Necrotizing Fasciitis: A Rare Complication of Acute Necrotizing Pancreatitis
Sumesh Kaistha1, Ameet Kumar2, TS Ramakrishnan3
1 Assistant Professor, Department of Surgery, Command Hospital Air force, Bangalore, Karnataka, India.
2 Assistant Professor, Department of Surgery, Command Hospital Air force, Bangalore, Karnataka, India.
3 Professor, Department of Surgery, Command Hospital Air force, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ameet Kumar, Department of Surgery, Command Hospital Air Force, Agram Post, Bangalore-560007, Karnataka, India.
E-mail: Docam@rediffmail.com
Necrotizing pancreatitis occurs in 10 to 25% of patients requiring hospital admission for acute pancreatitis and carries a high mortality rate. Necrotizing pancreatitis can cause a spectrum of complications. However, we report an extremely rare complication of necrotizing pancreatitis: necrotizing fasciitis of the abdominal wall. A 56-year-old male patient presented to our center with discoloration of skin over left flank of 15 days duration and pus discharge from it since three days. Two months back he was managed at a private hospital as a case of acute necrotizing pancreatitis and was discharged after one week of inpatient treatment. After discharge patient continued to have malaise and weakness but was able to do his routine day to day activity. On presentation at our hospital, patient was in septic shock and was taken emergently to operating theatre for debridement. However, later, the patient succumbed to his illness. Necrotizing fasciitis is an extremely uncommon complication of necrotizing pancreatitis and has a fulminant course. Timely detection and debridement can avert a potential mortality.
Acute Pancreatitis, Complications, Retroperitoneal Abscess
Case Report
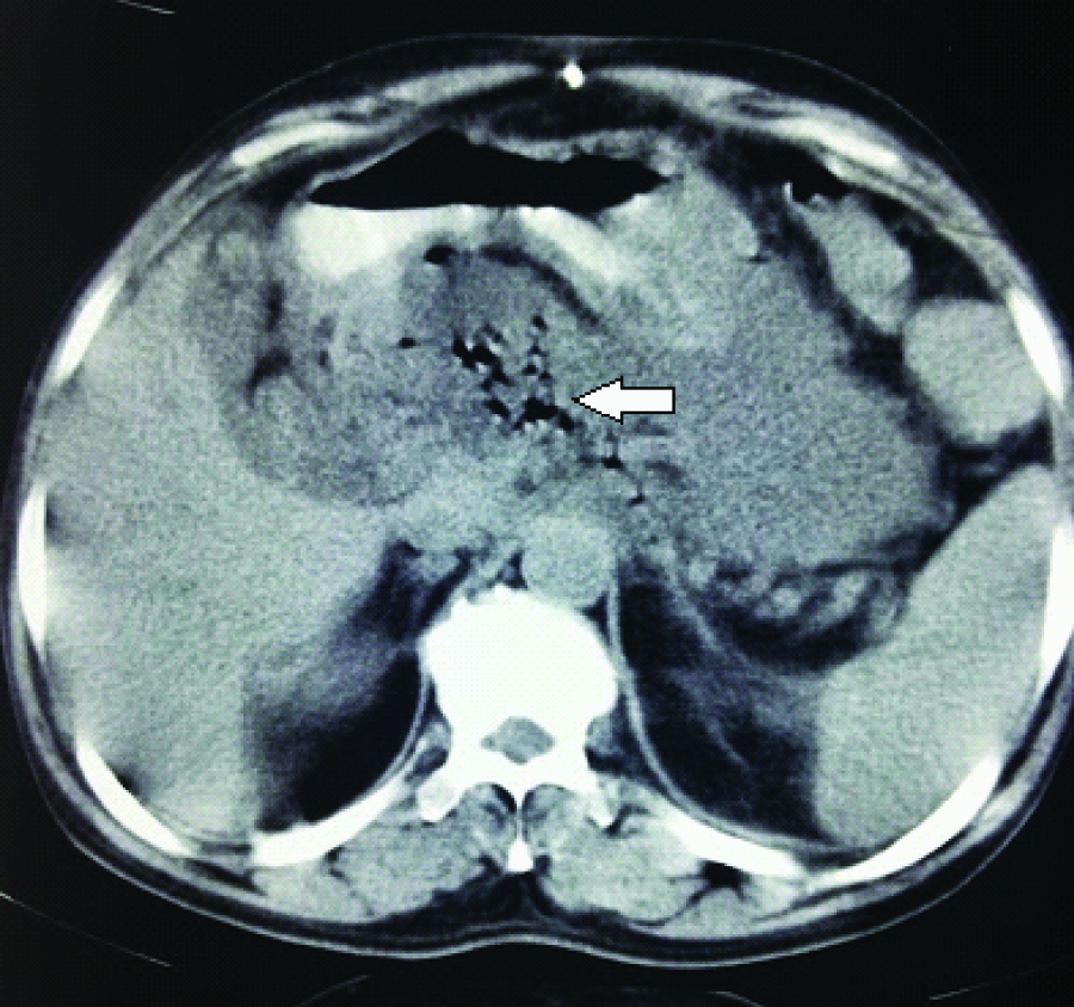
A 56-year-old patient complained of moderate intensity pain in epigastrium since two months. He gave history of alcohol consumption occasionally. He was evaluated at another hospital. His serum amylase was 1246 IU/L and CECT abdomen showed features of Acute Necrotizing Pancreatitis (ANP) with large peripancreatic collection extending till lower left psoas muscle with air pockets [Table/Fig-1]. After a week of conservative management, the patient was discharged as he had no organ failure and was on full oral diet. He remained comfortable for about two weeks after discharge except for some malaise and weakness. Thereafter, he developed skin erythema over the left flank which rapidly progressed to skin necrosis over the next 15 days. He never had fever during this entire period of illness. He was then brought to our hospital with the above complaints. In the past, he had undergone a gastrojejunostomy 20 years back for peptic ulcer disease.
CECT abdomen six weeks prior to presentation showing acute necrotising pancreatitis with peripancreatic with air pockets (Arrow).
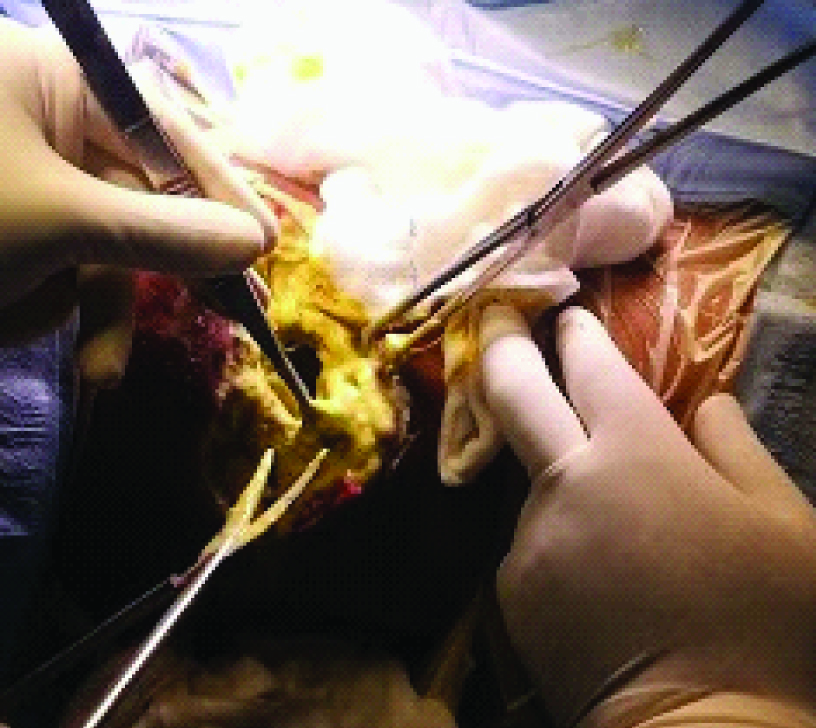
On examination, patient was toxic and in a poor general condition. He had tachycardia (120/min), hypotension (84/60 mmHg) and generalized oedema. Locally, he had a 15 x10 cm necrotic skin over the left flank with pus pouring out from the border of necrosis. He had leucocytosis (12800 cells/cmm), serum albumin was only 2.5 G/dL and serum amylase was 274 IU/L. As the patient’s general condition was poor with deranged renal functions, a repeat CECT was not done. After resuscitation and administration of broad spectrum antibiotics, he was taken up for urgent surgery (retroperitoneal debridement) [Table/Fig-2].
Intraoperative photograph showing debridement/ necrosectomy being done.
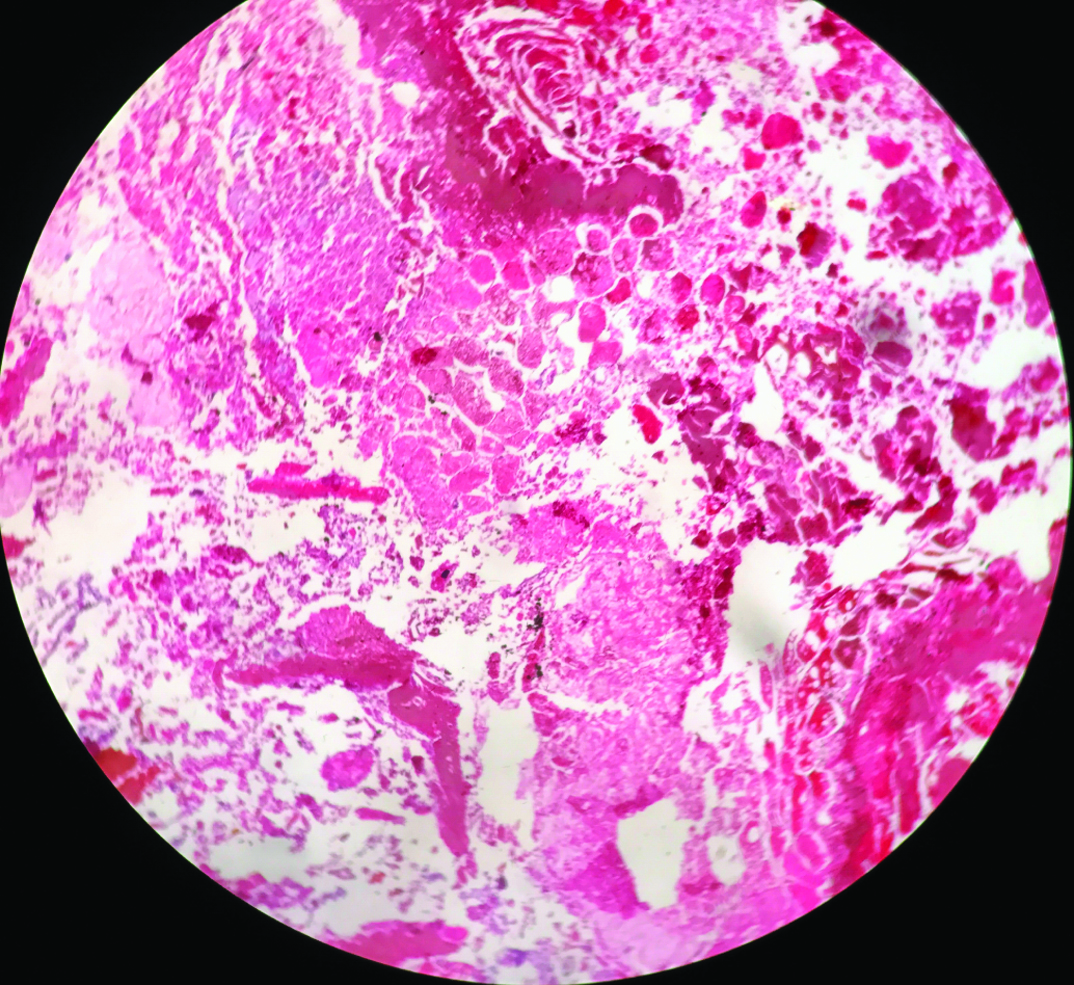
Intraoperatively, after excising 15 x10 cm necrotic skin, subcutaneous tissue and the abdominal muscle, the lesser sac was entered and pancreatic necrosum was removed along with pus. The cavity was thoroughly washed and Bogota bag applied with two tube drains in the cavity for wash [Table/Fig-3]. Postoperatively patient remained haemodynamically unstable and required high inotropic support. His clinical condition continued to deteriorate and succumbed to overwhelming sepsis on the third postoperative day. Histopathology of the necrotic tissue showed ghost outline of lobular and acinar pattern of inflammatory pancreatic tissue along with degenerated cells and large areas of haemorrhage and haemosiderin pigment [Table/Fig-4].
At the end of debridement: Two drains placed and Bogota bag applied.

Photomicrograph of pancreatic necrosectomy specimen showing ghost outline of lobular and acinar pattern of inflammatory pancreatic tissue along with degenerated cells and large areas of haemorrhage and haemosiderin pigment (H&E; 10x).
Discussion
ANP occurs in around 10-25% of patients of acute pancreatitis with mortality rate as high as 25% [1]. Necrotising fasciitis on its own also has a significant mortality rate of 24-34% [2]. The tissues adjacent to the pancreas progressively get necrosed over days or weeks before becoming evident [3]. The skin and subcutaneous tissue eventually becomes ischaemic and infected due to vascular thrombosis [4]. Necrotising fasciitis of flank can be caused by any underlying organ which can lead to inflammation/infection of the retroperitoneal tissues like complicated diverticulitis of colon, perforated appendix, posterior duodenal perforation, colonic perforation into the retroperitoneum, pyelonephritis or perinephric abscess. Rarely, perianal abscesses too can spread to involve the retroperitoneum and cause necrotising fasciitis [5]. Thus, Necrotising fasciitis can present as a complication of retroperitoneal abscess [6]. Retroperitoneal abscess has an indolent course over weeks with vague symptoms and nonspecific signs and once Necrotising fasciitis of retroperitoneum develops, there is almost uniform fatality [4,7]. In our patient, other causes of retroperitoneal abscess like pericolic and perirectal sepsis were ruled out clinically and with CT scan and later, confirmed on postoperative biopsy of the pancreatic necrotic tissue. The management of this condition will entail early detection, resuscitation and aggressive surgical debridement.
After a thorough literature search until December 2016 using MEDLINE and Google Scholar with key words like Necrotizing, fasciitis, retroperitoneum, pancreatitis, cutaneous; we found only one case in literature [8]. The case mentioned in this article and our patient had strikingly similar features. Both patients, after they seemed to have recovered from pancreatitis, suddenly developed skin changes without much systemic features which rapidly developed into a large patch of skin necrosis. Another similarity in these patients was that clinically, both did not manifest symptoms and signs of severe pancreatitis. Similar observation was made in another study on ANP by Miller BJ et al., where he found the low initial APACHE II score were frequently found in patients who ultimately died of retroperitoneal fasciitis [3].
Conclusion
Necrotizing fasciitis is an extremely uncommon complication of acute necrotizing pancreatitis and has a fulminant course. A clinician should be cautious of this rare entity because the only chance of survival is timely detection and debridement.
Conflict of Interest
The authors declare that they have no source of funding or conflict of interest to declare.
[1]. Baron TH, Morgan DE, Acute necrotizing pancreatitisN Engl J Med 1999 340(18):1412-17. [Google Scholar]
[2]. Sarani B, Strong M, Pascual J, Schwab CW, Necrotizing fasciitis: current concepts and review of the literatureJ Am Coll Surg 2009 208(2):279-88. [Google Scholar]
[3]. Miller BJ, Henderson A, Strong RW, Fielding GA, DiMarco AM, O’Loughlin BS, Necrotizing pancreatitis: operating for lifeWorld J Surg 1994 18(6):906-10. [Google Scholar]
[4]. Woodburn KR, Ramsay G, Gillespie G, Miller DF, Retroperitoneal necrotizing fasciitisBr J Surg 1992 79(4):342-44. [Google Scholar]
[5]. Amaranathan A, Sahoo AK, Barathi D, Shankar G, Sistla SC, muacevic a, adler jrRetroperitoneal necrotizing fasciitis masquerading as perianal abscess –rare and perilouscureus 2017 9(1):e982doi: 10.7759/cureus.982 [Google Scholar]
[6]. Amitai A, Sinert R, Necrotizing fasciitis as the clinical presentation of a retroperitoneal abscessJ Emerg Med 2008 34(1):7-40. [Google Scholar]
[7]. Pryor JP, Piotrowski E, Seltzer CW, Gracias VH, Early diagnosis of retroperitoneal necrotizing fasciitisCrit Care Med 2001 29(5):1071-73. [Google Scholar]
[8]. White NR, Fowler LL, Retroperitoneal and cutaneous necrotizing fasciitis secondary to necrotizing pancreatitisJ Emerg Med 2014 47(2):147-49. [Google Scholar]