Idiopathic Tumoral Calcinosis – Rare Clinico Pathological Entity: A Report of Two Cases
Sreedevi Jakka1, Radhika Narayan2, Minakshi Mishra3, Farah Rana4, J.K. Laik5
1 Specialist, Department of Pathology, Tata Main Hospital, Jamshedpur, Jharkhand, India.
2 Consultant, Department of Pathology, Tata Main Hospital, Jamshedpur, Jharkhand, India.
3 Head Consultant, Department of Pathology, Tata Main Hospital, Jamshedpur, Jharkhand, India.
4 Specialist, Department of Pathology, Tata Main Hospital, Jamshedpur, Jharkhand, India.
5 Consultant, Department of Pathology, Tata Main Hospital, Jamshedpur, Jharkhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sreedevi Jakka, Specialist, Department of Pathology, Tata Main Hospital Qt No. 2, Road No-5, Ramnagar, Sonari, Jamshedpur, Jharkhand, India.
E-mail: drjsreedevi@yahoo.com
Tumoral calcinosis is a rare disease reported mainly in blacks of tropical and subtropical African regions. It is characterized by tumour-like periarticular deposits of calcium that are found in the regions of the hip, shoulder, elbow and small joints of hands and feet. The involvement of this disease in a healthy patient is extremely rare in young and middle aged individuals. We are presenting two cases with large, painless periarticular swellings in subscapular joint and feet. First case presented with recurrent swelling in different anatomical locations at different time intervals involving the hip and followed by shoulder joint. Second case presented with swelling around the ankle joint. These two cases were diagnosed as Idiopathic tumoral calcinosis based on biochemical, radiological and histopathological findings.
Calcification, Periarticular deposits, Tumour like condition
Case-1
A 22-year-old female presented with large swelling on the right sub scapular region for two years duration. It gradually increased in size approximately 9 x 7 x 6 cm, situated in dorsal aspect of shoulder complex near the tip of scapula. Previously; she was operated for similar swelling of gluteal region two years back. There was no family history and trauma. General examination was within normal limit. Local examination showed large size, subcutaneous swelling involving the lateral border and angle of scapula, which was firm to hard in consistency, not adherent to underlying muscle. Rib cage and skin over the swelling appeared normal. It was associated with mild pain and tenderness.
Blood investigations included complete blood count - normal, Hbs Ag - negative, HCV Ab - negative, HIV I and II - negative, serum creatinine - 0.9 mg/dl, serum calcium - 9.0 mg/dl, serum phosphorus 3.6mg/dl, serum PTH – 56 ng/dl, Vit D- 10 ng/dl, ALP – 49.2mg/dl, serum uric acid – 2.9 mg/ dl were within normal limits, except ESR – 49mm (westergrens method) and CRP – 15.7 mg/dl.
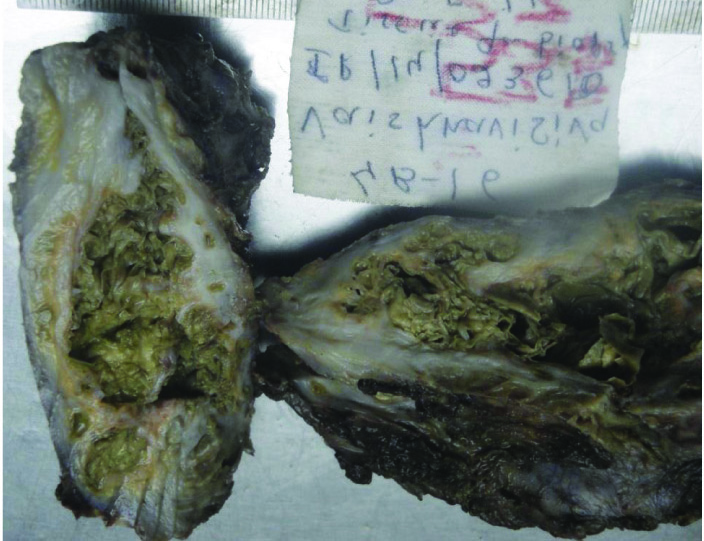
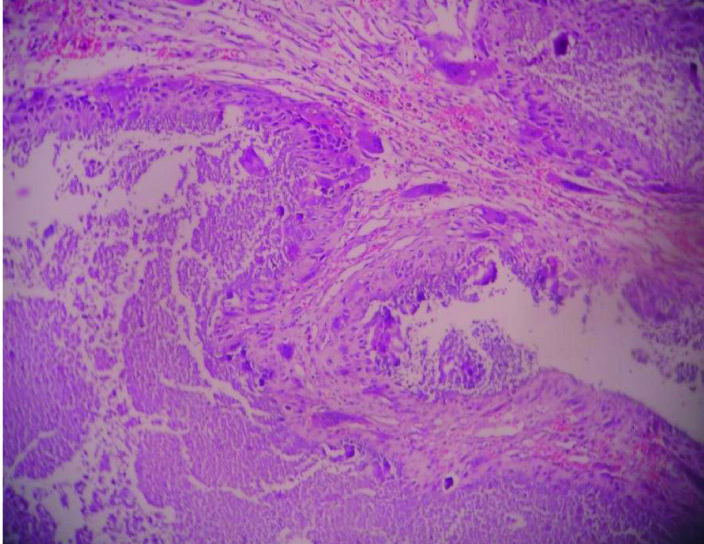
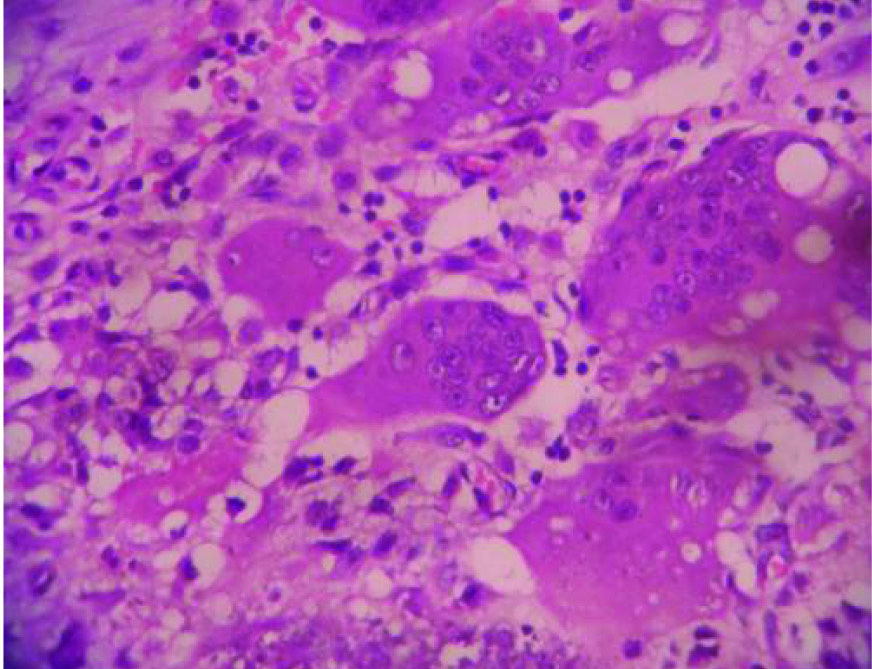
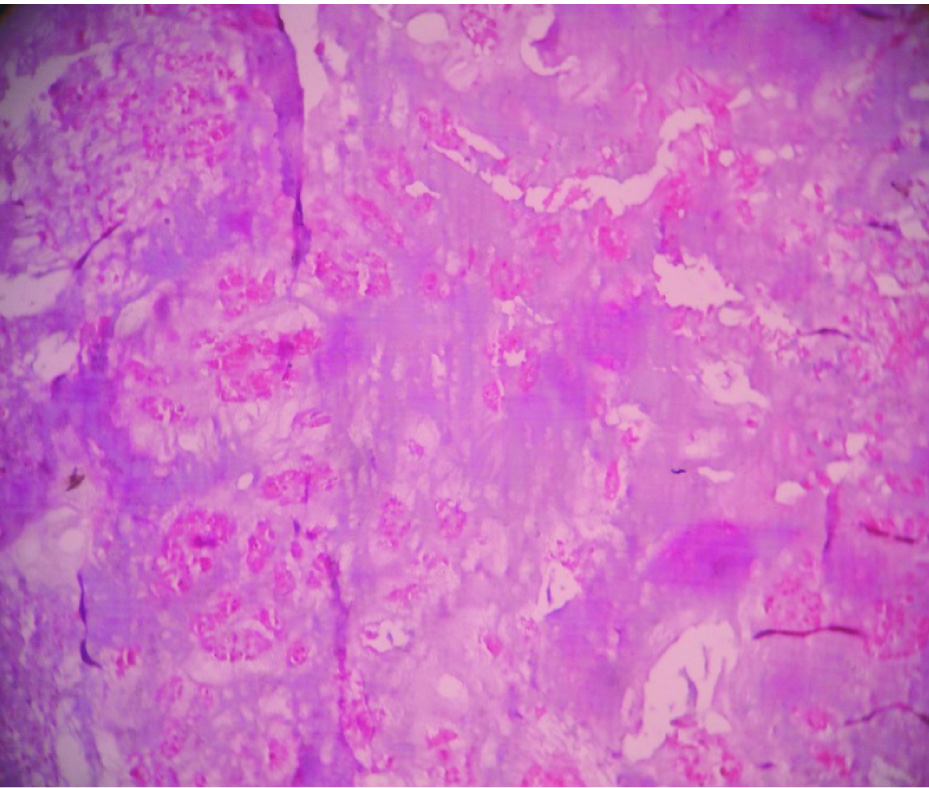
CECT findings showed subcutaneous multiple, rounded opacities separated by radiolucent lines (fibrous septa), which lie outside the joint capsule [Table/Fig-1]. Under general anaesthesia, the mass was removed enbloc with pseudocapsule and was sent for histopathological examination. Gross findings revealed a well-defined mass with spongy, cystic spaces filled with yellowish necrotic debris and thickened wall [Table/Fig-2]. Microscopy showed cystic spaces filled with necrotic calcified material, lymphoplasmacytic infiltrate, fair number of histiocytic and multinucleated osteoclastic type giant cells [Table/Fig-3,4]. Causes that may be responsible for calcification like chronic renal failure, primary hyperparathyroidism and myositis ossificans were ruled out. So a final diagnosis of idiopathic Tumoral calcinosis was given. We followed up the patient and observed that there was no recurrence.
CECT shows multiple round opacities separated by radiolucent lines at periarticular soft tissue deposits.

Gross photograph shows lobulated mass. Cut section reveals cystic space filled with necrotic debris.
Cystic spaces lined by dense inflammatory infiltrate, necrosis, few multinucleate giant cells (H&E 10X).
Osteoclast type multinucleate type giant cells, each consists of 10-25 nuclei per cell (H&E 40X).
Case-2
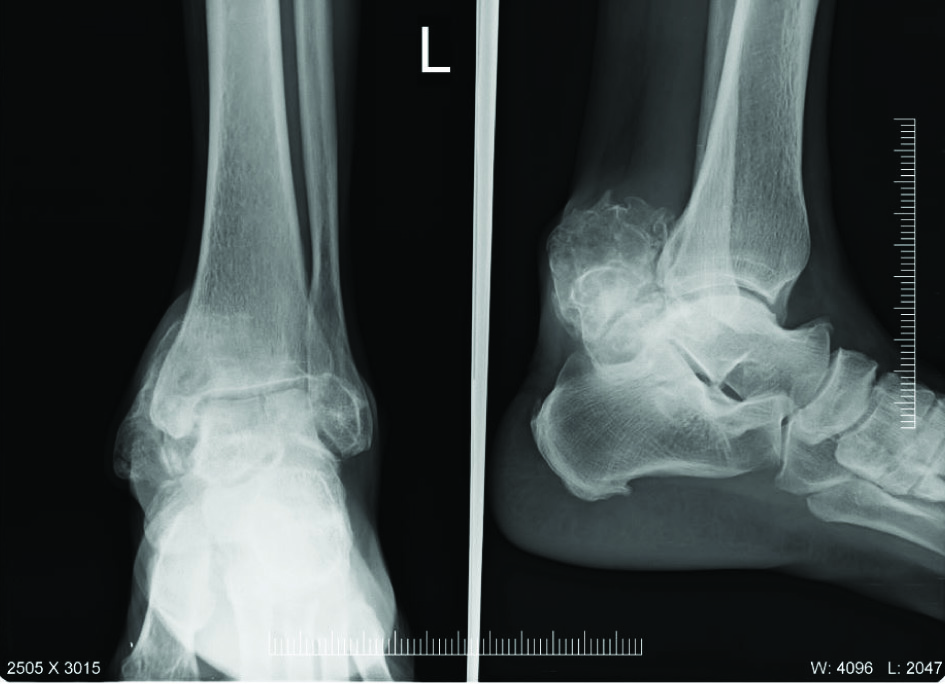
A single bony swelling over left dorsal aspect of feet and ankle region since 4 years was presented in a 49-year-old male [Table/Fig-5]. It was slowly growing over a long time and there was no history of trauma. On local examination, there was a bony hard swelling, free of overlying skin, mobile in mediolateral plane. Blood test results of complete blood count, serum calcium, phosphorus, creatinine, serum Parathormone (PTH), Antinuclear Antibody Test (ANA) which all were within normal limits.
Subcutaneous, hard swelling located in medial and posterior aspect of left ankle joint.

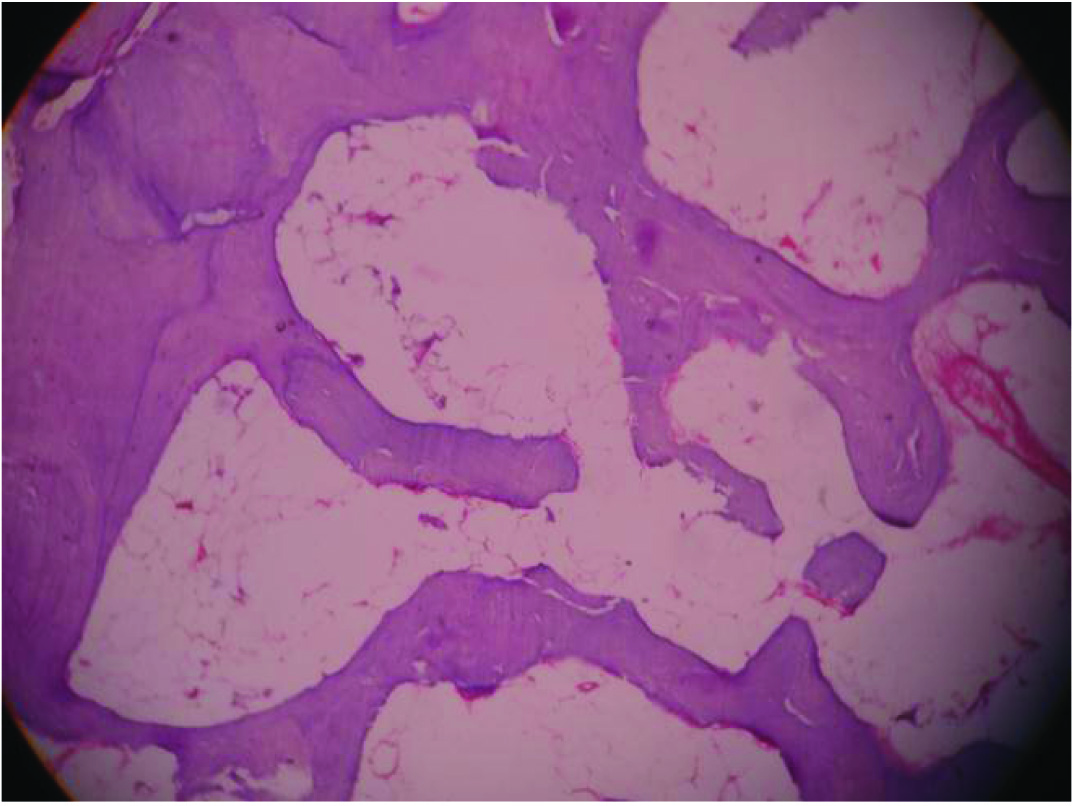
X-Ray findings showed large well defined mass close to the bone [Table/Fig-6]. CT scan was not done due to financial constraints and remote location of patient. Surgical excision was planned due to discomfort during wearing of shoes. Intraoperative findings were multiple calcified masses under tendo achilles enclosed in extensor retinaculum and free of underlying bone/joint. Gross findings were irregular, hard, creamish white, bone like compact mass measuring 6 x 5 x 4 cm. Microscopic findings were large areas of calcification, cartilagenous and focal osseous differentiation [Table/Fig-7,8]. The final diagnosis was idiopathic tumoral calcinosis in osseous stage. No recurrence was observed during follow up.
X-Ray lateral view shows multiple, small radiopacities in periarticular area of ankle joint.
Large areas of calcification and few vascular spaces (H&E 10X).
Osseous differentiation with fibroadipose tissue (H&E 10X)
Discussion
In 1943 tumoral calcinosis was proposed by Inclan [1]. These lesions consist of crystals of calcium hydroxy apatite and amorphous calcium phosphate which are commonly located around extensor surface of large joints, hip, elbow, shoulder, small joints of hands and foot. Adolescents and young adults are commonly affected [1]. In our first case, the young girl was presented with recurrent swelling involving the different anatomical location in hip and shoulder joint and in second case the swelling presented around the foot in a middle aged male. The unique presentation is painless, non-tender firm, rubbery masses [2]. Both cases were presented with firm to hard painless masses for a long time.
The exact cause is not known, but the disease has been reported in siblings. In our cases siblings were not affected. Tumoral calcinosis occurs in sporadic/familial inheritance. The familial form is associated with either hyperphosphatemia or a normo phosphatemic state inherited as an autosomal recessive gene, concomitant with mutations in GALNT3 gene [3] or the FGF23 gene [4]. Mechanical trauma or repeated juxta articular injury results in reparative response with resultant synovial metaplasia forming bursa with periarticular calcium deposits [5]. In both cases the causative factor was considered as unnoticed minor trauma and sporadic inheritance due to solitary calcification, no significant family history and no evident biochemical abnormalities.
Slavin et al., proposed a three-stage classification scheme consisting of cellular lesions devoid of calcification, cellular cystic lesions with calcification, and finally hypocellular calcified lesions [6]. In the active (cellular) phase a central mass of amorphous or granular calcified material is bounded by abundant proliferation of macrophages, osteoclast-like giant cells, fibroblasts, and chronic inflammatory cells. During the inactive phase there is an entirely calcified material surrounded by dense fibrous material extending into the adjacent tissues [7]. Microscopically both active and inactive forms of disease activity were seen in first and second cases.
In our first case patient had recurrent swellings at hip and shoulder joint at different intervals, so we had worked up for familial type tumoral calcinosis. All investigations were within normal limits, so we ruled it out. Medical treatment in the primary type could be considered before the surgical approach, especially in the hyper-phosphatemic entity.
Conclusion
Tumoral calcinosis is a distinct clinico-radio-pathological entity characterised by soft tissue periarticular calcinosis which mimics true neoplasm. This rare disease is pathologically identical to the soft tissue calcifications in which serum calcium/phosphorus levels increases as in chronic renal insufficiency, prolonged haemo dialysis, and secondary hyperparathyroidism. These two cases highlighted the importance of diagnosing pseudo tumours such as Idiopathic tumoral calcinosis.
[1]. Inclan A, Tumoral calcinosisJAMA 1943 121:490-95.[The JAMA Network] [Google Scholar]
[2]. Harkess JW, Peters HJ, Tumoral calcinosis. A report of six casesJ Bone Joint Surg Am 1967 49(4):721-31.http://jbjs.org/article.aspx?articleid=14711 [PubMed] [Google Scholar]
[3]. Specktor P, Cooper JG, Indelman M, Sprecher E, Hyperphosphatemic familial tumoral calcinosis caused by a mutation in GALNT3 in a European kindredJ Hum Genet 2006 51:487https://www.ncbi.nlm.nih.gov›NCBI›Literature›PubMedCentral(PMC) [Google Scholar]
[4]. Chefetz I, Heller R, Galli-Tsinopoulou A, Richard G, Wollnik B, Indelman M, A novel homozygous missense mutation in FGF23 causes familial tumoral calcinosis associated with disseminated visceral calcificationHum Genet 2005 118:261https://www.ncbi.nlm.nih.gov/pubmed/16151858[Pubmed] [Google Scholar]
[5]. Slavin RE, Wen J, Barmada A, Tumoral calcinosis –a pathogenetic overview:a histological and ultrastructural study with a report of two new cases, one in infancyInt J Surg Pathol 2012 20(5):462-73.Epub 2012 May 21 https://www. ncbi.nlm.nih.gov/pubmed/22614164[Pubmed] [Google Scholar]
[6]. Slavin RE, Wen J, Kumar D, Evans EB, Familial tumoral calcinosis. A clinical, histopathologic, and ultrastructural study with an analysis of its calcifying process and pathogenesisAm J Surg Pathol 1993 17:788https://www.ncbi.nlm.nih.gov/pubmed/8338191[Pubmed] [Google Scholar]
[7]. Kindblom LG, Gunterberg B, Tumoral calcinosis. An ultrastructural analysis and consideration of pathogenesisAPMIS 1988 96:368https://books.google.co.in/books?isbn=0323076157 [Google Scholar]