Bilateral Giant Juvenile Fibroadenoma of Breast
Nikhil Makkar1, Sumitoj Singh2, Surinder Paul3, Mandeep Singh Sandhu4, Ashok Kumar5
1 Junior Resident, Department of General Surgery, Government Medical College, Amritsar, Punjab, India.
2 Associate Professor, Department of General Surgery, Government Medical College, Amritsar, Punjab, India.
3 Professor, Department of Pathology, Government Medical College, Amritsar, Punjab, India.
4 Senior Resident, Department of General Surgery, Government Medical College, Amritsar, Punjab, India.
5 Assistant Professor, Department of General Surgery, Government Medical College, Amritsar, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sumitoj Singh, C-12, Medical College Campus, Amritsar-143001, Punjab, India.
E-mail: sumitoj@rediffmail.com
Fibroadenomas are benign lesions of breast commonly found in young age group. These focal tumours contain both mesenchymal and glandular tissue. Giant juvenile fibroma of breast is rare variant of fibroadenoma found usually in less than 20 years of age. They present with rapid enlargement of single or multiple, discrete, painless large nodule of breast. A 14-years-old premenarche girl presented with large bilateral breast lumps for two months. FNAC showed features of juvenile fibroadenoma. Breast conserving surgical excision of lumps was performed and histopathology confirmed the diagnosis of juvenile fibroadenoma. Giant juvenile fibroadenomas are characterised by rapid enlargement of encapsulated mass. The aetiology is unknown, although end-organ hypersensitivity to normal level of estrogen is postulated. We present a case of bilateral giant juvenile fibroadenoma for its rarity.
Adolescent, Giant fibroadenoma Breast, Phyllodes
Case Report
A 14-year-old premenarche girl presented with bilateral large breast lumps for two months [Table/Fig-1]. There was no history of pain, nipple discharge, skin ulceration, fever, anorexia, cough, weight loss and any trauma. Family history was not relevant.
Preoperative image of breasts showing bilateral breast swellings

On breast examination, well defined, firm lumps were present and the overlying skin and local temperature was normal. The right lump was 6 x 5 cm and on left side two lumps were present of size 10 x 6 cm and 2 x 3 cm. They were freely mobile, not fixed to underlying structures or skin. There was no axillary lymphadenopathy. Nipple areola complex was normal with no nipple discharge. Haemogram and routine biochemical investigation were within normal limits. Mammography was not done, as in young patient with dense glandular breast mammography is not recommended.
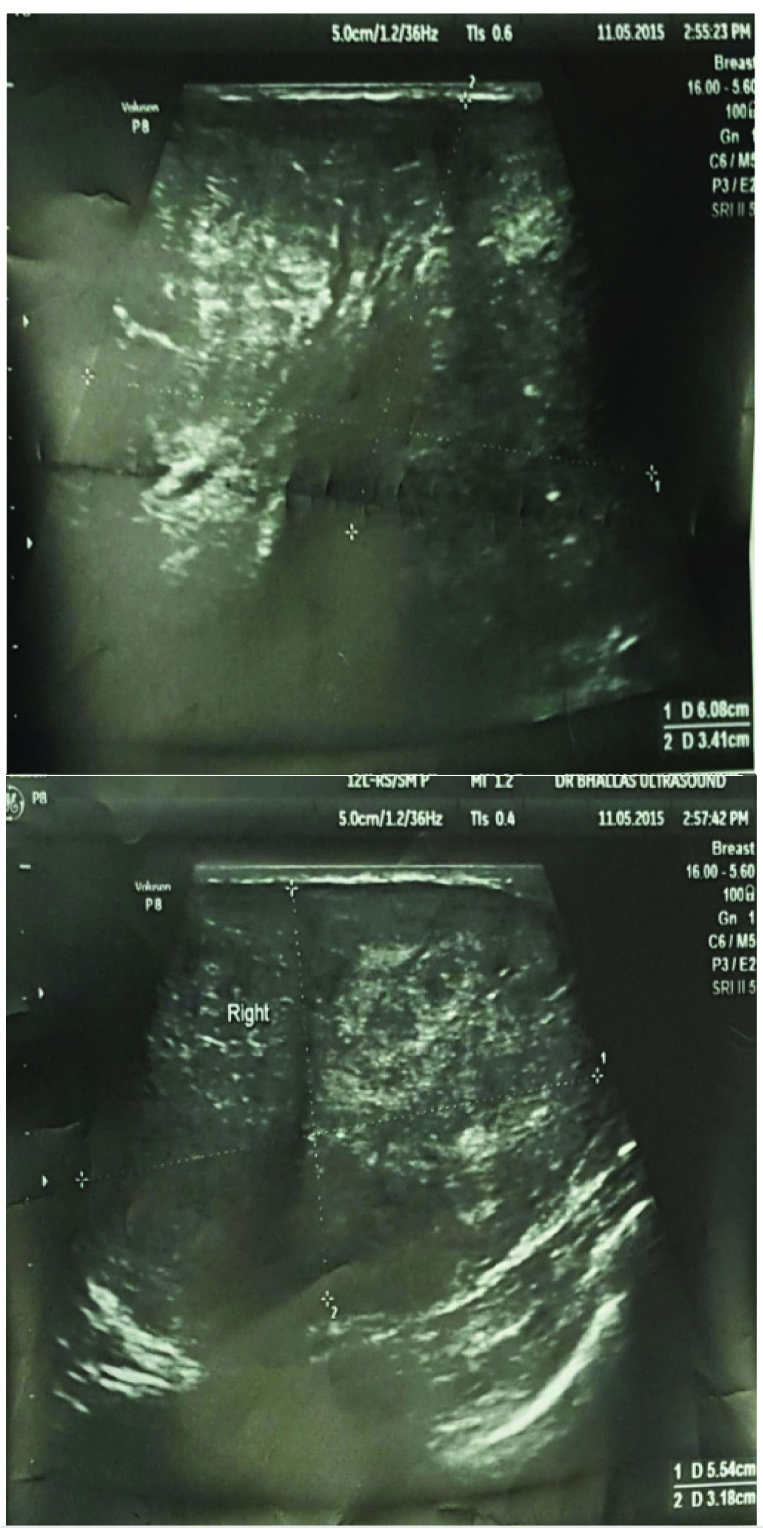
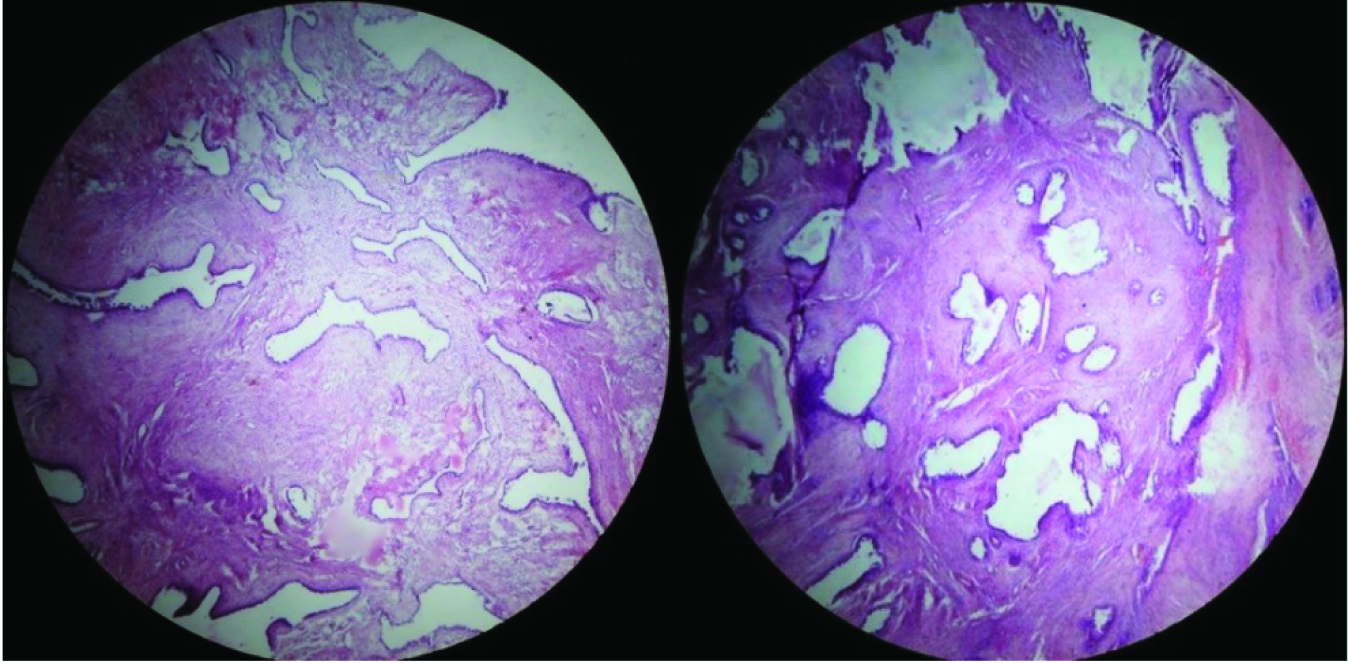
On ultrasonography bilateral lumps showed heterogeneous parenchymal pattern [Table/Fig-2]. Fine-Needle Aspiration Cytology (FNAC) of bilateral breast lumps yielded blood mixed aspirate showing bimodal pattern containing epithelial and stromal fragments with benign epithelial cells arranged in large mono layered sheets. Numerous single and bare bipolar nuclei were seen against the background of fibromyxoid stroma with stromal proliferation. Bilateral breast lumps were excised and histopathology findings from the Haematoxylin and Eosin stained sections showed pericanalicular epithelial growth pattern along with ductal hyperplasia and stromal cellularity at places with no evidence of mitosis suggesting diagnosis of giant juvenile fibroadenoma [Table/Fig-3,4]. Patient was followed up to six months and there were no fresh complaints.
Ultrasound breast: left and right breasts showing oval hypodense circumscribed lesion.
Photograph of excised right and left breast swellings.

Histopathology of right and left breast swelling showing proliferation of epithelial and stromal cells but lacking the leaf-like growth pattern (H&E, × 40).
Discussion
Benign breast disorders are common in females younger than 30 years, but such masses are not common in juvenile or premenarche age groups [1]. Fibroadenomas are common benign biphasic tumours of breast consisting of a circumscribed breast neoplasm, featuring proliferation of both epithelial and stromal elements. It is the most common tumour in women younger than 30 years presenting as painless, slow growing, mobile well defined firm nodules [2]. Juvenile fibroadenomas are defined as benign breast tumour occurring in adolescent females with stromal and epithelial hyper-cellularity but lacking the leaf like growth pattern of phyllodes tumours [3]. Fibroadenomas having size more than 5 cm are considered as giant fibroadenomas. The juvenile fibroadenoma constitutes 4% of the total fibroadenomas, and giant juvenile fibroadenoma constitutes only 0.5% of them [4]. Bilateral giant juvenile fibroadenomas are extremely rare with only few cases reported in English literature [4-13] [Table/Fig-5]. The term juvenile and giant fibroadenoma are used predominantly in adolescents and for massive fibroadenoma with usual histology, with sizes >5 cm or weight >500 gm respectively. Differential diagnosis of juvenile fibroadenoma is benign low grade phyllodes tumour, virginal hypertrophy, lipoma, Pseudoangiomatous Stromal Hyperplasia (PASH), hamartomas, breast abscess, macrocysts and carcinomas [14]. On mammography fibroadenomas are well circumscribed discrete oval mass which is either hypodense or isodense to glandular tissue or may present with a lobulated mass with or without calcification. Mammography lack sensitivity to distinguish between cysts and fibroadenoma but they can be easily distinguished by ultrasonography [15]. On ultrasonography fibroadenomas are well circumscribed round to ovoid mass with uniform hypo-echogenisity. The sonographic finding of juvenile fibroadenoma is similar as simple fibroadenoma, as well circumscribed, discrete oval hypo or isodense mass compared to glandular breast tissue. Occasionally sonographic appearance of a thin echogenic rim (pseudocapsule) may be found. They frequently show posterior acoustic enhancement and hypervascularity on colour Doppler sonography [16]. On excision, they are seen as well encapsulated masses.
Previously reported cases.
| S. No. | Author name (year) | Age | Clinical Features | USG Findings |
|---|
| 1 | Biswas SK et al., [5] | 14 yrs | Rapidly enlarging right breast lumps for four months, firm to hard irregular mass of size 15 x 13 cm | Heterogenous parenchymal pattern s/o bilateral fibroadenoma |
| 2 | Mukhopadhyay M et al., [6] | 11 yrs | Premenarche girl with bilateral rapid growing breast lumps, mobile slightly tender and lobulated. Right breast lump of 22 x 20 cm and left breast lump of 18 x 16 cm | Heterogenous parenchymal pattern |
| 3 | Khan S et al., [7] | 10 yrs | Progressive enlargement of both breasts for 1 yr, freely mobile with variable consistency. Right breast of size 6 x 5 cm and left of 10 x 15 cm | Solid bilateral breast lesion sign of fibroadenoma |
| 4 | Kaur N et al., [8] | 15 yrs | Girl with a six month history of rapidly growing breasts, large, diffuse nodular breasts with marked asymmetry | Fibroadenoma on ultrasonographyand FNAC |
| 5 | Baxi M et al., [9] | 16 yrs | Two yrs history of multiple painless and progressively enlarging hard, mobile, b/l lumps in breast and axilla varying in size from 2-8 cm | Mobile hypodense hypoechoic lesion sign of fibroadenoma |
| 6 | Lee CJ et al., [10] | 11 yrs | Extremely large and slightly asymmetric breasts for one year | Mobile hypodense lesion sign of bilateral fibroadenoma |
| 7 | Goyal S et al., [11] | 11 yrs | Rapidly enlarging right breast lump for three months(16X13 cm) | Parenchymal heterogenous sign of fibroadenoma |
| 8 | Nikumbh DB et al., [12] | 12 yrs | Premenstrual girl with right breast lump of 15 x 12 and left of 17 x 15 cm, bilateral mobile | Bilateral heterogenous parenchymal patterns |
| 9 | Muthukumaran J et al., [13] | 11 yrs | Girl with enlarging lump of 6 x 5 cm in left breast | Lesion of 5 x 6 x 5 cm sign of fibroadenoma |
| 10 | Beniwal K et al., [14] (2 cases) | a) 13 yrs b) 11 yrs | a) Rapid enlarging lump on left breast for four months b) Enlarging lump of right breast for two months | a) Ultrasonography showing lesion of 12 x 8 x 7.5 cm b) Hypodense lesion of 10 x 7 x 6.5 cm sign of giant fibroadenoma |
| 11 | Present case | 14 yrs | Premenarche girl with large bilateral mobile lumps of breast | Bilateral hypodense heterogenous parenchymal lesion |
The diagnostic criteria for juvenile fibroadenoma are a circumscribed mass, uniformly hypercellular stroma with frequent epithelial and myoepithelial hyperplasia having biphasic stromal and epithelial components and mostly occurring in patients in age group of 10-20 years. Histologically they have more cellular component than usual fibroadenoma. Most juvenile fibroadenomas show noticeable epithelial hyperplasia with a ductal, lobular, or combined ductal-lobular pattern [17]. Pathogenesis includes excessive stimulation of oestrogen and progesterone or increased receptor sensitivity. During puberty reduced levels of oestrogen antagonist have also been implicated in its pathogenesis [18].
Immunohistology shows stromal cells CD34, Factor XIIIa positive. Smooth muscle actin is more frequently positive than in adult fibroadenoma [1].
It is important to distinguish preoperatively among these entities as the treatment modalities and the prognosis differ markedly in these conditions. FNAC and biopsy easily rule out these conditions and managed accordingly.
Phyllodes tumour is an uncommon fibroepithelial tumour that can affect all age groups but usually present in the age group above 40 years. Usually they present as a single mass, rarely involve both breasts and can be benign, borderline or malignant depending on histologic variables. In low-grade phyllodes tumour, there is prominent leaf-like architecture and stromal condensation around the ducts and infiltration in the surrounding breast tissue with mitotic figures<4 per High Power Field (HPF). In high-grade phyllodes tumour, stromal overgrowth with atypia and atypical mitotic figures (<10 per HPF) are seen. They are treated by wide excision with a margin of normal tissue or by simple mastectomy [19].
Juvenile breast hypertrophy presents as rapid distressing enlargement of one or both breasts, which is often asymmetrical. Histologically abundant connective tissue and duct proliferation is seen, frequently associated with epithelial hyperplasia but little or no lobule formation [20].
Giant lipoma usually present as unilateral breast hypertrophy characterised by soft, mobile mass. On histology, encapsulated nodules of mature adipose tissue can be seen [21]. Breast abscesses present clinically with sign and symptoms of an abscess like pain, fever erythema and fluctuation. On biopsy focal collection of polymorphs with necrotic material is seen.
Hamartomas present as multilobular structures. Microscopically, these lesions present as a mixture of ducts, lobules, fibrous stroma, and adipose tissue.
Pseudoangiomatous stromal hyperplasia is a rare cause of gigantic breast characterised by dense, collagenous proliferation of the mammary stroma, seen as complex inter anastomosing spaces. These have spindle-shaped stromal cells at their margins simulating endothelial cells. FNAC and biopsy easily rule out these conditions [22].
Another entity named Carneys complex present with bilateral juvenile fibroadenomas in form of multiple myxofibroadenomas. It is associated with other features like cardiac myxomas, endocrine hyperactivity, cutaneous manifestations in form of hyperpigmentation and other abnormalities [23]. Though malignant tumours of the breast are rare in adolescents, still 2% of all primary malignant tumours occur in less than 25 years of age in females [24].
Conclusion
It is rare that young females present with breast masses, but the consideration of fibroadenoma or giant juvenile fibroadenoma in these cases is always warranted. These cases need thorough clinical evaluation, investigations and treatment by surgery for the better aesthetic outcomes to the patient. Here in this case report we present a rare case of bilateral juvenile fibroadenoma. It was removed by excision of the tumours, preserving the normal breast tissue, nipple and aerola. The patient is doing well on regular follow-up of six months.
[1]. Valdes EK, Boolbol SK, Cohen JM, Feldman SM, Malignant transformation of a breast fibroadenoma to cystosarcoma phyllodes: case report and review of theliteratureAm Surg 2005 71(4):348-53. [Google Scholar]
[2]. Yagnik VD, Juvenile giant fibroadenomaClin Pract 2011 1(3):e49 [Google Scholar]
[3]. Kempson RL, Rouse RV, Juvenile fibroadenoma of the breast. Stanford school of medicinehttp://surgpathcriteria.stanford.edu/breast/juvfibroadenoma/ [Google Scholar]
[4]. Dent DM, Cant PJ, FibroadenomaWorld J Surg 1989 13(6):706-10. [Google Scholar]
[5]. Biswas SK, Rehman T, Paul AC, Giant juvenile fibroadenoma of breastFaridpur Med Coll J 2012 7(1):42-45. [Google Scholar]
[6]. Mukhopadhyay M, Patra R, Mondal S, Ghosh A, Ray AK, Bilateral giant juvenile fibromas of breastsJ Indian Assoc Pediatric Surg 2009 14(2):68-69. [Google Scholar]
[7]. Khan S, Khan M, Rafique S, Giant juvenile fibroadenoma of breast in pre-pubescent girlJournal of the College of Physicians and Surgeons Pakistan 2015 25:S95-96. [Google Scholar]
[8]. Kaur N, Saini S, Somasekhar S, Bilateral florid juvenile fibroadenomas of the breast in an adolescent: a rare indication for subcutaneous mastectomyJ Pediatr Adolesc Gynecol 2015 28(5):e135-37. [Google Scholar]
[9]. Baxi M, Agarwal A, Mishra A, Agarwal G, Mishra SK, Multiple bilateral Juvenile fibroadenomas of breastEur J Surg 2000 166(10):828-30. [Google Scholar]
[10]. Lee CJ, Kim YJ, Seo YT, Pak SJ, Lee SI, Treatment of multiple bilateral juvenile fibroadenomas in a teenage breast by central pedicle breast reduction, with vertical and short horizontal scar: case reportAesthetic Plast Surg 2004 28(4):228-30. [Google Scholar]
[11]. Goyal S, Garg G, Narang S, Giant fibroadenoma of the breast in a pre-pubertal girl: a case reportInt J Cancer Ther Oncol 2014 2(1):020113 [Google Scholar]
[12]. Nikumbh DB, Desai SR, Madan PS, Patil NJ, Wader JV, Bilateral giant juvenile fibroadenomas of breasts: a case reportPathology Research International 2011 2011:482046 [Google Scholar]
[13]. Muthukumaran J, Krishnan N, Vivek S, Giant juvenile fibroadenoma of the breast – a case reportIndian Journal of Applied Research 2015 5(7):222-23. [Google Scholar]
[14]. Beniwal K, Aggarwal D, Kaur S, Giant juvenile fibroadenoma: report of two casesAsian Pac J Health Sci 2015 2(1):95-98. [Google Scholar]
[15]. Taori K, Dhakate S, Rathod J, Hatgaonkar A, Disawal A, Wavare P, Evaluation of breast masses using mammography and sonography as first line investigationsOpen Journal of Medical Imaging 2013 3:40-49. [Google Scholar]
[16]. Kim SJ, Park YM, Jung SJ, Lee KH, Sonographic appearances of juvenile fibroadenoma of the breastJ Ultrasound Med 2014 33(11):1879-84. [Google Scholar]
[17]. Pettinato G, Manivel JC, Kelly DR, Wold LE, Dehner LP, Lesions of the breast in children exclusive of typical fibroadenoma and gynecomastia. A clinicopathologic study of 113 casesPathol Annu 1989 24(Pt 2):296-328. [Google Scholar]
[18]. Tochika N, Ogawa Y, Kumon M, Araki K, Sugimoto T, Ohtsuki Y, Rapid growing fibroadenoma in an adolescentBreast Cancer 1998 5:321-24. [Google Scholar]
[19]. Mishra SP, Tiwary SK, Mishra M, Khanna AK, Phyllodes tumour of breast: a review articleISRN Surgery 2013 2013:361469 [Google Scholar]
[20]. Griffith JR, Virginal breast hypertrophyJ Adolesc Health Care 1989 10(5):423-32. [Google Scholar]
[21]. Li YF, Lv MH, Chen LF, Wu YF, Giant lipoma of the breast: a case report and review of the literatureClin Breast Cancer 2011 11(6):420-22. [Google Scholar]
[22]. Roy M, Lee J, Aldekhayel S, Dionisopoulos T, Pseudoangiomatous stromal hyperplasia: A rare cause of idiopathic gigantomastiaPlast Reconstr Surg Glob Open 2015 3(9):e501 [Google Scholar]
[23]. Irwin GW, Somerville JE, McIntosh SA, Refsum SE, The management of breast problems in Carney’s syndrome: A report of two cases and review of the literatureJournal of Plastic, Reconstructive & Aesthetic Surgery 2014 67(6):e169-e170. [Google Scholar]
[24]. Chang DS, McGrath MH, Management of benign tumours of adolescent breastPlastic and Reconstruction Surgery 2007 120(1):13-17. [Google Scholar]