Alcoholism is a chronic and progressive psychiatric illness described as an unsanctioned, maladaptive, repeated pattern of alcohol ingestion, irrespective of its adverse physical, psychological and social consequences [1,2]. The World Health Organization (WHO) estimates that excessive alcohol consumption is the third largest life style risk factor in the developed world [2]. It is also evident that an excessive intake of alcohol can seriously damage health [3].
Alcohol is consumed by drinking. It may thus inevitably affect the oral cavity, oral mucosa, and teeth of the consumer. Oral sideeffects of alcohol depend on the nature and contents of the drink, its alcohol concentration, and the frequency and amount of consumption [4]. The psychological effects and the personality changes in the abuser may affect the patient-dentist relationship as they take a reduced interest in seeking and paying for dental care. The physiological effect of alcohol intoxication may lead to the inability to understand and accept advice given by health care workers that may result in noncompliance [5].
With respect to oral health, alcohol is among the most important risk factors for oral cancer [6,7]. Alcohol causes a change in the rate of penetration of substances from the oral environment across the mucosa and this alteration of mucosal permeability may have a role to play in carcinogenesis [1]. Evidence suggests that the increasing incidence of oral cancer, particularly in younger people, is associated with increased alcohol intake rather than tobacco use [8]. While increased alcohol consumption has also been associated with an increased risk of oral premalignant lesions, there is a paucity of data concerning the prevalence of oral mucosal lesions in persons with a history of alcohol abuse [1].
Alcoholic dependents might experience dry mouth at night, they consume higher levels of refined carbohydrate to satisfy their “munchies” and neglect both personal and professional oral health care, all of these might increase their risk of caries [5,9]. There is very limited information about the relationship between drinking and periodontitis. Only few studies examined the relationship between drinking and Probing Depth (PD) [10,11]. Thus aim of present study was to assess the impact of alcohol dependency on oral health status among alcoholics in comparison with non alcoholics. Objective of the study was to assess and compare dental caries prevalence, periodontal status, mucosal lesions and the salivary and plaque pH difference among alcohol dependents and non alcoholic subjects.
Materials and Methods
A cross-sectional clinical comparative study was conducted among alcohol dependents and non alcohol subjects visiting Narayana Medical College, Nellore district, Andhra Pradesh, India, during the month of May 2015. The study was approved by Institutional Ethical Committee of Narayana Dental College.
Subjects categorized as alcohol dependents by investigator based on American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic criteria [12]. Subjects who were willing to participate in the study and who gave written consent and with minimum of 20 natural teeth were included in the study.
Inclusion criteria for controls (non-alcoholic subjects) were Subjects who were not categorized as alcohol dependents based on American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic criteria.
Subjects with systemic diseases who were edentulous and who were using antibiotics were excluded from the study. This exclusion criteria was applied to both study and control group.
Calibration of examiners: The investigator was trained and calibrated for data recording in the Department of Public Health Dentistry, Narayana Dental College and Hospital before conducting the study. Training was carried out till the examiner produced consistent observations. Ten subjects were examined and re-examined on successive days. Intra examiner reproducibility was evaluated through percent agreement and Cohen’s kappa Statistics pertaining to Community Periodontal Index (CPI), Loss of Attachment (LOA) and dentition status, mucosal lesions (kappa value was 0.85).
Data collection: Data was collected by using interview and clinical examination. Proforma consists of two parts. The first part consists of sociodemographic details, tobacco use and DSM-5 criteria for alcohol dependence. The second part was assessment of oral health status. Oral health status of subjects was assessed using a modified WHO Proforma [13]. Dentition status index was used for assessing the prevalence of dental caries; periodontal status was assessed with the help of CPI and LOA Index, mucosal lesions were assessed using modified WHO criteria [13].
Study procedure: Investigator visited Psychiatric Department and ward daily for a period of one month (May 1st to May 31st 2015) for selecting cases (Alcoholics), by using convenience sampling a total of 106 alcoholic patients were screened among them only 76 patients met inclusion criteria. Non alcoholic (controls) subjects were recruited from the general outpatient of Narayana Medical College and Hospital. A Total 184 subjects were screened for controls by using convenience sampling method among them 76 matched controls who met the inclusion criteria were selected by matching for confounding variables like age, gender and smoking. All subjects who entered the study were explained about the study procedure.
Oral examination: Oral examination was done by using mouth mirror, WHO probe under adequate light (type III clinical examination). Alcohol dependent subjects were examined in psychiatric ward by asking them to sit on a chair. Controls and they were bought to psychiatric ward for examination. Oral examination was done for assessment of dental caries using dentition status index, CPI and LOA was used for assessment of periodontal status and the oral mucosal lesions was assessed using WHO criteria. This is followed by collection of saliva and plaque for assessment of pH.
Collection of saliva: Unstimulated whole saliva specimens were collected by instructing subjects (study group, control group) not to use any oral stimulation such as eating and drinking for 90 minutes prior to collection. Subjects were in sitting and anterior head protrusion position. Whole saliva samples were obtained by expectorating into plastic tumblers.
Plaque collection: Plaque sample was collected by Fosdick’s method [14]. Plaque was collected by using blunt probe from buccal, lingual and proximal surfaces of selected teeth (16, 21, 26, 36, 31 and 46) and was mixed in 10 ml of distilled water. The plaque pH was tested using digital pH meter.
Results
Socio demographic details: [Table/Fig-1] summarizes the demographic details, cigarette smoking and alcohol use status of the study subjects in alcohol dependent and non alcoholic groups. The mean age of the study subjects in alcohol dependent group was (34.29±5.20) and non alcoholic group was (35.89±4.92).
Socio demographic details of alcohol dependents and non alcoholic subjects.
| Demographic details | n(%) | p-value |
|---|
| Alcoholic dependents | Non alcoholic subjects |
|---|
| Age | Mean(SD) | 34.29(5.20) | 35.89(4.92) | 0.082(NS)### |
| Gender | Male | 76(50%) | 76(50%) | |
| SES | Upper | 6(7.8%) | 2(2.6%) | 0.471(NS)# |
| Upper middle | 21(27.3%) | 23(30.3%) |
| Lower middle | 38(50%) | 43(56.6%) |
| Upper lower | 11(14.5%) | 8(10.5%) |
| Smoking | Smokers | 67(88.2%) | 73(96.1%) | 0.079(NS) ## |
| Non smokers | 9(11.8%) | 3(3.9%) |
| Quantity/day | Mean(SD) | 7.18(3.22) | 6.72(2.52) | 0.016* |
Chi-square test
Fisher-exact-test
Mann-Whitney U test
p<0.05 statistically significant p>0.05 non-significant, NS
There was no statistically significant difference between alcohol dependent subjects and non alcoholic subjects with respect to their age, gender distribution, socio economic status and tobacco usage, as group matching was done in an attempt to eliminate bias for comparison.
Prevalence of dental caries among alcohol dependent subjects and non alcoholic subjects: Over all dental caries experience among alcohol dependent subjects and non-alcoholic subjects was assessed using dentition status [Table/Fig-2]. Caries experience (DMFT) was significantly high among alcohol dependents (5.92±2.89) compared to non-alcoholic subjects (4.51±2.04). When individual decayed, missed, filled components were compared among alcohol dependents and non alcoholic subjects, missing component was significantly high among alcohol dependents (1.81±2.31) compared to non alcoholic subjects (0.65±0.96). There was no significant difference observed for decayed and filled components of DMFT.
Prevalence of dental caries among alcohol dependent subjects and non-alcoholic subjects. Mann-whitney U test used.
| Dental caries | Alcoholic dependents | Non alcoholic subjects | Mann-whitney u test |
|---|
| Mean(SD) | Median (Q1-Q3) | Mean (SD) | Median (Q1-Q3) | U statistic | p-value |
|---|
| Decayed | 3.52(2.25) | 3(2-5) | 3.13(1.78) | 3(2-4) | 2602.50 | 0.28(NS) |
| Missed | 1.81(2.31) | 1(0-3) | 0.65(0.96) | 0(0-1) | 2130.50 | 0.003* |
| Filled | 0.61(1.14) | 0(0-1) | 0.71(1.13) | 0(0-1) | 2717.00 | 0.44(NS) |
| DMFT | 5.92(2.89) | 6(4-7) | 4.51(2.04) | 4(3-6) | 1990.00 | ≤0.001* |
p<0.05 statistically significant p>0.05 non-significant, NS
Periodontal status among alcohol dependents and non alcoholic subjects: Periodontal status among alcohol dependents and non alcoholic subjects was assessed using CPI and LOA index. [Table/Fig-3] shows prevalence of periodontitis was higher (89.61%) in alcohol dependent subjects compared to controls (78.67%). Pockets were significantly high among alcohol dependents (2.31±1.68) compared to non alcoholic subjects (1.39±1.22). Only bleeding without pockets was significantly high among non alcoholic subjects (1.43±1.00) compared to alcohol dependent subjects (0.83±0.80). Loss of attachment up to 4-8mm was significantly high among alcohol dependent subjects (0.96±1.61) compared to non-alcoholic subjects (0.43±0.99) [Table/Fig-4].
Over all prevalence of periodontitis among alcoholic dependents and non-alcoholic subjects.
| Periodontal status | Alcoholics (n=77) | Non alcoholics (n=75) | Total (n=152) |
|---|
| Subjects With periodontitis | 69(89.61%) | 59(78.67%) | 128(84.21%) |
| Subjects Without periodontitis | 8(10.39%) | 16(21.33%) | 24(15.79%) |
Without Periodontics = those with CPI= healthy, bleeding and caucus and LOA=0-3 mm
Periodontal status among alcohol dependents and non alcoholic subjects. Mann-whitney U test used.
| Severity of perio- dontitis | Alcoholic dependents | Non alcoholic subjects | Mann-whitney u test |
|---|
| Mean (SD) | Median (Q1-Q3) | Mean (SD) | Median (Q1-Q3) | U statistic | p-value |
|---|
| CPI | Healthy | 0(0) | 0(0-0) | 0.03 (0.16) | 0(0-0) | 2810.50 | 0.15(NS) |
| Bleeding | 0.83 (0.80) | 1(0-1) | 1.43 (1.00) | 1(1-2) | 1858.00 | <0.001* |
| Calculus | 2.81 (1.28) | 3(2-4) | 3.15 (1.00) | 3(2-4) | 2464.00 | 0.10(NS) |
| Pocket 4-5 mm | 1.99 (1.07) | 2(1-3) | 1.27 (0.90) | 1(1-2) | 1777.50 | <0.001* |
| Pocket 6 mm or more | 0.32 (0.61) | 0(0-0.5) | 0.12 (0.32) | 0(0-0) | 2494.50 | 0.032* |
| Not recorded | 0(0) | 0(0-0) | 0(0) | 0(0-0) | 2887.50 | 1.00(NS) |
| Excluded sextant | 0.05 (0.27) | 0(0-0) | 0(0) | 0(0-0) | 2775.00 | 0.08(NS) |
| LOA | 0-3 mm | 4.99 (1.40) | 6(4-6) | 5.57 (0.91) | 6(6-6) | 2206.00 | 0.003* |
| 4-5 mm | 0.74 (1.04) | 0(0-1) | 0.40 (0.83) | 0(0-0) | 2328.00 | 0.014* |
| 6-8 mm | 0.22 (0.57) | 0(0-0) | 0.03 (0.16) | 0(0-0) | 2475.00 | 0.003* |
| 9-11 mm | 0(0) | 0(0-0) | 0(0) | 0(0-0) | 2887.50 | 1.00(NS) |
| 12 mm or more | 0(0) | 0(0-0) | 0(0) | 0(0-0) | 2887.50 | 1.00(NS) |
| Not recorded | 0(0) | 0(0-0) | 0(0) | 0(0-0) | 2887.50 | 1.00(NS) |
| Excluded sextant | 0.05 (0.27) | 0(0-0) | 0(0) | 0(0-0) | 2775.00 | 0.08(NS) |
p<0.05 statistically significant
p>0.05 non-significant
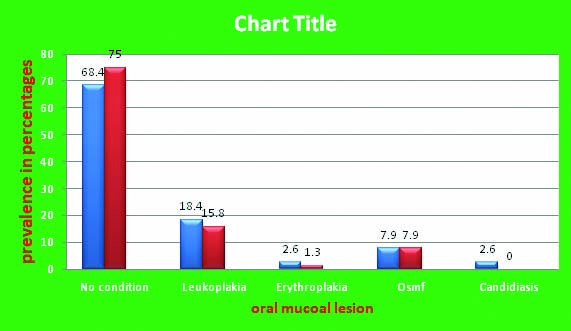
Prevalence of oral mucosal lesions: [Table/Fig-5] showing prevalence of oral mucosal lesions in alcohol dependent subjects and non alcoholic subjects. The prevalence of oral mucosal lesions was high in alcohol dependent subjects (31.5%) compared to non alcoholics (25%). Among the various types of oral mucosal lesions reported leukoplakia had a highest prevalence in alcohol dependent subjects (18.4%) followed by oral sub mucus fibrosis (7.9%), erythroplakia (2.6%) and candidiasis (2.6%).
Prevalence of oral mucous lesions among alcohol dependents and non-alcoholic subjects.
Prevalence of mucosal lesions among alcohol dependents was 31.5%
Prevalence of mucosal lesions among non alcoholic subjects was 25%
Comparison of plaque and saliva pH: [Table/Fig-6] showing mean salivary and plaque pH among alcohol dependent subjects and non alcoholic subjects. Subjects who were categorised as alcohol dependents showed a lower plaque pH (6.60±0.26) and salivary pH (6.81±0.29) compared to non alcoholic subjects (plaque pH 6.65±0.28, salivary pH 6.88±0.25) but the difference was not statistically significant.
Comparison of plaque and saliva pH among alcohol dependent and non-alcoholic subjects
| pH of plaque and saliva | Alcoholics Mean(SD) | Non alcoholics Mean(SD) | Unparied t-test |
|---|
| Plaque pH | 6.60(0.26) | 6.65(0.28) | 0.49 |
| Saliva pH | 6.81(0.29) | 6.88(0.25) | 0.47 |
*p<0.05 statistically significant p>0.05 non-significant, NS
Discussion
This cross-sectional comparative epidemiological study was aimed to assess the impact of alcohol dependency on oral health status among alcoholics in comparison with non alcoholics. Subjects categorized as alcoholics dependents based on American Psychiatric Association (DSM-5) diagnostic criteria and undergoing treatment for alcohol dependency in Psychiatric ward of Narayana Medical College were selected as cases (alcoholics). Controls (Non alcoholics) were selected from patients visiting General Hospital by matching with alcoholics to eliminate confounding bias. American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria was used for categorizing subjects as alcohol dependents. DSM-5 has nine criteria to categorize subjects under alcohol dependents; at least two among nine criteria should be satisfied by the subject with in 12 month period to be categorized as alcohol dependents.
Over all dental caries experience among alcohol dependent subjects and non alcoholic subjects was assessed using dentition status. Caries experience (DMFT) was significantly high among alcohol dependent subjects (5.92±2.89) compared to non alcoholic subjects (4.51±2.04) with significantly higher number of missing teeth were seen among alcoholics (1.81±2.31), this finding was similar to the findings of the studies conducted by Dasanyaka AP et al., Harris C et al., Sullivan EM, Hornecker E et al., and Kalpan G and Shapiro S [5,15-18]. Alcoholics had a three times higher permanent tooth loss than the national average for corresponding ages, as reported by survey of hospitalized alcoholics patients in Wyoming, USA [19]. Alcoholics and substance abusers are known to have poor oral health. Alcohol abusers experience dry mouth at night and neglect both personal and professional health care, and consume high amount of refined carbohydrates which may be the probable reason for high caries experience observed among them [5].
Alcohol dependents were at an increased risk for wide spread periodontal disease. Pockets were significantly high among alcoholic subjects compared to non alcoholic subjects. Similar to study conducted by Shimazaki Y etal, who reported that alcoholics has more than one third of teeth with Pocket depth of ≥ 4mm, as compared to non-drinkers [10]. Shizukuishi S et al., showed an association between amount of alcohol consumption and periodontal disease in Japanese factory workers [20]. Periodontal problems in alcohol dependents were primarily associated with bad oral hygiene and poor dental care [21].
Alcohol dependents were at an increased risk for clinical attachment loss. Loss of attachment was significantly high among alcohol dependents compared to non alcoholic subjects. Tezal M et al., reported a significant relationship between the frequency of alcohol drinking and clinical attachment loss (CAL) [22]. Khocht A et al., reported a comparable advanced loss of clinical periodontal attachment (≥5 mm) in alcoholics compared to community controls [23]. They reported that persistent alcohol abuse, as indicated by elevated blood gamma glutamyltranspeptidase (GGTP) levels, is significantly associated with loss of attachment. In addition, greater attachment loss in alcoholics may be a result of abnormalities in cytokine production. This cytokine is toxic to various cells and may lead to apoptosis and cell death [24]. Alcohol may affect the periodontal tissues by having adverse effect on host defense. It results in complement deficiency, defective neutrophil function (decreased adherence, motility, phagocytic activity), and increases the frequency of periodontal infections. Alcohol has a toxic effect on the liver. Prothrombin production, vitamin K activity, and clotting mechanism may be disrupted and hemorrhage may take place. Exaggerated gingival inflammation, bluish–red discolouration, and bleeding with slight provocation are commonly seen in alcoholics [22].
Prevalence of mucosal lesions was high in alcoholics (31.5%) compared to non alcoholics (25%). These findings are similar to the findings of studies conducted by Rooban T et al., and Harris CK et al., Saraswathi TR et al., [2,7,25]. Alcohol abuse is an established risk factor for oral and pharyngeal cancer as reported by O’Sullivan EM [1]. Evidence suggests that the increasing incidence of oral cancer, particularly in younger people, is associated with increased alcohol intake rather than tobacco use [8]. Tobacco consumption and alcohol drinking, synergistically influences the development of oral epithelial dysplasia as reported by Campisi G et al., [6]. Alcohol alters the mucosal permeability by changing the rate of penetration of substances from the oral environment across the mucosa and this may have a role to play in carcinogenesis [8]. These findings were supported as the aetiology of oral mucosal abnormalities is multi factorial, with life style factors such as tobacco and alcohol consumption playing a major causative role in many lesions. This pattern of combined tobacco and alcohol usage is not uncommon as unhealthy behaviours often occur in combination. Even in the present study both alcoholics and controls were smokers but quantity of smoking was more among subjects who were categorised as alcoholics.
Saliva and plaque pH of subjects who were categorised as alcoholics showed a lower plaque pH (6.60±0.26) and salivary pH (6.81±0.29) compared to non alcoholics (plaque pH 6.65±0.28, salivary pH 6.88±0.25) but the difference was not statistically significant. Study conducted by Dukic W et al., reported that pH values of both unstimulated and stimulated saliva, and were lower in the alcoholic group [26]. Chronic excess intake of acidic beverages like alcohol can directly lead to drop of pH, chronic alcohol consumption may have influence on decreased salivary flow. The differences in saliva pH values are obviously caused by the differences in flow rates, as low flow rates result in low pH values.
limitation
Small sample size was the limitation of the study, because it was a duration based study sample obtained was less. So it is recommended that further studies to be carried out on larger sample.
Conclusion
Subjects categorised as alcoholic dependent subjects had slightly lower mean plaque and salivary pH and a higher prevalence of dental caries, periodontitis and mucosal lesions compared with non alcoholic subjects.
#Chi-square test
##Fisher-exact-test
###Mann-Whitney U test
*p<0.05 statistically significant p>0.05 non-significant, NS
*p<0.05 statistically significant p>0.05 non-significant, NS
Without Periodontics = those with CPI= healthy, bleeding and caucus and LOA=0-3 mm
*p<0.05 statistically significant
p>0.05 non-significant
*p<0.05 statistically significant p>0.05 non-significant, NS