Pneumatosis Cystoides Intestinalis
Vamsidhar Rachapalli1, Sreedhara B Chaluvashetty2
1 Consultant Interventional Radiologist, Department of Radiology, BGS Global Hospital, Bengaluru, Karnataka, India.
2 Consultant Radiologist, Department of Radiology, BGS Global Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vamsidhar Rachapalli, Consultant Interventional Radiologist, Department of Radiology, BGS Global Hospital No 67, Uttarahalli Main Road, Kengeri-560078, Bengaluru, Karnataka, India.
E-mail: r_vamsidhar@yahoo.com
Bowel, Mural cysts, Pneumoperitoneum
Presence of free air in the peritoneal cavity is considered as a medical emergency, usually necessitating urgent surgical intervention. It is important to recognize the cause of pneumoperitoneum and then appropriately manage the patient.
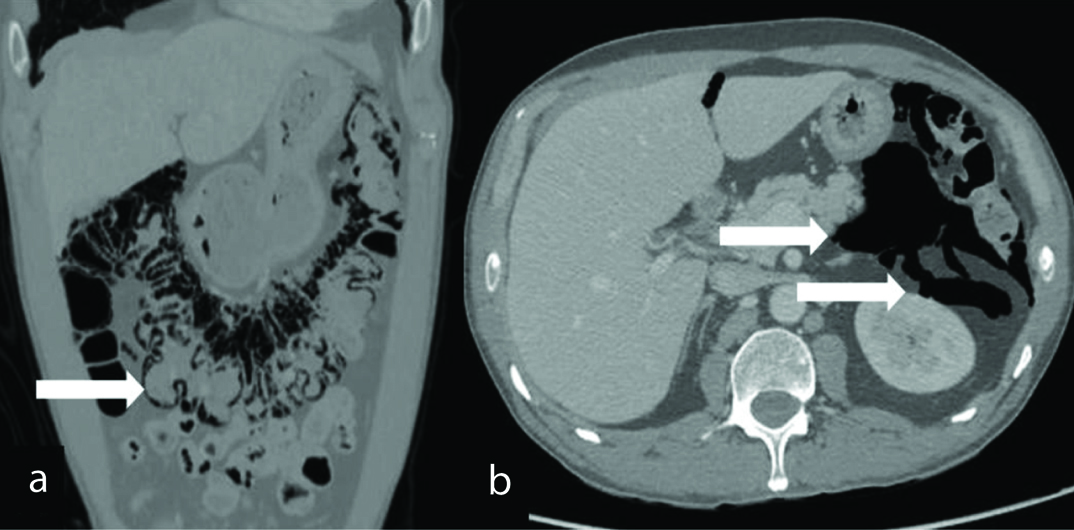
A 50-year-old male patient with a past medical history of Burkitts lymphoma and post allogeneic bone marrow transplant, which was done one year back; was referred for management of dyspnea secondary to Graft Versus Host Disease (GVHD) of gut and lung, which developed nine months post transplant. He was undergoing treatment for GVHD. In view of his respiratory symptoms a computerized tomography of the chest was undertaken, which showed free air in the abdomen. Subsequent Computerized Tomography (CT) of the abdomen and pelvis showed diffuse intramural air within the transverse colon [Table/Fig-1a,arrow] with extensive free intraperitoneal and retroperitoneal air foci [Table/Fig-1b,arrow]. No abnormal bowel wall thickening, free fluid or signs of mesenteric ischemia were noted. The main differentials for these radiological findings are bowel perforation or pneumatosis cystoides intestinalis. However, given that the patient did not have any abdominal symptoms or demonstrate signs of peritonism, a diagnosis of Pneumatosis Cystoides Intestinalis (PCI) was made. He was managed conservatively and was subsequently discharged in a stable condition.
a) Coronal reconstruction; b) Axial image-of a computerized tomography of the abdomen and pelvis, which demonstrates intramural air in the walls of the transverse colon [Table/Fig-1a,arrow] and free retroperitoneal and intraperitoneal air [Table/Fig-1b,arrows].
PCI is an uncommon condition characterized by gas in the bowel wall. The gaseous cysts contain hydrogen, nitrogen and carbon dioxide are located in the subserosal and submucosal layers of the bowel [1,2]. It was first described by Du Vernoy in 1730, but was named by Mayer almost 100 years later [2]. It occurs in 0.03% of the population with a male to female ratio ranging from 3-3.5:1 [2,3]. It can be iatrogenic in origin or occur in immunocompromised patients, those who had previous chemotherapy or suffer with chronic respiratory pathology [1]. It is known to occur in patients with GVHD [4]. In patients with GVHD, it occurs approximately two to eight months after the bone marrow transplant. However, cases have been reported as late as 24 months post transplantation [4]. In our case PCI developed nine months post transplant. Multiple theories have been postulated to account for PCI. The mechanical theory works on the basis that there is injury to the bowel wall or there is increased intraluminal pressure that leads to PCI. In patient with pulmonary diseases like asthma, chronic pulmonary disease, it is proposed that the pulmonary alveolar rupture leads to a pneumomediastinum. The gas travels along the aorta and the mesenteric vessels into the bowel wall (pulmonary theory). The bacterial theory states that the gas-forming bacteria breech the mucosal barrier through rents or increased permeability and produce the gas within the bowel wall. In the chemical theory or nutritional deficiency theory, malnutrition can prevent the digestion of carbohydrates, leading to increased bacterial fermentation, thus leading to production of large volumes of gas leading to distention eventually leading to submucosal dissection of gas [2]. However, none of these theories completely explain all the pathological process concerning all the aetiologies [2].
Patients are generally asymptomatic. When symptomatic, it shows clinical picture with nausea, vomiting, diarrhea and abdominal pain [5]. CT is helpful in finding additional signs reflecting the severity of the pathology which include linear appearance of gas pockets, presence of portal venous gas, bowel wall thickening, absent or intense abnormal mucosal enhancement, bowel dilatation, vascular occlusion, ascites [6]. Therefore, CT appears to be sensitive imaging modality in diagnosis of PCI.
Appropriate therapy depends on the aetiology of PCI. Over 90% cases can be managed without any treatment [2]. Medical management includes high flow oxygen, hyperbaric therapy, parenteral nutrition and antibiotics. Surgery is reserved for those with complications like volvulus or intra-abdominal haemorrhage occurs or to manage the primary condition causing the PCI like bowel obstruction or ischemia or if medical management fails [2,5]. Patients should be carefully monitored to identify any adverse signs and symptoms. In conclusion, pneumatosis interstitialis cystoides is a rare disorder that is poorly understood and along with chronic graft-versus-host disease it presents a heterogeneous clinical picture that does not correlate with results of imaging. Therefore, CT is a method of choice to diagnose PCI.
[1]. Azzaroli F, Turco L, Ceroni L, Galloni SS, Buonfiglioli F, Calvanese C, Pneumatosis cystoides intestinalisWorld J Gastroenterol 2011 17(44):4932-36. [Google Scholar]
[2]. Wu LL, Yang YS, Dou Y, Liu QS, A systematic analysis of pneumatosis cystoides intestinalisWorld J Gastroenterol 2013 19(30):4973-78. [Google Scholar]
[3]. Rathi C, Pipaliya N, Poddar P, Pandey V, Ingle M, Sawant P, A rare case of hypermobile mesentery with segmental small bowel pneumatosis cystoides intestinalisIntest Res 2015 13(4):346-49. [Google Scholar]
[4]. Laskowska K, Burzynska-Makuch M, Krenska A, Kołtan S, Chrupek M, Nawrocka E, Pneumatosis cystoides interstitialis: A complication of graft-versus-host disease. A report of two casesPol J Radiol 2012 77(2):60-63. [Google Scholar]
[5]. Ooi SM, Pneumoperitoneum in a non-acute abdomen-pneumatosis cystoides intestinalisSurg Case Rep 2015 1(1):44 [Google Scholar]
[6]. Olson DE, Kim YW, Ying J, Donnelly LF, Predictors for differentiating benign and clinical worrisome pneumatosis instestinalis beyond the neonatal periodRadiology 2009 253(2):513-19. [Google Scholar]