Case 1
A 68-year-old, postmenopausal woman was referred to plastic surgery department from the department of obstetrics and gynaecology with complaint of swelling in the right labial region present approximately over the last two years. It was small and painless, gradually increasing in size. More rapid increase in size was observed over the last three months.
On clinical examination, there was a solitary swelling situated in the right labium majus extending from the level of pubic bones down to just above the vulval fourchette inferiorly. A swelling of size 10 x 7 x 3 cm was noted, which was a soft but tense swelling with a smooth surface with no tenderness or local warmth. It was subcutaneous, extending deep into tissue planes. Fluctuation was present. Transillumination was negative. No enlargement of regional lymph nodes. A clinical diagnosis of Bartholin gland cyst was made and planned for surgical excision.
Under spinal anaesthesia, with patient in lithotomy position and a urethral foley’s catheter in situ, an elliptical vertical incision was made and the skin flaps were reflected. The large cystic swelling was exposed and separated by blunt and sharp dissection on all sides and completely excised. There was nearly 500 ml of thick straw coloured fluid in the cyst. The resultant defect in the right vulvar region was repaired in two layers.
The excised tissue was sent for histopathological examination. Cut section of the tissue showed uniloculated cyst with a smooth inner surface which was greyish brown in colour. Microscopic examination showed the cyst lined by cuboidal to columnar epithelium and the cyst wall showed chronic inflammatory cell collections. Suggestive of infected Bartholin cyst with haemorrhage.
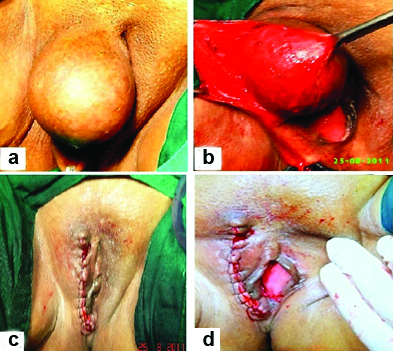
Postoperative period was uneventful and the patient recovered fast and was discharged on seventh postoperative day after removing the sutures. She was comfortable and doing well when she came for check up after three weeks. There was no report of recurrence over the last five years [Table/Fig-1].
a) Preoperative; b) Peroperative; c) After excision of the cyst; d) Post-operative.
Case 2
A 42-year-old woman came with chief complaint of large swelling near the introitus on the right side since one and half years which grew suddenly over the last six days to the present size. Patient gave a history of fever five days prior, which was associated with chills and rigors. She was a known diabetic since one year and was on medication. There was no history of any trauma, weight loss or loss of appetite.
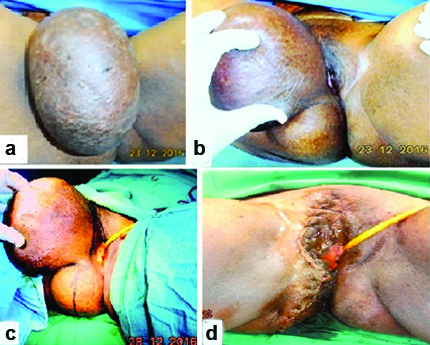
On examination, there were two masses one at right labia majora (23 x 11 cm) and one just below it at the right gluteal region (6 x 6 cm). Both the swellings were cystic in consistency with cross fluctuation present between the two. Transillumination was negative and getting above the swelling was absent. Per speculum and bimanual examination were normal [Table/Fig-2].
a) Preoperative; b) Showing dumb-bell appearance; c) Peroperative; d) Postoperative.
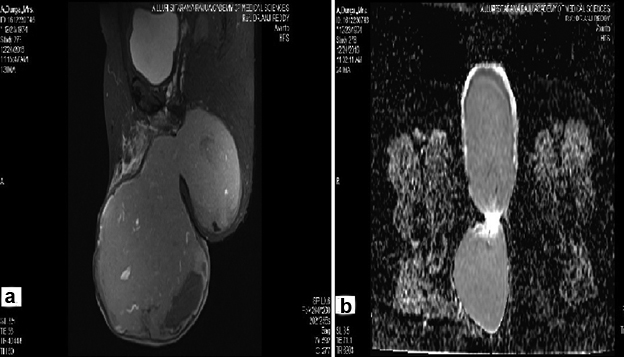
MRI pelvis was done and the report showed evidence of very large thick walled (6 mm) bilobed heterogenous cyst, arising from the right vulval region below the level of pubic symphysis, anterior lobe-14.2 x 10.6 x 13.5 cm; posterior lobe 7.3 x 7.6 x 8.3 cm extending postero-infero-medially upto proximal one third of right thigh [Table/Fig-3].
a) MRI of the cyst b) MRI showing dumb-bell appearance.
Patient was taken up for surgery. A vertical elliptical incision was made around the base of the cyst 1 inch away from labia and 2 inches away from anal opening. Cyst with false capsule was dissected and separated by blunt and sharp dissection on all sides. The labial cyst was excised and found to be having dark stained thick fluid; the gluteal cyst was also isolated and separated and removed in toto. Levator muscles repaired and skin was closed with 4-0 Prolene [Table/Fig-4a,b]. The excised cyst along with its extension was sent to the department of pathology for histopathological examination.
a) Peroperative image showing cyst separation; b) Gross specimen; c) Photomicrograph (H&E, X 40) cyst lined by squamous epitlelium with inflammatory cells in the wall; d) Postoperative.
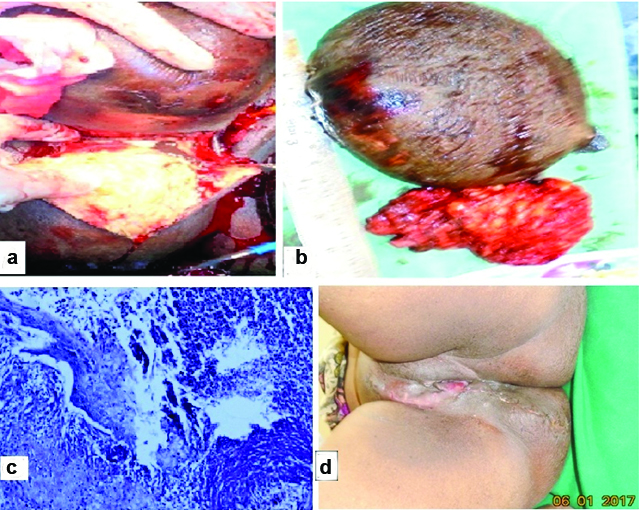
On gross examination, larger specimen of size 23 x 11 x 9 cm weighing 1500 gm: wrinkled skin with altered blood with a wall thickness of 1.5 cm; and also a smaller specimen which was a fibrofatty mass partly covered by skin of 9 x 7 x 5 cm.
Microscopic examination showed stratified squamous epithelium with underlying cyst and cyst wall showed extensive denudation of serosa. The wall was thickened and infiltrated by predominantly acute inflammatory cells. Areas of haemorrhage and congested blood vessels were also noted [Table/Fig-4c].
During the postoperative period patient was put on antibiotic coverage and suture removal was done on seventh postoperative day. Wound healed well and was discharged with satisfactory result [Table/Fig-4d].
Discussion
Bartholin’s glands, the female counterpart of the Cowpers glands in the male, are compound racemose glands lined by columnar epithelium. Each gland measures about 0.5 cm, with a 2 cm duct, opening into the vestibule, in the groove between hymen and labia minora at 5’O and 7’O clock position. Their function is to secrete alkaline mucous for lubrication during sexual stimulation [1].
The most common types of Bartholin gland masses are cysts or abscesses [2]. Bartholin gland cysts develop from dilatation of the duct following blockage of the duct opening. An obstructed Bartholin duct can become infected and form an abscess. Abscesses are three times more common than cysts [2,3]. Women in the reproductive age group are likely to develop Bartholin abscess. Abscesses appear most likely in women at risk for sexually transmitted infections [4]. The infection is usually polymicrobial, with bacteroides and Escherichia coli being predominant organisms [5,6].
Bartholin cysts usually do not cause any symptoms, but abscesses can present with severe pain and can cause discomfort, typically during ambulation, sitting or sexual intercourse (dyspareunia). Fever may or may not be an associated feature [7]. On examination it appears as a warm, tender, soft, fluctuant mass in lower medial labia majora and may occasionally be surrounded by erythema and oedema. Large abscesses may expand into the upper labia. Other conditions that may mimic Bartholin’s abscess include hidradenitis suppurativa, lipomas, epidermoid cysts and Skene’s duct cysts [8,9]. The key to identify a Bartholin mass is the anatomic location of the mass [10].
In addition to physical examination, high definition ultrasound and MRI is helpful in aiding a diagnosis [11-13].
The initial treatment is incision and drainage with placement of Word catheter [14]. Immediate pain relief occurs upon drainage of pus. The catheter is left inside for 4-6 weeks for epithelization. Similarly, the Jacobi ring can also be used for drainage and re-epithelization of the cysts. In a randomized study on treatment of Bartholin cysts, outcomes using Jacobi rings and word catheter were comparable, but rings have a greater patient satisfaction. In the same study, 4%-17% presented with recurrence after using catheter insitu, and often there were cases of premature dislodgment of the catheter before the tract is epithelialized [15]. For deep cysts and abscesses, this treatment is not advisable [16]. However, antibiotics are not given routinely, because more than 80% of cultures from Bartholin’s cysts and about 33% of cultures from Bartholin’s abscesses are sterile.
Another common method of treatment for Bartholin glands cysts is marsupialization where a small 1.5 cm to 3 cm incision is given over the cyst allowing drainage of the secretions [17]. But in the presence of an abscess, marsupialization should not be performed. In a randomized prospective study, out of 83 women submitted to marsupialization, the most frequent postoperative symptoms were discharge at the surgical site and labial oedema and also 24.1% presented with recurrence, 68.7% had scar formation [18].
Other methods of treating Bartholin gland cysts or absceses include silver nitrate application, CO2 laser vaporization, and needle aspiration with or without alcohol sclerotherapy and gland excision.
In randomized prospective study comparing marsupialization and silver nitrate application in management of Bartholin cyst and abscesses, both seem to be equally effective, however, with silver nitrate, complete healing with less scar formation was observed [18].
In a study in 2012 on management of Bartholin cysts with CO2 laser vapourization, out of 127 patients, only 86.6% cured after a single laser treatment. The mean cyst size in the study was ranging from 1.5 cm to 5.0 cm [19]. However, management of bigger size cysts with CO2 laser ablation has not been mentioned in literature.
In a systematic review in 2009, authors concluded that all of the available treatments were associated with lesser recurrence rates, faster healing, and few adverse events. However, best treatment approach for these bigger size cysts could not be identified according to the current literature [20].
Although giant Bartholin’s cyst is reported in several case reports, dumb-bell shaped presentation has not been reported in literature. In our cases marsupulization, CO2 laser ablation, sclerotherapy are not feasible because of the bigger size of the cysts. So we managed the cases with excision and pelvic floor repair with subsequent good outcome in both the cases. Thus, excision of the entire Bartholin gland and duct is the definitive procedure of treatment for these cases.
Conclusion
Though Bartholin’s cyst abscess presents as a vulval mass, a dumb-bell shaped presentation or as a giant cyst, as in our cases are very rare. Management modality of these may be altered from that of a normal presentation according to the amount of discomfort it causes to the patient and size and extent of the mass. Though physical examination and MRI help in making a diagnosis, biopsy is confirmatory. Surgical management with complete cyst excision under antibiotic coverage is the definitive treatment.
[1]. Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM, Williams Gynaecology 2016 :280 [Google Scholar]
[2]. Antvorskov JC, Josefsen K, Engkilde K, Funda DP, Buschard K, Dietary gluten and the development of type 1 diabetesDiabetologia 2014 75:1770-80. [Google Scholar]
[3]. Omole F, Simmons BJ, Hacker Y, Management of Bartholin’s duct cyst and gland abscessAm Fam Physician 2003 68:135-40. [Google Scholar]
[4]. Aghajanian A, Bernstein L, Grimes DA, Bartholin’s duct abscess and cyst: A Case-Control studySouth Med J 1994 87(1):26 [Google Scholar]
[5]. Brook I, Aerobic and anaerobic microbiology of Bartholin’s AbscessSurg Gynaecol Obstet 1989 169(1):32 [Google Scholar]
[6]. Tanaka K, Mikamo H, Ninomiya M, Tamaya T, Izumi K, Ito K, Microbiology of bartholin’s gland abscess in JapanJ Clini Microbiol 2005 43(8):4258 [Google Scholar]
[7]. Kessous R, Aricha-Tamir B, Sheizaf B, Steiner N, Moran-Gilad J, Weintraub AY, Clinical and Microbiological characteristics of Bartholin’s gland abscessesObst Gyn 2013 122(4):794 [Google Scholar]
[8]. Koenig C, Tavassoli FA, Nodular hyperplasia, adenoma, and adenomyoma of Bartholin’s glandInt J Gynecol Pathol 1998 17:289-94. [Google Scholar]
[9]. Kessous R, Aricha-Tamir B, Sheizaf B, Steiner N, Moran-Gilad J, Weintraub AY, Clinical and microbiological characteristics of Bartholin gland abscessesObstet Gynecol 2013 122:794-99. [Google Scholar]
[10]. Sosnik H, Sosnik K, Halon A, The pathomorphology of Bartholin’s gland. Analysis of surgical dataPol J Pathol 2007 58:99-103. [Google Scholar]
[11]. Kozawa E, Irisawa M, Heshiki A, Kimura F, Shimizu Y, MR findings of a giant Bartholin’s duct cystMagn Reson Med Sci 2008 7:101-03. [Google Scholar]
[12]. Berger MB, Betschart C, Khandwala N, De-Lancey JO, Haefner HK, Incidental bartholin gland cysts identified on pelvic magnetic resonance imagingObstet Gynecol 2012 120:798-802. [Google Scholar]
[13]. Eppel W, Frigo P, Worda C, Bettelheim D, Ultrasound imaging of Bartholin’s cystsGynecol Obstet Invest 2000 49:179-82. [Google Scholar]
[14]. Marzano DA, Haefner HK, The Bartholin’s gland cyst: Past, Present and FutureJ Low Genital Tract Disease 2004 8(3):195 [Google Scholar]
[15]. Gennis P, Li SF, Provataris J, Randomized pilot study comparing a rubber ring catheter to the word catheter in the treatment of Bartholin abscessesAcad Emerg Med 2004 11(5):527 [Google Scholar]
[16]. Koc O, Sengul N, Gurel S, Perineal leiomyoma mimicking complex Bartholin massInt Urogynecol J 2010 21:495-97. [Google Scholar]
[17]. Bora SA, Condous G, Bartholin’s, vulval and perineal abscessesBest Pract Res clin Obste Gynaecol 2009 23(5):661-66. [Google Scholar]
[18]. Ozdegirmenci O, Kayikcioglu F, Haberal A, Prospective randomized study of marsupilization versus silver nitrate application in the management of bartholin gland cysts and abscessesJ inim Invasive Gynaecology 2009 16(2):149-52. [Google Scholar]
[19]. Figueiredo ACN, Folgado da Silva PA, Duarte AR, Gomes TPM, Borrego LMP, Marques CAC, Bartholin’s gland cysts: management with carbon-dioxide laser vaporizationRev Bras Ginecol Obstet 2012 34(12):550-54. [Google Scholar]
[20]. Wechter ME, Wu JM, Marzano D, Haefner H, Management of Bartholin duct cysts and abscesses: a systematic reviewObstet Gynecol Surv 2009 64:395-404. [Google Scholar]