic and clinical features of idiopathic granulomatous lobular mastitis mimicking advanced breast cancerYonsei Med J 2006 47:78-84. [Google Scholar]
[9]. Kuba S, Yamaguchi J, Ohtani H, Shimokawa I, Maeda S, Kanematsu T, Vacuum-assisted biopsy and steroid therapy for granulomatous lobular mastitis: report of three casesSurg Today 2009 39:695-99. [Google Scholar]