An archetypal outcome for a tooth with an immature root and necrotic pulp would be the regeneration of pulp tissue into the canal capable of bolstering the continuation of normal root development [1]. Three components contributing to the success of this procedure include, stem cells that are capable of hard tissue formation, signalling molecules for cellular stimulation, proliferation, and differentiation, and finally, a 3-dimensional physical scaffold that can fortify cell growth and differentiation [2]. The induced bleeding technique of revascularization is well documented in the literature [3-5].
PRP has been mentioned as a potentially ideal scaffold for regenerative endodontic treatment regimens because of its increased growth factor concentrations [1]. PRF is a second generation platelet concentrate which requires no biochemical handling of blood and is easy to procure [6]. The potential applications of PRF as a biologic scaffold to promote the regeneration of lost or injured dental pulp tissues and stimulate dentinogenesis was mentioned in a research study [7]. It has been mentioned that PRF is an ideal biomaterial for pulp dentin complex regeneration [8].
No study has compared the effect of PRP, PRF and induced bleeding in the revascularization of a tooth with necrotic pulp and open apex. The purpose of this study was to add knowledge to the existing literature in the field of regenerative endodontics by comparison of the effect of PRP, PRF and induced bleeding in the revascularization of a tooth with necrotic pulp and open apex. The main objectives of the study were to: (a) radiographically evaluate the continuation of root development, increase in the dentin wall thickness and narrowing of canal space, apical closure and resolution of the periapical lesion; and to (b) to clinically evaluate the response to pulp sensibility testing, percussion and palpation tests.
Materials and Methods
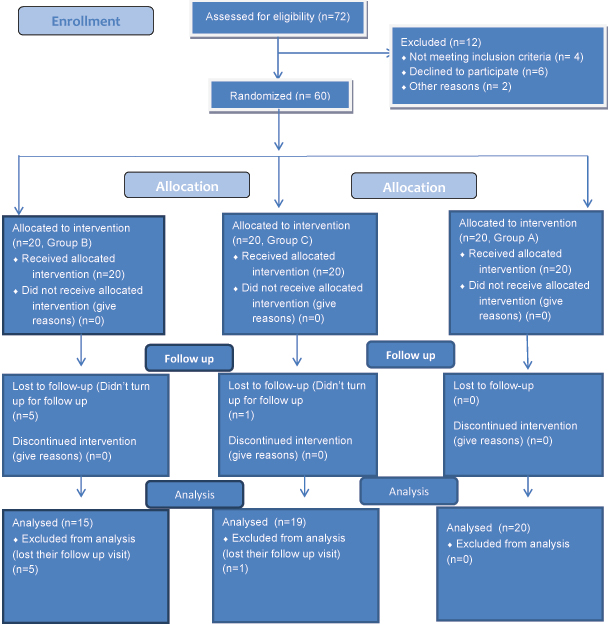
A triple blind randomized controlled trial was conducted at Government Dental College, Calicut, Kerala over a period of one year. Sixty patients with non vital, immature anterior teeth were randomly categorised into three groups in a parallel design [Table/Fig-1]. The computer generated random number table was used to assign the patients into three treatment groups. Group A patients were treated with PRF [8], Group B patients were treated with induced bleeding technique [3], Group C patients were treated with PRP [9]. The patients, the investigator and the evaluator/examiner were unaware of the allocation sequence. Informed consent was obtained from the patients. The study proposal was approved by the Institutional Ethics Committee. Subjects were initially assessed for eligibility at a baseline visit. Age of the patients ranged from 6 to 28 years with 32 males and 28 females. Patients were followed up at 3rd, 6th, 9th and 12th months intervals. At 3rd and 9th month clinical examination alone was performed. At 6th month, only the periapical status (PAI score) was recorded. Since one cannot appreciate much radiographic changes within a short span of three months, the data were not collected at 3rd and 9th month.
Consort 2010 flow diagram.
Inclusion Criteria
Clinical criteria included patients between 6-28 years of age who were healthy and free of any systemic diseases. Patients with necrotic immature permanent teeth, secondary to trauma and/ or caries and patients who responded negatively to allergic patch test (triple antibiotic paste) were included in the study. Preoperative radiograph showing incomplete root formation, wide apical foramen – apex >/= 1 mm and thin dentinal walls were the radiographic criteria.
Exclusion Criteria
Patients who were allergic to any drugs or with systemic illness, grossly decayed or fractured teeth that required post and core as final restorations, presence of draining sinus and presence of periodontal pockets were the exclusion criteria clinically. Radiographically, apical foramen less than 1 mm, presence of periapical radiolucency more than 10 mm, presence of external or internal root resorption as well as patients with a history of major surgeries like cardiac, kidney transplantation, haemodialysis were excluded from the study.
Sample Size Determination
Based on previous studies [1,10-12] sample size estimation was done and a minimum of 18 subjects were required in each group. Hence we rounded the sample size to be 20.
Treatment Methods
General Steps: The tooth was isolated under rubber dam and access cavity was prepared with a round diamond bur and long straight fissure bur. The canal was minimally instrumented and was copiously irrigated with 5.25% sodium hypochlorite and dried with sterile paper points. The triple antibiotic paste (containing metronidazole-400 mg, ciprofloxacin-200 mg, and minocycline-100 mg in the ratio 1:1:1 by weight) was prepared in a creamy consistency using propylene glycol and macrogol ointment taken in 1:1 ratio by weight [13] and was placed inside the canal up to a maximum of 2 mg. The access cavity was then closed with cotton pellets and intermediate restorative material. The patient was recalled after three weeks. In the second sitting, the tooth was checked for any discoloration, abscess, mobility, or pain on percussion and after disinfecting the mouth with betadine solution, the tooth was re-accessed under rubber dam isolation. The antibiotic paste was removed using sterile saline solution. No instrumentation of the canal space was performed and the canal space was dried using sterile paper points. Following the general step, the patients were randomly categorised into three groups with 20 patients in each group as mentioned earlier.
Radiographic Assessment: Standardised reproducible radiographs (IOPAR) using a standardised paralleling cone technique with positioning aids were taken at baseline, 3rd, 6th, 9th and 12th months visits. The periapical status assessment was assessed using the PAI [Table/Fig-2] [14]. All radiographs were evaluated by a single examiner who was masked to the treatment group to which a patient was assigned and also to whether the radiograph was taken at baseline or re-evaluation. The method of viewing the radiographs was standardised. Films were examined in a dark room by using an illuminated viewer box with magnification (3.5 X) while mounted in a cardboard slit to block off ambient light emanating from the viewer. All radiographs were scanned and the images were stored in a computer for assessment.
Periapical Index (Orstavik D et al.,) [14].
| Score | Criteria |
|---|
| 1 | Normal periapical structures |
| 2 | Small changes in bone structure |
| 3 | Changes in bone structure with some mineral loss |
| 4 | Periodontitis with well defined radiolucent area |
| 5 | Severe periodontitis with exacerbating features |
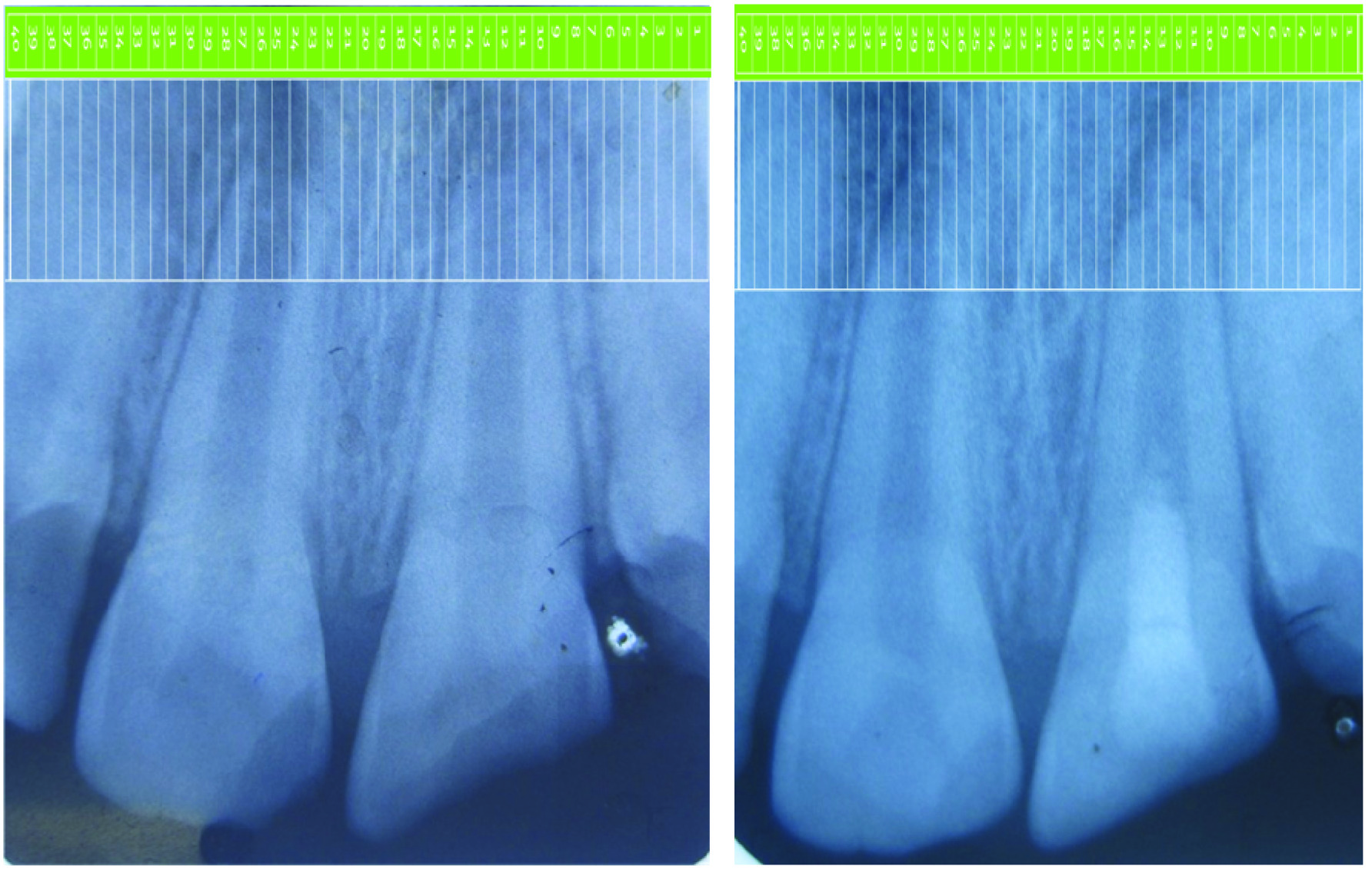
Root lengthening was measured by superimposing the Schei’s ruler over the radiographic image in such a way that the long axis of the tooth and the ruler were parallel to each other. The changes in root length were determined by comparing the number of segments of Schei’s ruler from the incisal edge to the root apex (same tooth) of the preoperative and 12th month follow up radiograph [Table/Fig-3a,b]. Similarly, lateral wall thickening was measured by superimposing the Schei’s ruler perpendicular to the long axis of the tooth. The changes in the lateral wall thickening was determined by comparing the number of segments of Schei’s ruler from the lateral surfaces of the root to the root canal wall (same tooth) [Table/Fig-4a,b] [15]. The outcome was categorised into satisfactory and good if there was increase in a single increment and two or more increments respectively. This method effectively compensates for any radiographic shortening or lengthening errors that might occur despite the best efforts to standardise the radiographic technique [15].
Determination of increase in the root length using a Schei’s ruler.
a) – preoperative radiograph of tooth no. 8 showing blunt and open apex.
b) – 12th month follow up radiograph showing increase in the length of the root with closure of the apex. (All Images: Left to right)
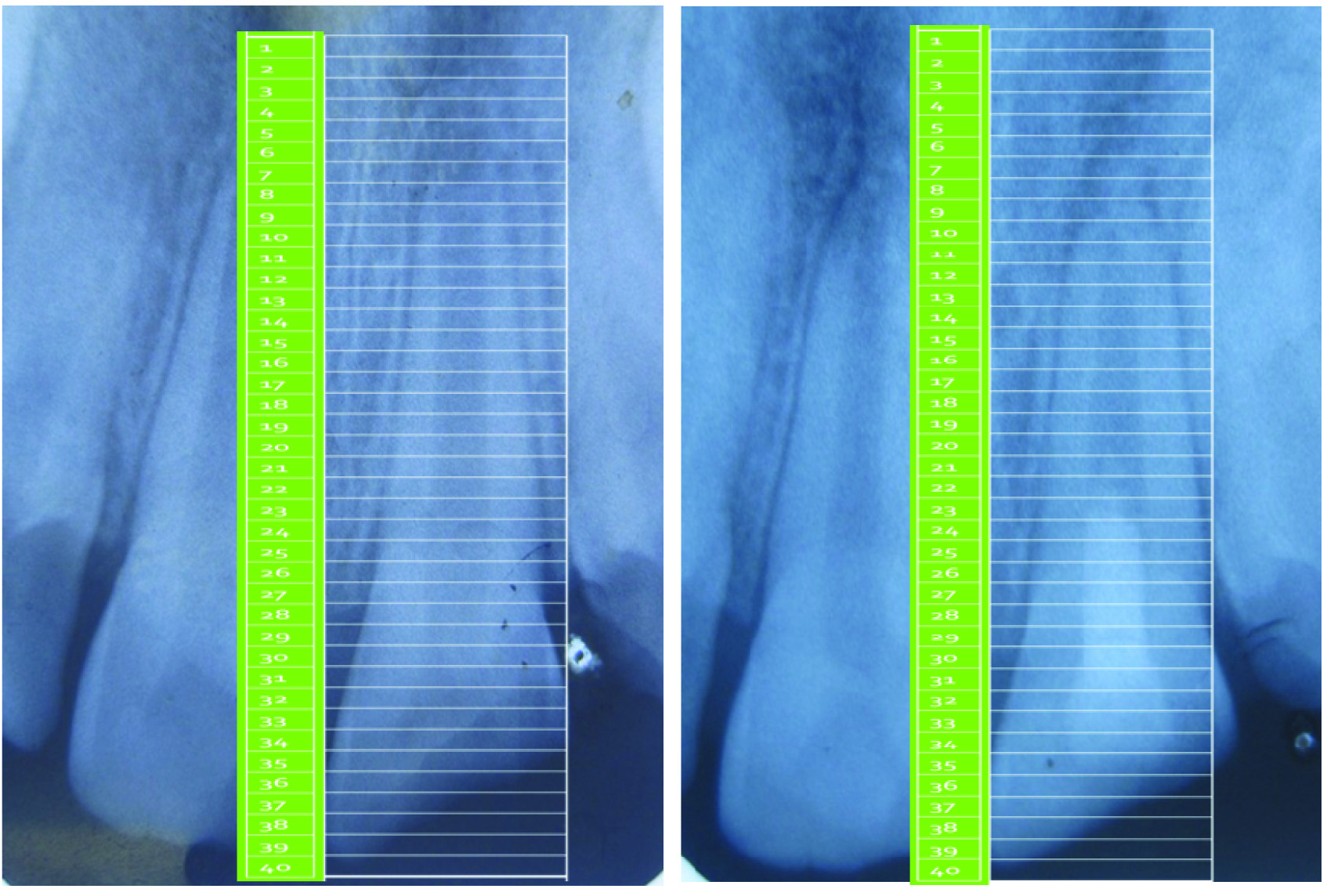
Determination of increase in the lateral wall thickening using a Schei’s ruler. a) – Preoperative radiograph of tooth no. 8 showing thin dentinal walls with an open apex; b) – 12th month follow up radiograph showing increase in the lateral wall thickness with closure of apex.
Five types of apical responses are observed in a necrotic immature tooth treated by revascularization procedure. In this study, a system proposed by Chen and Chen was used to evaluate the apical responses of teeth in all the three groups [Table/Fig-5] [4].
Types of apical response (Chen and Chen) [4]
| Types | Radiographic Picture |
|---|
| Type 1 | Increased thickening of the canal walls and continued root maturation |
| Type 2 | No significant continuation of root development with root apex becoming blunt and closed |
| Type 3 | Continued root development with the apical foramen remaining open |
| Type 4 | Severe calcification (Obliteration) of the canal space |
| Type 5 | A hard tissue barrier formed in the canal between the coronal MTA plug and the root apex |
Determination of the Outcome of the Periapical Status
Treatment success was assessed using two outcome measures.
Strict criteria of success [16] (absence of pain, inflammation or swelling and conventional radiograph showing complete healing and presence of a normal periodontal ligament space);
Loose criteria of success [16] {absence of pain, inflammation or swelling and conventional radiograph showing complete healing and presence of a normal periodontal ligament space or incomplete healing (if there was reduction in size of the lesion without return to normal periodontal ligament space width)}.
The tooth with a PAI score of 1 or 2 was considered successful under strict criteria of success and tooth with a PAI score of either 3 or 4 or 5 was considered to be a failure. A tooth with PAI score of 1 or 2 or 3 was considered successful under the loose criteria of success, whereas a tooth with a PAI score of 4 or 5 was considered to be a failure.
If a tooth had received root canal treatment due to endodontic reasons, the treatment was considered failed. Also, a tooth with a PAI score of 4 or 5 was considered to be a failure even if the tooth was clinically normal and asymptomatic.
The statistical analysis was performed using commercially available software (SPSS 16, SPSS Inc., Chicago, IL, USA). The primary outcome variable was measured using PAI index, clinical parameters and other radiographic parameters. The Chi-square test was used to interpret the data among the three groups at the end of 12 months for the variables root lengthening and lateral wall thickness. ANOVA test was performed to compare the mean of the PAI scores of the three groups at preoperative stage and 12 months. If statistically significant, Bonferroni test was done to compare the outcome among the three groups. The significant level was set at p<0.05. Kappa agreement was used to see whether the clinical criteria of success (asymptomatic) were in agreement with radiographic criteria i.e., strict and loose.
Results
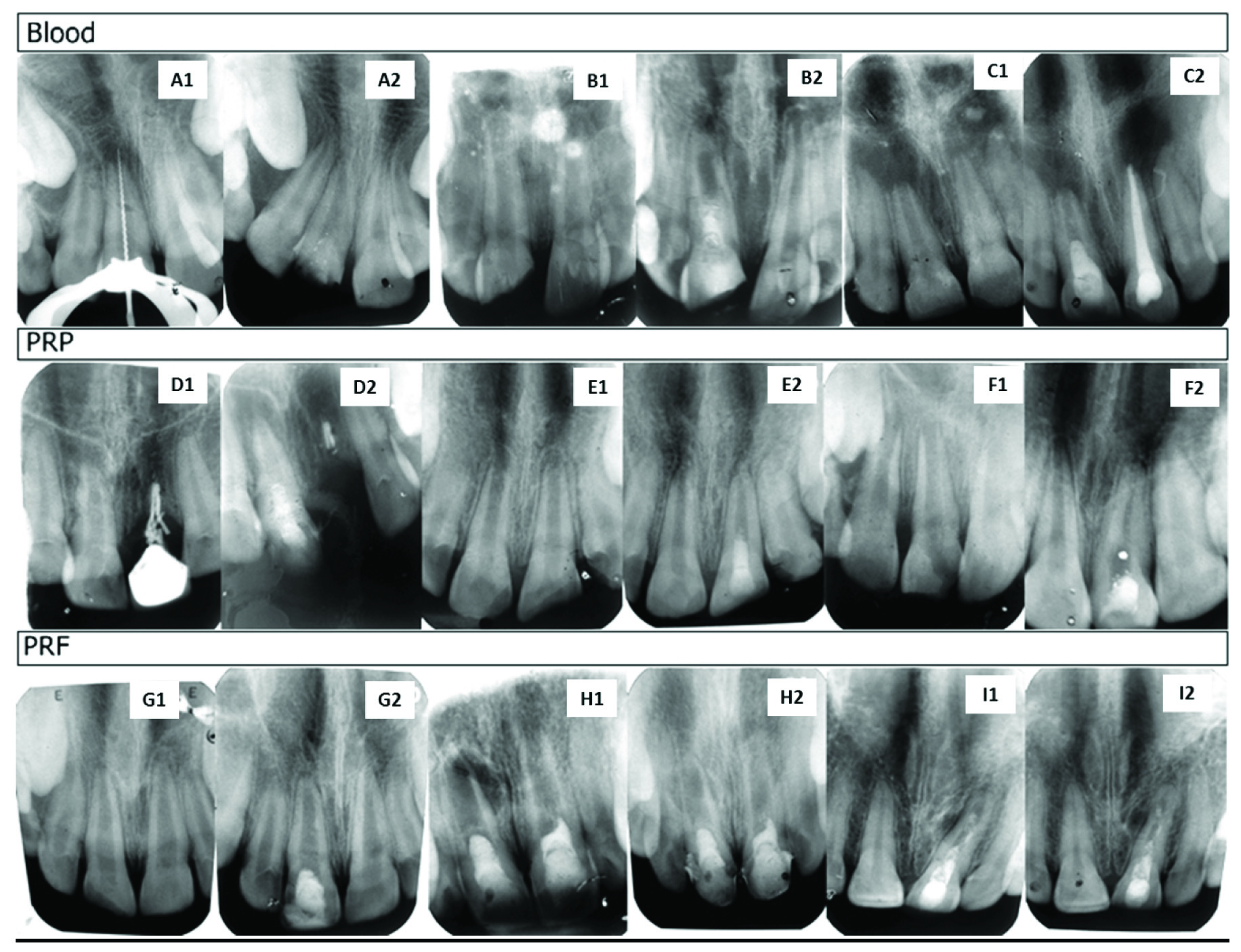
The preoperative and postoperative radiographs of all the groups are given in a composite image [Table/Fig-6]. Out of 60 patients in our study six patients (five from Group B and one from Group C) were excluded from the study as they did not present themselves for the regular follow up visits.
Induced Bleeding Group (Blood): A1 – Tooth no. 8 showing a file extending beyond the confines of the root canal due to an open apex; A2 – At the end of 12 months tooth no. 8 shows a proper closure of the apex with normal periodontal ligament lining. (Type 1 apical response). B1 – Tooth no. 8 shows thin dentinal walls laterally and apically with a wide open apex; B2 – After 12 months, the thickness of the dentinal wall is increased laterally and apically. (Type 1 apical response) C1 – Tooth no.8 shows a wide open apex greater than 1 mm with thin dentinal walls laterally; C2 – After 12 months, there is continued root development with apical foramen remaining open. (Type 3 apical response).
PRP Group: D1 – Tooth no. 8 showing wide open apex with thin dentinal walls; D2 – At the end of 12 months there is near closure of apex with root lengthening apically. (Type 3 apical response). E1 – Tooth no.9 shows an open apex greater than 2 mm with thin lateral and apical dentinal walls; E2 – After 12 months there is complete closure of apex suggesting apexogenesis with root maturation. (Type 1 apical response). F1 – Tooth no. 9 shows an open apex with arrested root growth due to trauma; F2 – At the end of 12 months there is almost complete closure of the apex with root maturation. (Type 3 apical response).
PRF Group: G1 – Tooth no. 8 shows an Ellis class III fracture with an open apex; G2 – At the end of 12 months there is near closure of the apex with root thickening and lengthening. (Type 3 apical response). H1 – shows the immediate postoperative radiograph of tooth no. 9 after the condensation of PRF into the canal with open apex and thin dentinal walls; H2 – At the end of 12 months there is just a blunt closure of the apex with not much root maturation. (Type 2 apical response).
I1 – Tooth no. 9 shows incompletely matured root with an open apex; I2 – After 12 months there is increased thickening of the canal walls and continued root maturation. (Type 1 apical response).
Clinical Criteria of Success
Clinical evaluation showed no significant difference between the groups. Clinically none of the patients were symptomatic. A total of 18 patients in Group A, 15 patients in Group B and 19 patients in Group C showed a successful clinical outcome. Two patients in Group A showed a failure outcome as their PAI score was 4 even though they were clinically asymptomatic [Table/Fig-7].
The clinical and radiographic success in all the three groups. Clinical criteria of success - χ2 value = 3.531, p-value = 0.171 Radiographic success - χ2 value = 7.630, p-value = 0.106 Chi-square test was used as the test of significance.
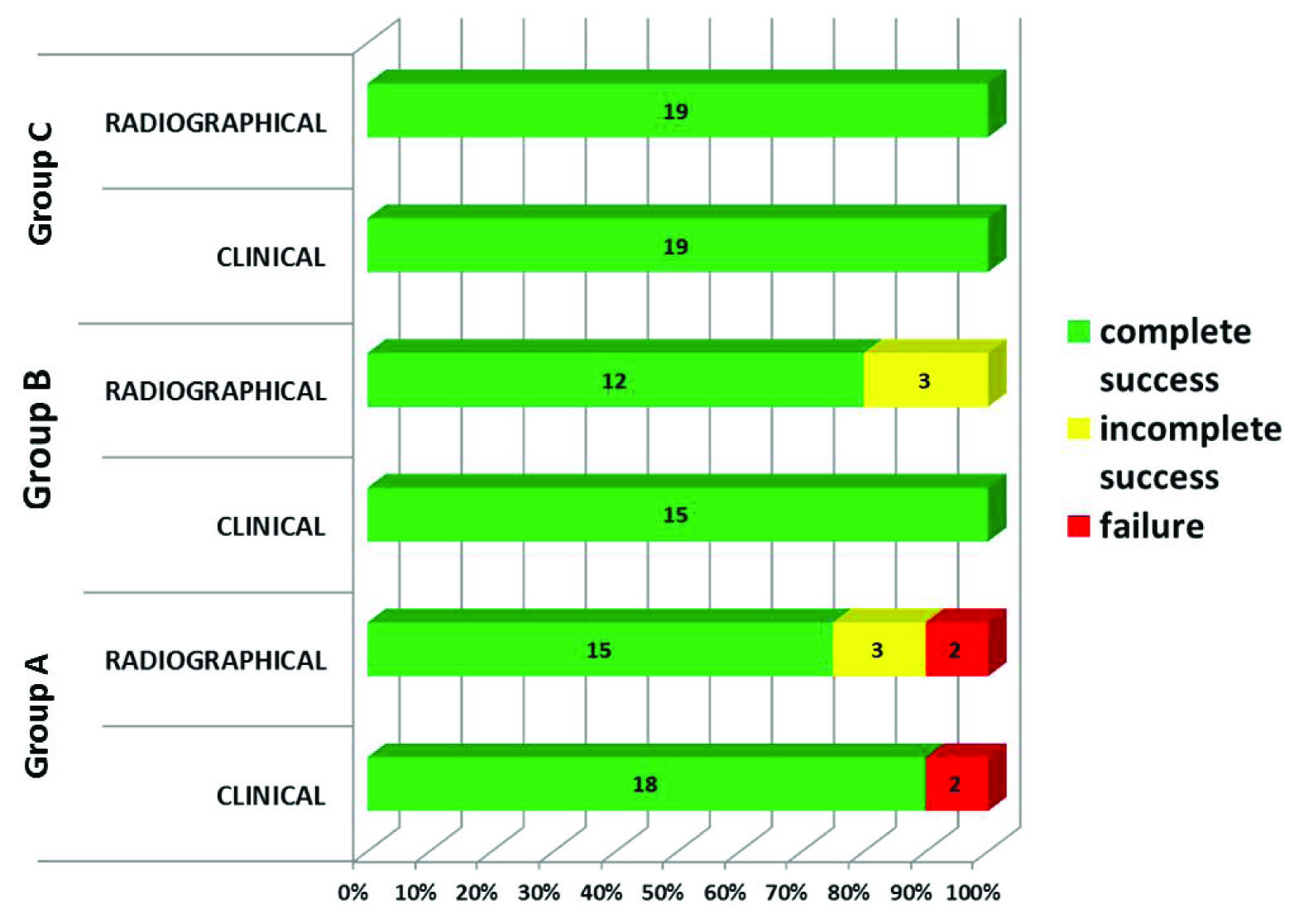
Success Assessment by Radiographic Means
Success criteria by radiographic means had no significant difference between the groups. A total of 15 patients in Group A, 12 patients in Group B and 19 patients in Group C showed complete healing. Also, three patients in Group A and three patients in Group B showed an incomplete healing (PAI score=3) and two patients in Group A were grouped as failure group because their PAI score was 4 [Table/Fig-7].
Success criteria were divided into strict and loose [16]. Both the criteria showed no significant differences between the groups.
Strict Criteria of Success
There was no statistical difference among the groups when the success was defined under strict criterion. A total of 15 patients from Group A, 12 patients from Group B and 19 patients from Group C were grouped under success category when the strict criteria of success were applied. Also, five patients from Group A and three patients from Group B were grouped under failure category as their PAI score was at or above 3 [Table/Fig-8].
The radiographic success in all the three groups. Chi-square test was used to analyse the statistics in strict criteria and loose criteria of success.
Strict criteria = χ2 value = 5.268, p-value = 0.072 Loose criteria = χ2 value = 3.531, p-value = 0.171
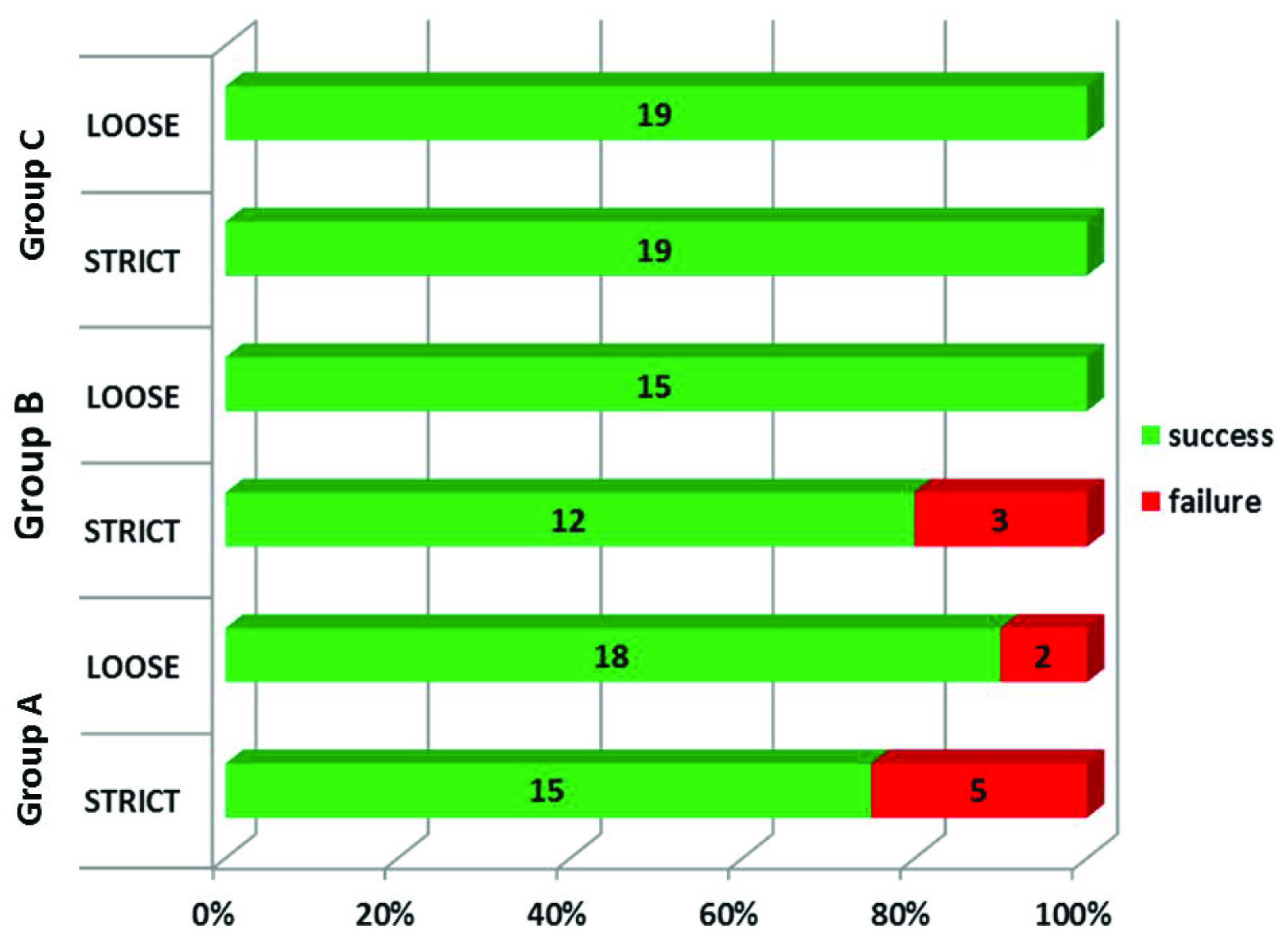
Loose Criteria of Success
The success in the loose criteria had 100% Kappa agreement with clinical criteria of success. A total of 18 patients from Group A, 15 patients from Group B and 19 patients from Group C were categorised into success group when the loose criteria of success were applied. Also two patients in the Group A were categorised as failure as their PAI score was 4, even-though they were clinically asymptomatic [Table/Fig-8].
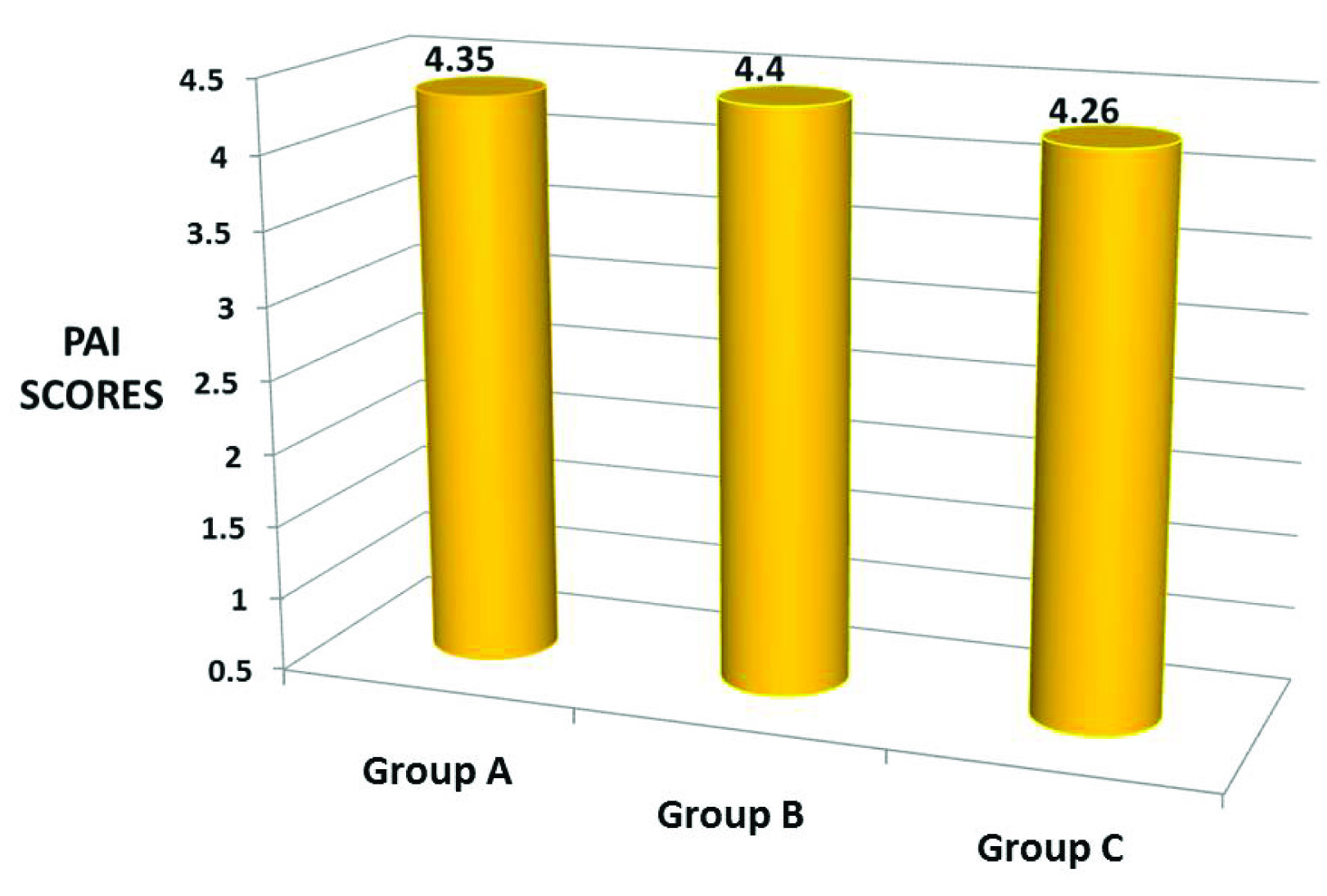
Preoperative Periapical Index Scores
Patients with a PAI score of 4 or 5 were selected for this study. The mean PAI scores of Group A, Group B and Group C were 4.35, 4.4 and 4.26 respectively [Table/Fig-9].
The preoperative mean PAI scores of all the three groups
Comparison of Periapical Healing at 6th and 12th months
Significant change occurred in the p-value (0.015) favouring Group C at the end of one year. The PAI scores of all three groups at 6th and 12th month has been mentioned in [Table/Fig-10].
Comparison of periapical healing at 6th and 12th month using ANOVA and BONFERRONI TEST
| n | 6th Month Mean±SD | 12th month mean±SD |
|---|
| GROUP A | 20 | 3.20±0.410 a,c | 1.85±1.040 a |
| GROUP B | 15 | 2.93±0.458a, | 2.07±0.594a,b |
| GROUP C | 19 | 2.74±0.562a,b | 1.32±0.478 a,c |
| Total | 54 | 2.96±0.513 | 1.72±0.811 |
| F-value | | 4.549 | 4.52 |
| p-value | | 0.015 | 0.016 |
Same alphabets denote no significant difference. Different alphabets denote significant difference.
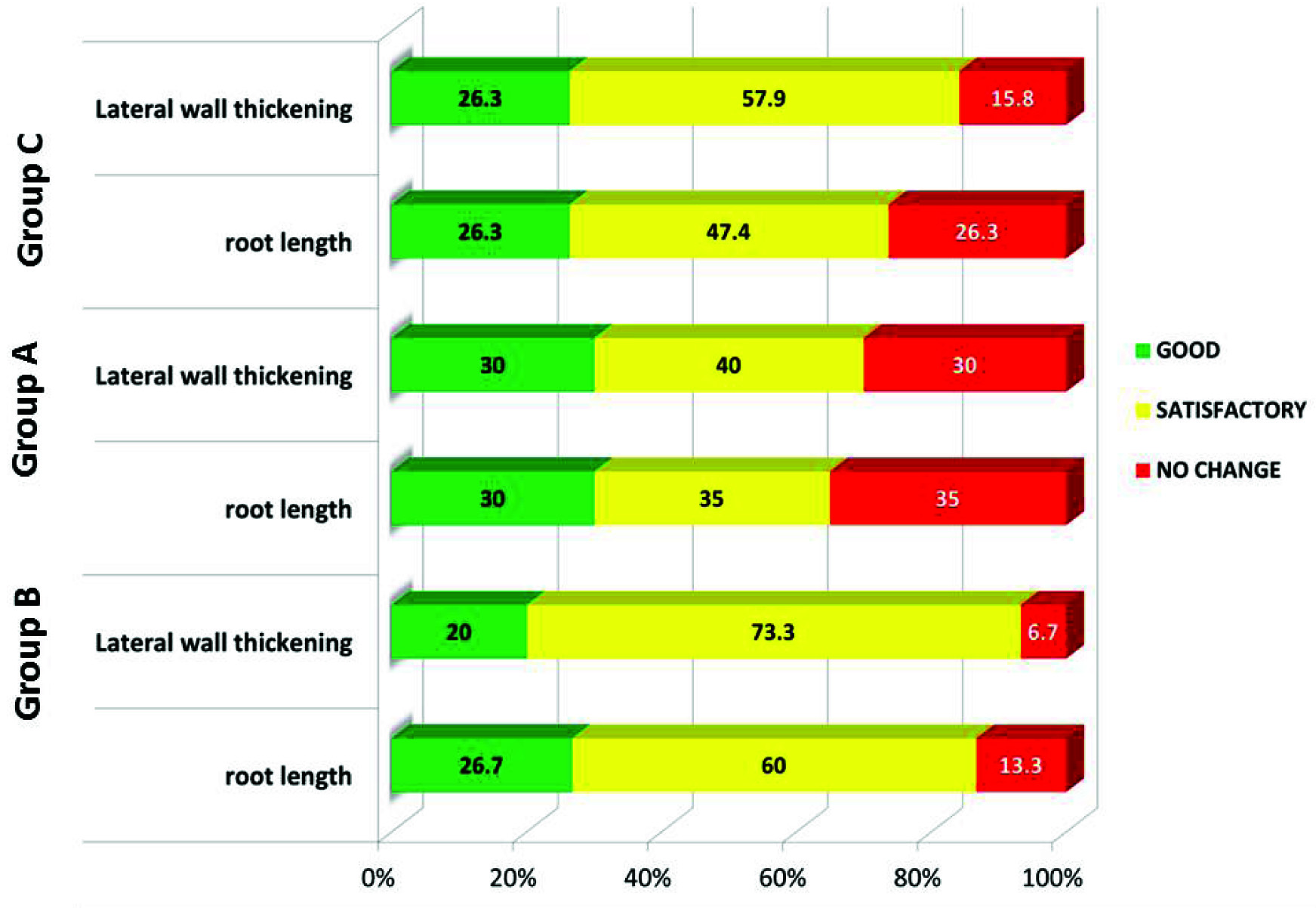
Root Lengthening and Lateral Wall Thickness at the End of 12 months
According to Chi-square test, there was no significant difference among the three groups at the end of 12 months with respect to root lengthening and lateral wall thickness. Preoperative radiographs were used as the baseline data, from which the changes in root length and thickness were assessed [Table/Fig-11].
The increase in the root length and lateral wall thickness at the end of 12 months.
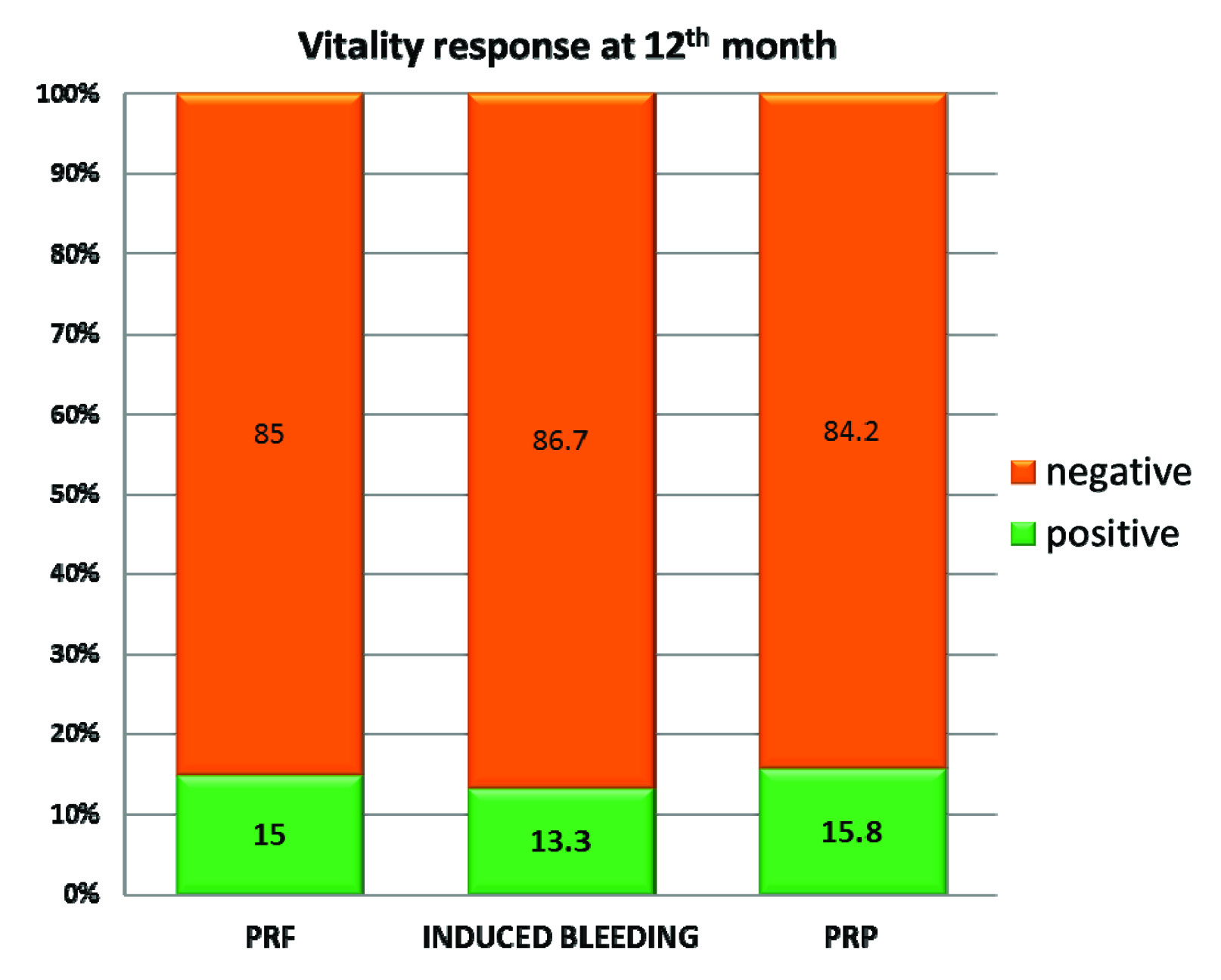
Response to Vitality Testing at 12 months
When the vitality response of the patients in all the three groups were plotted in a graph, a gradual shift in the percentage of response from negative to positive was observed during follow up period. A total of 15% of patients in Group A, 13.30% of patients in Group B and 15.8% of patients in Group C showed a positive response to vitality testing after 12 months [Table/Fig-12]. Apical response at the end of 12 months is shown in [Table/Fig-13].
The vitality responses of all the three groups at 12th month.
Apical foramen responses at the end of 12 months.
| Response | GROUP A | GROUP B | GROUP C |
|---|
| N | % | N | % | N | % |
|---|
| Type 1 | 2 | 10% | 2 | 13.3% | 2 | 10.5% |
| Type 2 | 2 | 10% | 3 | 20% | 2 | 10.5% |
| Type 3 | 10 | 50% | 8 | 53.3% | 12 | 63.2% |
| Type 4 | 1 | 5% | 0 | 0% | 0 | 0% |
| Type 5 | 1 | 5% | 1 | 6.7% | 0 | 0% |
| No Change | 4 | 20% | 1 | 6.7% | 3 | 15.8% |
| Total | 20 | 100% | 15 | 100% | 19 | 100% |
Discussion
The ability of the apical pulp tissue to survive under unfavourable necrotic condition and proliferate under favourable condition is the principle behind revascularization [8]. Three key requirements for a successful revascularization are: (a) Root canal disinfection; (b) matrix inside the canal for growth of tissue; and (c) a tight seal access filling [5]. An ideal scaffold should allow cell binding and cell localisation, supply growth factors, and should be biodegradable in nature. Though blood clot is a good scaffold [17,18], it’s a poor source of growth factors. The concentration of platelet in PRP is more than 1 million/ml, which is five times as higher than that of normal platelet count [19]. It is a concentrated suspension of different growth factors like platelet derived growth factor, transforming growth factor b, insulin like growth factor, vascular endothelial growth factor, epidermal growth factor, and epithelial cell growth factor and has been mentioned as an ideal scaffold for regenerative endodontic procedures [1].
PRF is an ideal scaffolding material for regeneration because, it is easy to prepare, requires no biochemical handling of blood and hence it is purely autologous in nature unlike PRP which requires biochemical processing of blood [8].
Though there was no significant difference among the three groups with respect to periapical healing at the end of three months, but there was difference at the end of six months (p-value=0.015) favouring Group C over other groups [Table/Fig-10]. With this, we speculate that PRP gives better results with respect to periapical wound healing compared to PRF and induced bleeding group in a short span of time. Again at the end of 12 months follow up, Group C showed a better periapical healing compared to other groups [Table/Fig-10]. Hence, based on the results obtained in our study we suggest that PRP is better than PRF and induced bleeding with respect to periapical wound healing when used in the regenerative endodontic procedures. This probably could have occurred because of the liquid consistency of PRP that enabled it to reach the periapex without any impedance [8], unlike PRF, which has gel like consistency, thereby delivering maximum amount of growth factors to hasten the wound healing process. The results of our study are in contrast with the study done by Narang I et al., in which PRF was mentioned to give excellent results on grounds of periapical healing [20] whereas the results are comparable with respect to root lengthening and lateral wall thickening.
The three groups were comparable on the grounds of lateral wall thickening, root lengthening, and response to vitality testing.
On analysing the apical foramen response of the three groups, it was found that Type 3 response [Table/Fig-5], G2) was the most common response in all the three groups and Type 4 and Type 5 being the least common. Hence the most common outcome of revascularization procedure would be the continuation of normal root development with apical foramen remaining open. Since the present study is the result of 12 months follow up, we can assume that the apical foramen might close during the course of time.
When MTA was placed slightly below the level of CEJ, a positive response was obtained to cold test and Electric Pulp Test (EPT) in our study. Since MTA limits the growth of new tissue ahead of it, the placement of MTA and its thickness determines the responsiveness of the tooth to pulp sensibility testing [1]. Hence, if a tooth has matured (radiographically) after the revascularization procedure, it means there is cementum like hard tissue in the root canal with functional cementoblast like cells [3,21]. Such a tooth is considered vital even if it responds negatively to pulp sensibility tests. Since MTA is hydrophilic in nature and needs moisture to set [1], it became the material of choice in our study as there is potential for moisture contamination in the clinical setting, and also MTA by itself provides signalling molecules for the growth of the stem cells [8].
Limitation
Since five patients from Group B did not present themselves for the follow up, the results of the study could have had changes with respect to postoperative healing and apical foramen changes. Placement of MTA was slightly variable because of the access filling material which could have changed the position of MTA near CEJ. The histological changes in the root canal are not addressed in this study, which can precisely state the nature of tissues formed in response to various revascularization techniques.
Conclusion
Though PRP gives results in a short period of time compared to other groups, it requires drawing 10-15 ml blood from the patient and needs biochemical processing. On the other hand, induced bleeding technique, though it gives delayed results compared to PRP, requires no drawing of blood from the patient and no biochemical handling of blood and hence is a less cumbersome procedure. On analysing the pros and cons of the techniques performed, it is wise to establish induced bleeding technique as the standard endodontic procedure for revascularization of a non vital immature permanent tooth.