APN is defined as a bacterial or fungal infection of the renal parenchyma and collecting system. The diagnosis is based on a combination of clinical and laboratory findings. Clinical features include increased urinary frequency, dysuria, flank pain and a high-grade fever (>38.5°C) with rigors. Laboratory findings include pyuria, white cell casts, and a positive urine culture. APN occurs as a result of bacterial invasion of the renal parenchyma from ascending infection from the lower urinary tract. Haematogenous spread to the kidneys occurs less commonly. APN is subdivided into uncomplicated and complicated. Complicated PN is associated with an abnormal urinary tract, obstruction, stones, immunocompromised state, diabetes, pregnancy. The clinical spectrum of acute PN ranges from mild illness to pyonephrosis and emphysematous PN with a fulminant course [1].
Patients with mild symptoms of APN can be managed in an outpatient setting. But, those presenting with life-threatening complications like shock, septicaemia and multi-organ failure require hospitalization. Mortality due to APN varies from 1% to 12% [2].
The British Medical Research Council Bacteriuria Committee defined APN as a clinical syndrome of flank pain, costovertebral tenderness, fever and laboratory findings of renal infection including leucocytosis, pyuria, haematuria, bacteriuria, positive urine culture and rarely bacteraemia [3].
Pathologically, APN is defined as suppurative inflammation of the renal parenchyma and pyelocalyceal system distributed along one or more medullary rays supporting an ascending route of infection [4]. Radiologically, on Contrast Enhanced Computed Tomography (CECT) scans, it is seen as hypoenhancing regions with or without renal swelling and may be focal or diffused. APN includes all acute infection related to parenchymal abnormalities without abscess diagnosed radiologically [5].
Severity of PN cannot be predicted with clinical or laboratorial parameters alone. Radiological images such as USG and CT are also necessary to know the nature, extent and severity of disease and to plan intervention if required. CT abdomen will help detect calculi, emphysematous change, parenchymal calcification, obstruction and inflammatory masses. Very few studies are available to correlate the clinical severity of PN with radiological severity of the disease [2,3,6].
Hence, this study was done to compare clinical and biochemical parameters with radiological findings by USG and CT among patients diagnosed to have PN.
Materials and Methods
Medical records of all patients diagnosed with APN admitted at Institute of Nephrourology Hospital Bengaluru, Karnataka, India, from January 2016 to December 2016 were reviewed retrospectively. Patients demographic details, medical history, clinical, biochemical and radiological imaging reports were reviewed.
All the patients diagnosed to have PN based on clinical and/or radiological findings were included in this study.
In this study, the diagnosis of PN was based on clinical and radiological criteria as explained below [2].
Clinical criteria were the presence of classical triad of PN i.e., fever with chills and rigor; presence of flank pain and pyuria, defined as greater than 10 white blood cells per high-power field of centrifuged urine sample.
Radiological diagnosis of PN was made when USG/CT abdomen showed evidence of infection of renal parenchyma, in the form of bulky kidney, compression of renal sinus, perinephric fat stranding, abscess and emphysematous changes.
EPN is necrotising infection with presence of gas in the renal parenchyma, collecting system or perinephric tissue. Based on CT findings, EPN can be classified as: Class 1: Gas in the collecting system, Class 2: Gas in the renal parenchyma without extension to the extrarenal space, Class 3A: Extension of gas or abscess to the perinephric space, Class 3B: Extension of gas or abscess to the pararenal space and Class 4: Bilateral EPN or solitary kidney with EPN [7].
Hypotension is defined as a systolic blood pressure of <100 mmHg.
Acute renal failure was defined as 25% decrease in Glomerular Filtration Rate (GFR) from baseline, according to Acute Dialysis Quality Initiative (ADQI) group.
GFR is calculated based on the Modification of Diet in Renal Disease (MDRD) study equation.
Statistical analysis
Statistical analysis was performed with SPSS Version 15.0. Descriptive studies were performed for the cohort. Fischer Exact test were performed for significance. The p value of <0.05 was considered to be significant.
Results
All patient records fulfilling the inclusion criteria were included for analysis. The study includes 100 patient records. Mean age of patient were 48.7 years (range 15 – 85), majority of them were more than 40 years (70) with female (62) preponderance. Among them, three females were in 2nd trimester of their pregnancy. Classical triad of PN was present in 87 of patients. Renal function was normal in 21 patients. Acute kidney injury secondary to PN was present in 47 patients. PN was present in 32 chronic kidney disease patients. Risk factors and comorbidities are represented in [Table/Fig-1]. Diabetes (69) was the most common comorbid condition. Recurrent PN was documented in 16 patients. History of renal calculi was noted in 9 patients.
Demographics and comorbidities of patients.
| Parameter | Number |
|---|
| Age (years) | <18 | 03 |
| 18-30 | 09 |
| 31-40 | 18 |
| 41-50 | 23 |
| 51-60 | 22 |
| >60 | 25 |
| Sex | Male | 38 |
| Female | 62 |
| Triad of PN | | 87 |
| Septic shock | | 07 |
| Diabetes mellitus | | 69 |
| pregnancy | | 03 |
| Renal calculi | | 09 |
| Benign prostatic hyperplasia | | 01 |
| Recurrent PN | | 16 |
| Renal function | Normal | 21 |
| AKI | 47 |
| CKD | 32 |
(Triad of PN-Fever, flank pain, dysuria. DM-Diabetes Mellitus, HTN-Hypertension, AKI-Acute kidney injury, CKD-Chronic kidney disease, BPH-Benign prostatic hyperplasia.)
Biochemical Findings
Lecucocytosis was present in 68 patients and thrombocytopenia was found in 16 patients. Pyuria was present in 87 patients. Microscopic hematuria was present in 21 patients. Positive urine culture was found only in 24 patients. Majority of them had E coli infection, followed by Enterococcus, Klebsiella and Candida. None of the patient had positive blood culture. [Table/Fig-2]
| Urine microscopy | Pus cell >10/hpf | 87 |
| Red blood cell >5/hpf | 21 |
| Haemoglobin | >10 | 96 |
| <10 | 4 |
| Total WBC count | Normal | 32 |
| Increased | 68 |
| Platelets | Normal | 84 |
| Decreased | 16 |
| Serum | Normal | 21 |
| Increased | 79 |
| Urine culture | No growth | 76 |
| Positive | 24 |
| Blood culture | No growth | 0 |
(WBC - white blood cell, hpf-high power field)
Imaging Parameters
Renal USG [Table/Figure 3] was performed at the time of admission among all patients. It was suggestive of APN in 66 cases, unilateral PN was seen in 40 and bilateral in 26 patients. Other USG findings include - 17 with dilated pelvicalyceal system, 11 had increased echogenicity, three had renal calculi, two showed cyst and one had benign prostatic hypertrophy.
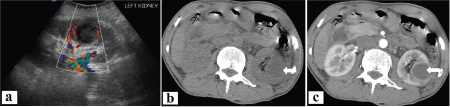
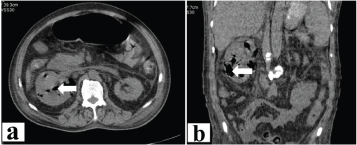
CT abdomen reports were available for 74 patients, it revealed unilateral PN in 33 and bilateral in 30 patients [Table/Fig-3]. Three patients were diagnosed to have renal abscess [Table/Fig-4]. Evidence of emphysematous PN was present four of patients [Table/Fig-5]. Dilated pelvicalyceal system noted in three patients and renal calculi was noted in 15 patients.
| Parameters | | Number |
|---|
| USG abdomen | Unilateral PN | 40 |
| Bilateral PN | 26 |
| CT abdomen | Unilateral PN | 33 |
| Bilateral PN | 30 |
| Abscess | 3 |
| Emphysematous PN | 4 |
(CT-computed tomography, PN-Pyelonephritis)
Renal abscess. a) USG image of left kidney showing a well-definedhypoechoic lesion with internal debris in mid-lower pole, not taking vascularity on color Dop-pler study; b & c) Plain and contrast enhanced CT images of the same patient showing a well-defined rim enhancing hypodense lesion in the left kidney.
Emphysematous pyelonephritis. a) Axial and b) Coronal, Plain CT images show enlarged right kidney with multiple pockets of air seen in both renal calyces and parenchyma. Perinephric fat stranding noted.
USG findings of PN were significantly associated with triad of PN symptoms, and those who had PN for the first time [Table/Fig-6, 7]. CT was helpful in detecting PN with complications, but there was no significant association between CT and clinical and biochemical parameters like duration of fever, leucocytosis, pyuria, septic shock and renal impairment.
Comparison of ultrasound (USG) findings with triad of pylenophritis I (PN).
| USG findings | Dysuria | Fever, flank pain, dysuria | Fever | Flank pain | Total | Fisher’s Exact Test |
|---|
| USG normal | 2 | 6 | 0 | 3 | 11 | 0.003 |
| USG bulky kidney, PNS + | 0 | 61 | 1 | 4 | 66 |
| USG dialated PCS | 0 | 16 | 0 | 1 | 17 |
| USG calculi | 0 | 2 | 1 | 0 | 3 |
| USG cyst | 1 | 1 | 0 | 0 | 2 |
| USG BPH | 0 | 1 | 0 | 0 | 1 |
| Total | 3 | 87 | 2 | 8 | 100 |
(PNS - perinephric fat standing; PCS -pelvicalyceal system; BPH - benign prostatic hyperplasia).
Comparison of ultrasound (USG) findings with history pylenophritis I (PN).
| USG | Current PN | Recurrent PN | Total | Fisher’s exact Test |
|---|
| USG normal | 6 | 5 | 11 | 0.028 |
| USG bulky kidney, PNS + | 56 | 10 | 66 |
| USG dilated PCS | 17 | 0 | 17 |
| USG calculi | 2 | 1 | 3 |
| USG cyst | 2 | 0 | 2 |
| USG BPH | 1 | 0 | 1 |
| Total | 84 | 16 | 100 |
(PNS - perinephric fat standing; PCS -pelvicalyceal system; BPH - benign prostatic hyperplasia
Treatment
All patients were treated with appropriate antibiotics and supportive therapy. Majority of them responded to the treatment without any mortality. Intervention in the form of Double J stenting was done in 12 patients and one patient required percutaneous nephrostomy for renal abscess. Dialysis dependent state occurred in 7 (27%) out of 32 patients with chronic kidney disease.
Discussion
The objective of this study was to compare clinical and biochemical parameters with radiological findings (USG/CT) among patients diagnosed to have PN.
Mean age of our patient in this study was 48.7 years, majority of them were above 40 years. In Dhamotharan VN et al., study, majority were in the age group of 51-60 years [8]. Mean age of patient was 57.4 years in a study done by Kumar S et al., [9] and the mean age was 37 years in a study done by Rollino C et al., [10]. The prevalence of PN was more common among females and this finding was similar to Kumar S et al., [9] and Rollino C et al., study [10]. This could be explained because of the presence of short urethra among female. In this study, the mean duration of symptoms prior to hospitalisation was 8.9 days and it was 18 days in kumar S et al., study [9]. Mean length of hospitalisation was 6.8 days in present study and 11 days in a study by Rollino C et al., [10].
Classical triad of PN was present in 87 patients in this study which was higher than that found by Dhamotharan VM et al(35%) [8]. Renal dysfunction was present in 79 patients, of these 47 had acute kidney injury and 32 had chronic kidney disease. Study by Kumar S et al., found the renal dysfunction among 93% patients [9]. Microscopic haematuria was seen in 21% in this study, whereas it was 7% in Dhamotharan VM et al., group [8]. Urine cultures were positive in 24% of patients in present study, it was positive in 88.5% of patients in Kumar S et al., study [9]. Gram-negative bacilli, Escherichia coli were the most frequently isolated organism. Low yield of urine culture may be due to prior use of antibiotics or presence of atypical organisms which requires special culture media.
Diabetes mellitus was the most common comorbidity in our patients (69) which was similar to the findings by Dhamotharan VM et al., [8]. Diabetics are more prone to infection because of diabetic cystopathy, alteration of bacteria-host interaction and defective neutrophil bactericidal activity, impaired phagocytosis and chemotaxis[11-13]. Geerling SE et al., stated an increased adherence of Escherichiacoli to diabetic uroepithelial cells and this was due to higher levels of glycosylated haemoglobin (HbA1c)[12]. Due to impaired production of cytokines, the Escherichia coli infection does not cause symptomatic urinary tract infection (UTI) in diabetic.
Nephrolithiasis had been reported to be a risk factor for PN. In this study 9% of patients had renal calculi on CT. Studies have found that renal stones act as nidus for bacteria so are associated with treatment failure for uncomplicated PN[13,14].
In this study, EPN was found in 4 patients on CT, all were in Class 2 based on classification proposed by Huang JJ and Tseng CC [7]. Three out of these four patients were diabetic. Patients improved after antibiotic therapy alone for two weeks.
Classical triad of symptoms to diagnose PN is not specific and sensitive. Studies have shown CT was better in detecting PN in the form of parenchymal abnormalities like perinephric stranding, bulky kidney, decreased or delayed cortical enhancement (on contrast), inflammatory masses, kidney enlargement or gas formation [15,16]. Majd M et al reported a sensitivity of 86.8% and specificity of 87.5% of CT in diagnosing APN, compared with 74.3% and 56.7% for USG [17].
In our study, USG abdomen was able to detect PN in 66/100 patients, while CT detected in 70/74 of patients, including renal abscess in three patients, emphysematous PN in four patients which was missed in USG. CT was found to reduce the risk of missing renal abscesses by about 37 times compared with USG [18].
There are few studies that correlate the clinical and biochemical parameters with CT diagnosed APN for identification of severity of disease [2,19-22]. Only two studies have shown good correlation of CT findings with clinical severity [2, 21].
Limitation
The limitation of the study were that it is based on review of hospital records, CT reports were not available for 26 patients and CT did not show any significant association with clinical and biochemical parameters. Prospective studies with simultaneous comparison of USG and CT findings in patients with PN will help decide better mode of diagnosis.
Conclusion
From our study, it was found that diabetics are at higher risk of developing PN. Early diagnosis helps prevent complications. Majority of PN patients respond to antibiotics when diagnosed early.
(Triad of PN-Fever, flank pain, dysuria. DM-Diabetes Mellitus, HTN-Hypertension, AKI-Acute kidney injury, CKD-Chronic kidney disease, BPH-Benign prostatic hyperplasia.)