A Randomized Comparison between Video Demonstration and Verbal Instruction in Improving Rota Haler Technique in Children with Persistent Asthma: A Pilot Study
Archana Arumugom1, Venkatesh Chandrasekaran2
1 Undergraduate Student, Department of Paediatrics, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India.
2 Assistant Professor, Department of Paediatrics, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Venkatesh Chandrasekaran, Assistant Professor, Department of Paediatrics, JIPMER, Dhanvantri Nagar, Puducherry-605006, India.
E-mail: cvenkatesh@hotmail.com
Introduction
Inhalation therapy is the cornerstone in management of asthma. Failure to use the device properly is one of the factors incriminated in poor control of asthma.
Aim
To compare the technique of rota haler use in children with persistent asthma immediately after receiving either verbal instruction or a video based demonstration and again at one month following intervention.
Materials and Methods
A total of 28 children, older than six years attending the childhood asthma clinic of our hospital, who were prescribed rota halers for the first time and who were technique naïve were enrolled into the study, after obtaining informed consent from the parents after meeting inclusion and exclusion criteria. They were then randomly assigned to either verbal instructions (group of 14) or video demonstration group (group of 14), for teaching them the rota haler technique. Their technique was then assessed using a modified version of the inhaler device assessment tool immediately after education and one month after the intervention. The proportions of children with good technique in both groups at both time points were compared.
Results
There was no significant difference in the baseline variables like age, gender, location, socio-economic status and disease duration between both groups. The proportion of children achieving good technique was significantly more in the video group than the oral instruction group at immediate assessment and also at one month post intervention with an odds of 8 and 23.40 respectively (p=0.0262 and 0.0075 respectively).
Conclusion
Video demonstration is effective in improving the technique of rota haler use at immediate assessment and at one month post intervention. Further studies are needed to validate this study and to assess factors that predict successful device use.
Asthma, Child, Dry powder inhaler, Outcome assessment, Video demonstration
Introduction
Inability to use inhaler devices correctly is one of the factors incriminated in poor symptom control in children with asthma. Of the various inhalational devices available for children with asthma, the use of dry powder inhalers (rota haler) emerged as one of the cost-effective methods of drug delivery in resource limited settings especially in older children [1,2]. Additionally, the problem of coordinating dose release with inspiration seen with pressurised metered dose inhalers is overcome by dry powder inhalers (rota halers), since they use inspiratory flow energy to carry the drug dose to the respiratory tract. The rota haler is breath-activated device and minimal coordination is required between actuation and inspiration. They achieve higher pulmonary deposition than meter dose inhalers and they are environmentally friendly as they do not contain propellant gases [3].
To improve the efficacy of rota haler, it is essential to ensure that the patients have proper compliance with the usage of the device. Factors important in patient compliance with therapy include correct use of device, ease and convenience of use of the device and adopting a proper technique while using them [4]. Many children with asthma do not use their inhalational devices correctly and need some kind of education to improve their use [3,5-7]. Though several studies regarding techniques and demonstrations to help patients use inhaler devices in an effective way have been carried out, the role of video aided demonstrations in improving rota haler technique has not yet been studied convincingly.
The aim of the study was to compare the technique of rota haler use in children with persistent asthma immediately after receiving either verbal instruction or video demonstration and again at one month following intervention.
Materials and Methods
This was a pilot open labelled Randomized Controlled Trial (RCT) conducted between 1st June 2016 to 31st July 2016. This study was conceived as initial study to document difference in outcome for sample size calculation for a larger subsequent study comparing verbal instruction versus video demonstration in improving rota haler technique in children with persistent asthma. Children older than six years of age with persistent asthma who are prescribed rota-haler for the first time were included in the study. Children who lack general understanding (those with intellectual disability or sensory impairment), children who were unable to use rota haler effectively due to local causes (local inflammation, anatomical defect) were excluded from the study.
Assuming successful device use to be 25% in control group and 75% in experimental group with a significance level of 5% and a power of 80% a total of 24 children were needed for the trial (superiority trial, binary outcome). We enrolled a total of 28 participants who were randomly assigned to either the control group to whom, the device use was taught by verbal instruction alone or the video aided group, to whom the device use was taught by video demonstration. Computer generated block randomization (sealed envelope.com) was used for sampling. The envelopes containing the codes were prepared by a medical student not involved in the study. The parent was asked to open an opaque envelope numbered serially which contains the code for a particular intervention. Consecutive children aged six years and above attending the childhood asthma clinic of JIPMER with persistent asthma who were newly started on rota haler and who are naïve to rota haler technique were enrolled by the second author and randomized to either receive verbal instruction or a short video demonstration on how to use the rota haler. They were then asked to demonstrate the technique which is scored for appropriateness using a modified version of the Inhaler Device Assessment tool (IDAT) which is a widely used and validated tool for assessing inhaler device use [8]. The verbal instructions and video instructions were standardized so that no additional information is given in any particular group which might modify outcomes.
For the above purpose the assessment tool steps were used for instruction. The verbal instructions were provided by the treating team. The assessment of technique was done immediately after the first demonstration and one month later. The assessment was done by a nursing staff trained in the assessment of device technique using modified IDAT tool and who was not involved in the study.
Baseline parameters like age, sex, parental literacy, socioeconomic status were compared between the two groups. The proportion of children displaying appropriate technique (defined as scoring 5/5 on modified IDAT) was compared between the video demonstration group and verbal demonstration group. Data analysis was done by the first author who was blinded to the codes.
Statistical Analysis
For comparison of means, unpaired t-test with double sided p-value was used. For comparing proportions, Fisher`s-exact test was used. Odds ratio was calculated for primary outcome of interest. Statistical tests were done using Quickcalcs online statistical program. A p-value less than 0.05 were considered significant. The study was approved by undergraduate research monitoring committee, JIPMER and Institute Ethics Committee, JIPMER.
Trial Registration: This trial does not require registration as per Food and Drug administration amendment act 801.
Results
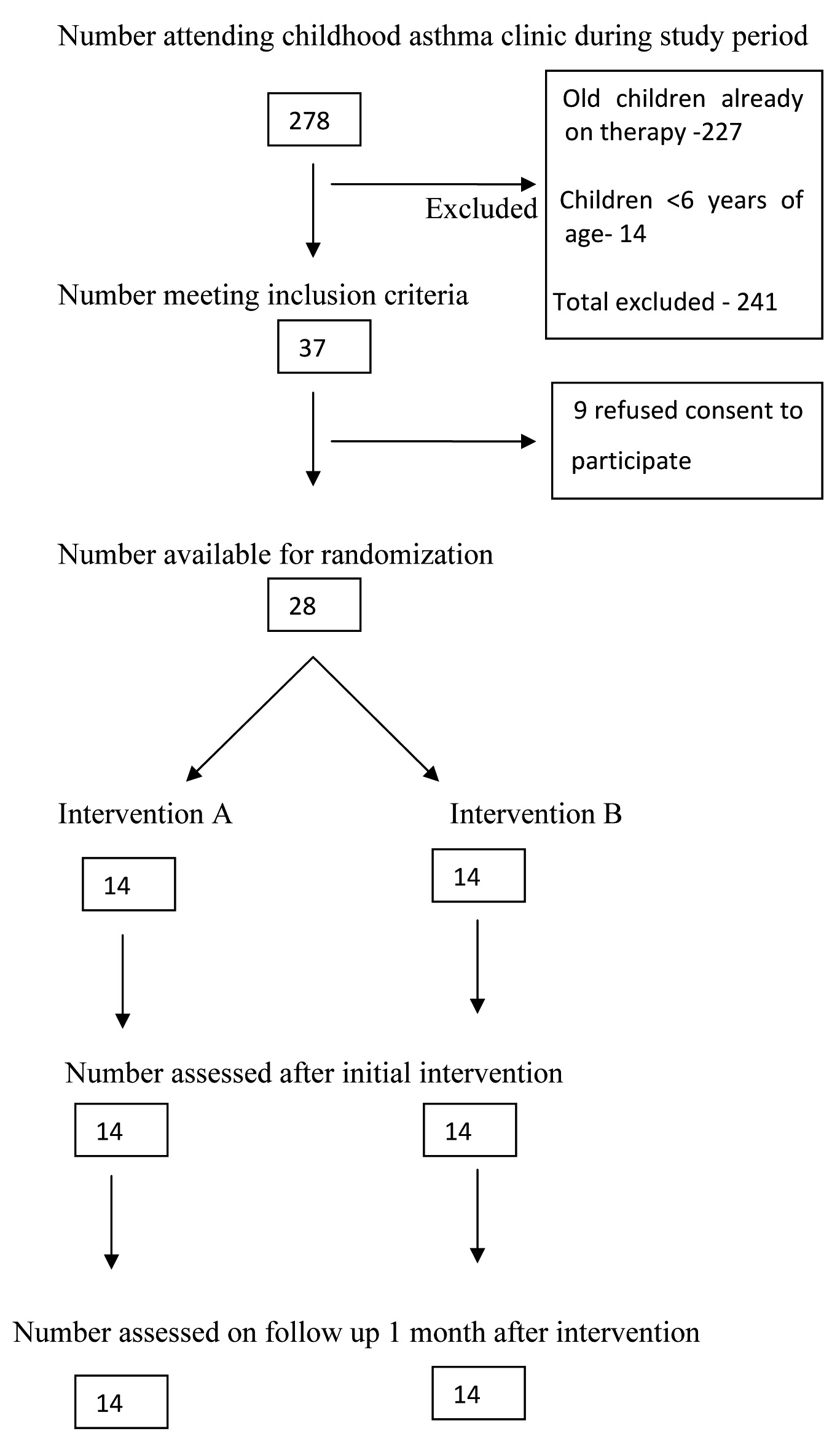
Among the 278 children seen in the asthma clinic during the study period, 37 children met the inclusion criteria for the study. Parents of nine children refused consent for the study and hence excluded ([Table/Fig-1]: consort flow diagram). There was no significant difference between the variables like age, gender, locality, socioeconomic status and disease duration at baseline between the two groups [Table/Fig-2]. The entire study population belonged to upper lower class.
Figure showing consort flow diagram of study participants.
Comparison of background characteristics between the groups.
| Variables | Intervention A | Intervention B | p-value (Fisher’s-exact test and paired t-test*) |
|---|
| Age | 6 to <9 | 9 | 7 | 0.7036 |
| 9 to 12 | 5 | 7 |
| Mean age | 7.75±1.76 | 8.60±2.07 | 0.2524* |
| Gender | Male | 7 | 8 | 1.000 |
| Female | 7 | 6 |
| Locality | rural | 13 | 12 | 0.543 |
| Urban | 1 | 2 |
| SES* | Upper | 0 | 0 | 1.000 |
| UM | 0 | 0 |
| LM | 0 | 0 |
| UL | 14 | 14 |
| LOWER | 0 | 0 |
| Disease duration | <3 years | 6 | 7 | 0.7083 |
| ≥3 years | 8 | 7 |
| Mean disease duration (years) | 3.30±2.33 | 2.45±2.15 | 0.3250* |
SES calculated by modified Kuppuswamy scale (score determines the social class; score based on father/mother's education, occupation and percapita income)
The proportion of children achieving good device technique as assessed by modified IDAT score was high in the intervention B (Video demonstration group) compared to intervention A (verbal instruction group) both at immediate assessment and at 1 month post intervention with a p-value 0.0461 and 0.0044 respectively [Table/Fig-3]. The odds of achieving good technique immediately after intervention is 8 times higher with intervention B when compared to intervention A. Similarly the odd of achieving good technique at 1 month post intervention is 23.40 times higher with intervention B compared to intervention A. The above difference was statistically significant with a p-value of 0.0262 and 0.0075 respectively [Table/Fig-4].
Comparison of primary outcome of interest between the groups during initial scoring and scoring after one month.
| Groups | Proportion achieving 5/5 on IDAT tool (initial) | Proportion achieving 5/5 on IDAT tool (after 1 month) |
|---|
| Intervention A (14) | 2 (14.28%) | 5 (35.71%) |
| Intervention B (14) | 8 (57.14%) | 13 (92.86%) |
| p-value (Fisher’s exact-test) | 0.0461 | 0.0044 |
Odds ratio between exposure and control group.
| Assessment time | Outcome | Exposure (B) (Video demonstration) | Control (A) (Oral instructions) | ODDS RATIO (95% CI) | p-value |
|---|
| Initial | GOOD (IDAT 5/5) | 8 | 2 | 8 (1.2789 to 50.0416) | 0.0262 |
| POOR (IDAT <5) | 6 | 12 |
| One month | GOOD (IDAT 5/5) | 13 | 5 | 23.40 (2.32 to 235.54) | 0.0075 |
| POOR (IDAT <5) | 1 | 9 |
Discussion
From our study, we found that the number of children achieving good rota haler technique was significantly more in the video demonstration group at immediate assessment (57.14% vs 14.28%, p-value =0.0461) as well as during assessment 1 month following intervention (92.86% vs 35.71%, p-value =0.0044).
The children with incorrect technique at both time periods went through a corrective education by the nursing staff for appropriate technique and as a result, we found that higher proportion achieving correct technique at one month post intervention in both groups. This is in contrast to study by Carpenter DM et al., in which video demonstration of metered dose inhalers with or without spacer had improved device use at immediate visit but not at 1 month follow up [6]. Our study differs from theirs in that, our children were between the ages of 6 and 12 years in contrast to 7-17 years in their study and the device used in our study was rota haler in contrast to MDI in theirs.
In a study by Sleath B et al., looking at the proportion of children using their devices correctly, it was seen that only 8.1% performed all the steps correctly for MDIs, 22% for discus and 15.6% for turbu haler [7]. In our study, also we find that 14.28% used the rota haler device correctly in the oral instruction group at immediate assessment which is comparable to the study by Sleath B et al., [7]. However, 57.14% in the video demonstration group performed all the steps correctly.
According to our study, the odds of performing all the steps correctly after video demonstration as compared to verbal instructions at immediate assessment was 8 and after one month of initial assessment it was 23.40 which were both significant (p-value 0.0262 and 0.0075 respectively). Our study is one of the few studies evaluating the technique of rota haler use in technique naïve children using a modified version of IDAT score. Other studies concerning rota haler technique were either carried out in adult patients with chronic obstructive pulmonary disease [9] or in children who were already on rota haler device with prior awareness about using it [10].
Limitation
The limitations of our study are low sample size and hence underpowered to study the individual variables that affect device use and the modified IDAT score for rota haler has not been validated by other studies. Further studies are needed with large sample size to validate our findings and to study the effect of individual variables that predict proper technique of device use.
Conclusion
Video demonstration is an effective way to improve rota haler technique in technique naïve children with persistent asthma, prescribed rota haler for the first time, compared to verbal instructions alone. Re-education to correct the errors committed during device use is important to sustain and improve the proportion of children using the device correctly at 1 month following intervention. Further studies are needed to validate these findings in a large sample.
Funding: The first author recieved stipend from JIPMER as a part of GJ STRAUS project.
*SES calculated by modified Kuppuswamy scale (score determines the social class; score based on father/mother's education, occupation and percapita income)
[1]. van Aaldaren WM, Garcia-Marcos L, Gappa M, Lenney W, Pedersen S, Dekhuijzen R, How to match the currently available inhaler device to an indicidual child with asthma or recurrent wheezeNPJ Prim Care Respir Med 2015 25:14088 [Google Scholar]
[2]. Brand PL, Key issues in inhalation therapy in childrenCurr Med Res Opin 2005 21:S27-32. [Google Scholar]
[3]. Melani AS, Inhalatory therapy training:a priority challenge for the physicianActa Biomed 2007 78:233-45. [Google Scholar]
[4]. Aydemir Y, Assessment of the factors affecting the failure to use inhaler devices before and after trainingRespir Med 2015 109:451-8. [Google Scholar]
[5]. Pedersen S, Dubus JC, Crompton GK, ADMIT Working GroupThe ADMIT series—issues in inhalational therapy 5) Inhaler selection in children with asthmaPrim Care Respir J 2010 19:209-16. [Google Scholar]
[6]. Carpenter DM, Lee C, Blalock SJ, Weaver M, Reuland D, Coyne-Beasley T, Using videos to teach children inhaler technique:a pilot randomized controlled trialJ Asthma 2015 52:81-87. [Google Scholar]
[7]. Sleath B, Ayala GX, Gillette C, Williams D, Davis S, Tudor G, Provider demonstration and assessment of child device technique during pediatric asthma visitsPaediatrics 2011 127:642-48. [Google Scholar]
[8]. Davies B, Danseco E, Cicutto L, Higuchi KS, McConnell H, Edwards N, Nursing best practice guidelines evaluation user guide:inhaler device assessment tool for promoting asthma control in childrenNursing Best Practice Research Unit, University of Ottawa, Canada 2006 :1-30. [Google Scholar]
[9]. Shreshtha S, Sapkota B, Ghimirey A, Shakya R, Impact of counselling on inhalational technique (rotahaler) in chronic obstructive pulmonary disease patientsInt J Pharm 2013 3:442-49. [Google Scholar]
[10]. Prasad SS, Impact of counselling on inhalational technique (rotahaler) in childhood asthma:a prospective pre post intervention studyJournal of Evolution of Research in Pediatrics and Neonatology 2015 1:9-11. [Google Scholar]