Idiopathic Brachial Neuritis in a Patient with Multiple Myeloma
Lale Cerrahoglu1, Ozlem Erol2, Tuba Cerrahoglu Sirin3
1 Department of Physical Medicine and Rehabilitation, School of Medicine, Celal Bayar University, Manisa, Turkey.
2 Department of Physical Medicine and Rehabilitation, School of Medicine, Celal Bayar University, Manisa, Turkey.
3 Department of Neurology, Sisli Hamidiye Etfal Education and Research Hospital, Istanbul, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tuba Cerrahoglu Sirin, Department of Neurology, Agri State Hospital, Agri, Turkey.
E-mail: tubacerrahoglu@hotmail.com
Idiopathic Brachial Neuritis (IBN), is a rare brachial plexopathy with an unknown aetiology. Multiple myeloma is a neoplastic plasma cell disease characterised by bone lesions. In this article, we present the case of a 59-year-old male patient with IBN associated with multiple myeloma, who was admitted to our clinic with right shoulder pain and right arm weakness. He experienced muscle weakness and atrophy in his right arm after a sudden onset of pain attack in the shoulder. Plexus and cervical vertebral MRI showed no pathology. Electrodiagnostic studies showed upper and middle trunk plexopathies. Laboratory analysis revealed anaemia, hypercalcaemia, renal dysfunction and monoclonal gammopathy in immunoglobulin electrophoresis. A bone marrow biopsy established the diagnosis of IgG kappa multiple myeloma. This is the first case report that presents the association of multiple myeloma and IBN.
Hypercalcaemia, Immunoglobulin IgG, Neuralgic amyotrophy
Case Report
A 59-year-old male patient presented with complaints of pain, weakness and limitation of movement in his right shoulder for the past year. The pain started with a sudden sharp burning character spreading to the patient’s shoulder and neck one year ago. Approximately one month later, pain lost its sharp burning character; but, it continued as localized shoulder pain. The patient was experiencing difficulty in lifting his arms. Within the month, while severity of pain was decreasing; it got more difficult for the patient to lift his arms. There was no previous history of trauma, chronic disease, infection, vaccination, neurotoxicity, radiation therapy, use of chronic medication and surgery.
The patient appeared cachectic with a weight loss of about 7 kilos in the last three months. Passive right shoulder movements were normal but painful. Right shoulder muscles were atrophic. Abduction and flexion of right shoulder; flexion and extension of right elbow muscle was weak (1/5 and 3/5 according to muscle strength grading scale, respectively). Right biceps and brachioradial reflexes were hypoactive.
Laboratory studies revealed anaemia, hypercalcaemia and renal failure [Table/Fig-1]. Upon detecting high globulins in the patient’s analyses, we carried out further investigations, which revealed monoclonal gammopathy in immunoglobulin electrophoresis, and CD138, MUM1, IgG and kappa paint in 80-90% of the plasma cells in bone marrow biopsy, which lead us to the diagnosis of Multiple Myeloma.
Laboratory findings of the patient.
| Biochemistry parameters | Laboratory findings | Reference |
|---|
| Haemoglobin | ↓6.6 g/dl | 13.6-17.2 g/dl |
| Haematocrit | ↓19.7% | 39.5-50.3% |
| Leukocyte | 10000/mm3 | 4500-10300/mm3 |
| Thrombocytes | 219000/mm3 | 150000-400000/mm3 |
| Creatinine | ↑2.5mg/dl | 0.7-1.3 mg/dl |
| Calcium | ↑12.2 mg/dl | 8.3-10.6 mg/dl |
| Total protein | ↑13.3 g/dl | 6.4-8.7 g/dl |
| Albumin | 2.5 g/dl | 3.2-4.8 g/dl |
| Sedimentation | ↑>140 mm/h | 0-20 mm/h |
| C-reactive protein | ↑16.4 mg/l | 0-5 mg/l |
| Glomerular filtration rate | ↑25.42 | >60 |
| β-2 microglobulin | ↑14098 μg/l | 609-2366 μg/l |
| IgG | ↑2310 mg/dl | 700-1600 |
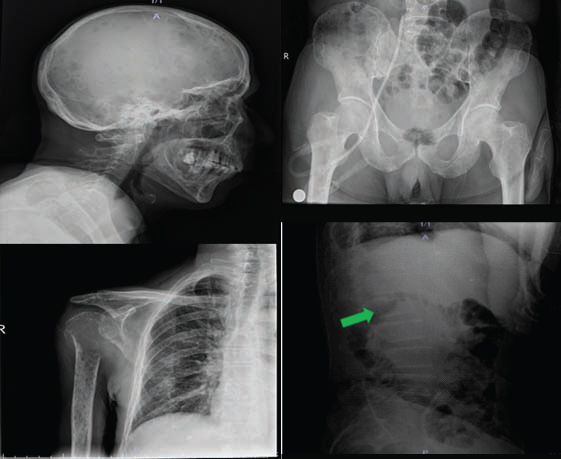
The right shoulder radiographs indicated expansive lytic lesion that destructed right proximal humerus. In addition, the bone survey showed multiple lytic lesions in skull, scapula, left humerus and pelvis [Table/Fig-2]. The MRI of the shoulder showed generalised oedema in rotator cuff and secondary tears to the lytic lesion in tendon attachment sites of the supraspinatus/infraspinatus muscles. The brachial plexus MRI and cervical MRI showed no pathological findings.
Radiographs of the skull, pelvis and right humerus demonstrates nu-merous lytic lesions. Lateral radiograph of the lumbar spine (Arrow) shows deformity of the L1 vertebral body due to compression fracture.
Electroneuromyography detected upper and middle trunks brachial plexopathy with chronic neurogenic Motor Unit Action Potential (MUAP) changes in supraspinatus and infraspinatus muscles in addition to the partial chronic neurogenic MUAP changes in biceps brachi and triceps muscles [Table/Fig-3].
Electrodiagnostic nerve conduction study results of the patient.
| Right | Left | Nerve | Nerve Conduction velocity (m/sn) | Distal latency (ms) | Sensory nerve action potential (μν) | Compound muscle action potential (mV) |
|---|
| X | | N.medianus | 36 ↓ | 2,5 | 14 ↓ | |
| X | | N.ulnaris | 52 | 2,7 | 22 | |
| X | | N.lateral antebrachial cutaneous | 38 ↓ | 2,8 ↑ | 8 ↓ | |
| X | | N.medianus | 53 | 3,2 | | 7 |
| X | | N.ulnaris | 56 | 2,9 | | 8 |
| X | | N.radialis | 60 | | | 10 |
| X | | N. musculocutaneus (Erb’s-m.biceps) | | 5,5 ↑ | | 4 ↓ |
| X | | N. radialis (Erb’s-m. triceps) | | 4,0 | | 7,5 |
| X | | N.axillaris (Erb’s-m. deltoid) | | 5,2 ↑ | | 2↓ |
| X | N.medianus | 58 | 2,6 | 24 | |
| X | N.ulnaris | 53 | 2,7 | 20 | |
| X | N.lateral antebrachial cutaneous | 58 | 1,9 | 22 | |
| X | N.medianus | 53 | 2,9 | | 9 |
| X | N.ulnaris | 54 | 2,5 | | 10 |
| X | N.radialis | 56 | 2,2 | | 4 |
| X | N. musculacutaneus (Erb’s-m.biceps) | | 4,4 | | 8 |
| X | N. radialis (Erb’s-m. triceps) | | 5,7 | | 8 |
| X | N.axillaris (Erb’s-m. deltoid) | | 4,3 | | 5 |
Based on the evaluation of his medical history, physical examination and laboratory data, the patient was diagnosed with IBN. He was referred to Haematology and Radiation Oncology Department for further multiple myeloma treatment.
Discussion
IBN is an uncommon neuropathy, which shows various lower motor symptoms and asymmetrical involvement. The aetiology is unknown but is thought to be autoimmune due to precursory events [1]. IBN starts with a sharp one sided acute severe pain attack at shoulders, trapezius, scapular area, arms and forearms. This pain decreases within 2-4 weeks. Rapidly progressive muscle weakness and atrophy develop within the weeks following the reduction of pain. It most commonly affects the upper trunk and shoulder girdle muscles [2]. The majority of patients show a slow recovery in motor functions in 6-18 months [1].
IBN affects men more than women. Even though the pathophysiology of IBN remains uncertain, a trigger event (upper respiratory tract infection, vaccination, surgical and emotional stress etc.,) is defined a few days before its appearance in 28-83% of cases [1]. Nerve biopsy shows perivascular T cell infiltration, germinal center B-lymphocytes and antibodies against peripheral nerve myelin along with axonal degeneration [3]. This inflammatory process, which infiltrated brachial plexus nerve fibers, is believed to originate from an autoimmune pathology [4].
Multiple myeloma is a neoplastic plasma cell disease characterised by clonal proliferation of malignant plasma cells in the bone marrow, monoclonal protein in serum or urine and anaemia, renal failure, hypercalcaemia, and bone lesions [5]. According to International Myeloma Working Group Guidelines, the diagnosis of multiple myeloma can be made when the three following criteria met: elevated levels of monoclonal protein in the blood or urine, over 10% plasma cells in a bone marrow sample and/or plasmacytoma on tissue biopsy and myeloma related organ dysfunction (>1, hypercalcaemia, renal insufficiency, anaemia, lytic bone lesions) [6]. As a result of elevated M protein levels in the blood, 80% atypical clonal cell in bone marrow and osteolytic lesions; our patient was diagnosed with IgG kappa myeloma.
The most common peripheral neurologic involvement of multiple myeloma patients is the spinal cord/nerve root compression caused by a plasmacytoma [7]. One third of multiple myeloma patient’s present peripheral Polyneuropathy (PN). Sensory symptoms at PN are explicit and moderate at IgM type multiple myeloma patients with anti-Myelin-Associated Glycoprotein (anti-MAG) [8]. Although IgG or IgA type multiple myeloma patients having PN are less common than IgM type multiple myeloma patients, it emerges in a similar way to Chronic Inflammatory Demyelinating PN (CIDP) [7]. Invasion of peripheral nerve axons by amyloidosis often deemed to be the cause of diffuse sensorimotor PN aetiology in multiple myeloma [9].
The indexed patient had plexopathy symptoms that continued for one year and they were no related factors which could be the trigger of IBN. Upper-middle trunks involvement was found in EMG. There was no pathology on MRI of the brachial plexus. IBN MRI might show moderate thickening in plexus and hyperintensity T2-weighted imaging; however, MRI findings also can be detected normal [10].
IBN association with multiple myeloma has not been reported in the literature before.
Conclusion
Aetiology of IBN is still unknown, however, it is considered as an autoimmune disease due to nerve biopsy studies. It is also known that autoimmune peripheral nervous system diseases as CIDP may occur in IgG multiple myeloma. Since, in our case, there were two autoimmune events at the same time and there was no other trigger for IBN; the immune response of peripheral nervous system is thought to be triggered by IgG multiple myeloma.
[1]. Khadilkar SV, Khade SS, Brachial plexopathyAnn Indian Acad Neurol 2013 16:12-18. [Google Scholar]
[2]. Sumner AJ, Idiopathic brachial neuritisNeurosurgery 2009 65:150-52. [Google Scholar]
[3]. van Alfen N, Clinical and pathophysiological concepts of neuralgic amyotrophyNat Rev Neurol 2011 7:315-22. [Google Scholar]
[4]. Vriesendorp FJ, Dmytrenko GS, Dietrich T, Koski CL, Antiperipheral nerve myelin antibodies and terminal activation products of complement in serum of patients with acute brachial plexus neuropathyArch Neurol 1993 50:1301-03. [Google Scholar]
[5]. Durie BG, Kyle RA, Belch A, Bensinger W, Blade J, Boccadoro M, Myeloma management guidelines: A consensus report from the scientific advisors of the International Myeloma FoundationHaematology J 2003 4:379-98. [Google Scholar]
[6]. Palumbo A, Sezer O, Kyle R, Miguel JS, Orlowski RZ, Moreau P, International Myeloma Working Group Guidelines for the management of the multiple myeloma patients ineligible for standard high dose chemotherapy with autologous stem cell transplantationLeukemia 2009 23(10):1716-13. [Google Scholar]
[7]. Blade J, Rosinol L, Complications of multiple myelomaHaematol Oncol Clin North Ame 2007 21:1231-46. [Google Scholar]
[8]. Latov N, Hays AP, Sherman WH, Peripheral neuropathy and anti MAG antibodiesCrit rev neurobiol 1988 3:301-32. [Google Scholar]
[9]. Darnell RB, Posner JB, Paraneoplastic syndromes affecting the nervous systemSeminoncol 2006 33:270-98. [Google Scholar]
[10]. Scalf RE, Wenger DE, Frick MA, Mandrekar JN, Adkins MC, MRI findings of 26 patients with Parsonage-Turner syndromeAJR Am J Roentgenol 2007 189:39-44. [Google Scholar]