To Evaluate the Change in Brain Natriuretic Peptide Levels in Outpatients with Ischemic Cardiomyopathy and Its Association with Functional Capacity: A Pilot Study
Amarapalli Jayachandra1, Vivek Aggarwal2
1 Specialist, Department of Cardiology, Command Hospital Northern Command, Udhampur, Jammu and Kashmir, India.
2 Assistant Professor, Deparment of Internal Medicine, AFMC, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amarapalli Jayachandra, Specialist, Department of Cardiology, Command Hospital Northern Command, Udhampur, Jammu and Kashmir, India.
E-mail: jamarapalli@gmail.com
Introduction
Literature is sparse on the clinical correlation of six minute walk test (6MWT) and Brain Natriuretic Peptide (BNP) levels in ischemic Cardiomyopathy (Ischemic CMP) patients. New York Heart Association (NYHA) classification is most commonly used for functional assessment of Heart Failure (HF), which is very subjective. This limitation is overcome by 6MWT which has prognostic significance in addition to assessment of level of functional impairment. Serum BNP correlate with clinical severity of HF as assessed by NYHA class.
Aim
To evaluate the change in BNP levels in outpatients with ischemic CMP and its association with functional capacity.
Material and Methods
Sixty seven patients of established ischemic CMP by coronary angiography With Left Ventricular Ejection Fraction (LVEF) <40%, were recruited on an Outpatients Department (OPD) basis and assessed for baseline BNP levels and functional capacity (NYHA class and 6MWT). These patients were managed on OPD basis and the treatment was optimised and all the aggravating factors like uncontrolled diabetes, hypertension and anaemia were corrected. Patients were also advised life style modifications and cessation of smoking and alcohol consumption. All these patients were followed up for six months with optimum medical treatment and repeat 6MWT and BNP levels. Primary end point was change in the functional class and the BNP levels at six months. Statistical analysis was done with paired t-test and Pearson correlation for BNP levels and 6MWT/NYHA class.
Results
A total of 67 patients were enrolled, out of which 48 patients had six months follow up. Thirty two patients were in NYHA Class II and remaining was in NYHA Class III at the time of enrollment. At six months, 37 were in NYHA Class II and 11 in Class III. At enrollment, 37 cases were able to walk >300 m in six minutes and 11 cases walked < 300 m where as at six months 43 walked >300 m and five walked <300 m. As compared to baseline the mean distance covered in 6MWT showed significant improvement and with reduction in BNP levels at six months (p<0.001). Mean BNP levels correlated better with 6MWT (p <0.001) than NYHA class (p<0.67).
Conclusion
In patients with established ischemic CMP with LVEF <40%, there is a significant reduction in BNP levels and improvement in 6MWT at six months with optimum medical therapy. A 6MWT correlated better with BNP levels than with NYHA class with a significant p-value. However, larger such studies and a longer duration of follow up is desirable to prove this association.
Cardiac biomarkers, Heart failure, New York Heart Association class, Six minute walk test
Introduction
Functional limitation in HF is widely assessed using NYHA functional classification. NYHA functional class is a subjective assessment which varies from person to person and is difficult to measure [1]. 6MWT is a simple, easily reproducible, bedside and objective assessment tool which can measure the level of functional impairment [2,3]. Elevated plasma BNP levels have been associated with reduced LVEF, left ventricular hypertrophy, elevated left ventricular filling pressures, and Acute Coronary Syndromes (ACS) [4]. BNP levels tend to be less elevated in HF with preserved Ejection Fraction (EF) than with reduced EF. BNP levels correlate with NYHA class for assessing severity of HF [5-8]. Hospitalized patients tend to have higher BNP levels which decrease with optimal medical therapy for decompensation. BNP is a powerful test in assessing the prognosis in the patients with HF [9-11]. Literature is sparse on the clinical association of 6MWT and BNP levels in patients with Ischemic CMP. The hypothesis of this study was that 6MWT is a better, objective measure to assess functional status in patients with ischemic CMP and has a good association with the BNP levels. This was a pilot study to see the association of the BNP levels with 6MWT in the patients of established Ischemic CMP attending the OPD of a tertiary care centre in North India. These patients were followed up for six months and the change in the 6MWT and BNP levels were noted after optimization of the therapy and the aggravating factors. Objectives of this study was to assess the utility of BNP levels in predicting future outcomes in OPD patients with ischemic CMP, to evaluate the ability of BNP levels and 6MWT in predicting future adverse cardiac events and to observe any new associations between BNP levels and functional capacity in the patients with ischemic CMP.
Materials and Methods
This study was conducted at a tertiary care post graduate research institute in North India from July 2011 to December 2013. It was a prospective observational study done in OPD patients of Ischemic CMP. Ischemic CMP was confirmed on the basis of previous coronary angiography showing more than 75% of stenosis of either Left Anterior Descending (LAD) or left main or any of the other two coronary vessels along with decreased left ventricular systolic function with EF of less than 40% as assessed by transthoracic echocardiography [12]. On recruitment 5 ml blood sample was collected for BNP levels and subsequently patients were subjected to 6MWT. These patients were followed up and the treatment was optimized. All the aggravating factors like uncontrolled diabetes, hypertension and anaemia were corrected. Patients were also advised life style modifications and cessation of smoking and alcohol consumption. These methods were administered by educating and counseling of the patients at the time of OPD consultations and were reinforced at the time of each follow up (OPD visit/admission to the hospital). All these patients were followed up for six months with optimum medical treatment. After six months 6MWT and BNP levels were repeated, patients were divided into five groups (<150, 150-300, 301-450, 451-600 and > 600 m) according to the distance covered in 6MWT. The 6MWT was performed on a ground level in the enclosed corridor. The corridor was air conditioned and had a walking ramp of 44.1 mtr/147 ft length.
A detailed proforma was prepared to obtain details regarding the sociodemographic characteristics of the patient, the presenting signs and symptoms, time duration and severity at presentation, comorbidities, and risk factors for HF. The effect of treatment and outcome at every contact in OPD/hospitalization during follow up period of six months was assessed. Primary endpoint was change in functional capacity as assessed by 6MWT and NYHA class and change in the BNP levels at six months with optimal medical therapy and secondary endpoints were cardiovascular mortality, morbidity, hospitalization and coronary intervention in the follow up period of six months. The data was collected and analysed. The study was approved by Institutional Ethical Committee and informed consent was taken from all the patients.
All established patients of Ischemic CMP confirmed on coronary angiography with EF of <40% were included.
Patients who were not able to do 6MWT due to any reason, history of recent hospitalization or cardiac decompensation in last three months, patients with chronic obstructive airway disease on spirometry and chest radiograph, chronic kidney disease (GFR <60 ml/min), ACS as established by history, symptoms, ECG and cardiac biomarkers, patients in NYHA Class IV were not included in the study.
Statistical Analysis
All statistical tests were two sided and performed at a significance of α=0.05. For comparison between baselines to six months paired t-test and Pearson correlation coefficient were used to see relationship between change in BNP and 6MWT and NYHA class. Data was analysed using SSPS for windows 17.0.
Results
A total of 67 patients were enrolled, out of which 48 patients completed six months follow up. One patient died during the study period. Mean age of the patients was 59±11.26 years with 35 (73%) being males. Two third (31/48) of the patients were ≥ 55 years of age. Hypertension was the commonest comorbidity noticed in 25 (52%) of the patients followed by diabetes in 16 (33.3%) and dyslipidemia in 12 (25%). Family history of CAD was present in 8 (16.6%) of the patients. Prior history of Percutaneous Coronary Intervention (PCI) was present in 40 (83.3%) of the patients and 2 (4.16%) had atrial fibrillation. At the time of enrollment, the mean BNP level was 1377.96±1004.25 pg/dl, distance covered in 6MWT was 376.74±120.57 m. Two third of the patients (32/48) were in NYHA Class II and remaining was in NYHA Class III [Table/Fig-1].
Baseline characteristics.
| Patient Criteria | | No of Patients n=48 (100%) |
|---|
| Age (years) | Mean Age | 59 ± 11.26 |
| ≥ 65 years | 17 (35.41%) |
| 55-64 years | 14 (29.16%) |
| 45-54 years | 12 (25.0%) |
| 35-44 years | 4 (8.33%) |
| < 35 years | 1 (2.08%) |
| Gender | Males | 35 (72.91%) |
| Females | 13 (27.08%) |
| Confounding risk factors | Family history of CAD | 8 (16.66%) |
| Smoking | 19 (39.58%) |
| Comorbidities | Diabetes mellitus | 16 (33.33%) |
| Hypertension | 25 (52%) |
| Dyslipidemia | 12 (25%) |
| Functional status | Mean 6MWT | 376.74±120.57 |
| NYHA class II | 32 (66.66%) |
| NYHA class III | 16 (33.33%) |
| Baseline BNP levels | | 1377.96±1004.25 |
On follow up, total nine patients were hospitalized. Of the hospitalized patients, three patients had left ventricular failure, two underwent coronary artery bypass grafting, two underwent percutaneous intervention to right coronary artery, one each for permanent pacemaker implantation and severe anaemia requiring blood transfusion. At six months, 37 (77%) were in NYHA Class II and 11 (23%) in class III. There was insignificant change in the NYHA status at the end of six months. There was a significant improvement in the distance covered in 6MWT at six months with p-value of <0.05 as depicted in [Table/Fig-2].
Change in BNP levels and 6MWT at six months according to NYHA class.
| Variables | At onset | At six months | p-value |
|---|
| Mean±SD | Mean±Sd |
|---|
| Class II (N=32) | BNP | 1385.13±989.730 | 585.11±475.570 | <0.001 |
| 6MWT | 443.220±75.0160 | 495.43±78.608 | 0.002 |
| Class III (N=16) | BNP | 1364.47±1061.781 | 894.59±722.983 | 0.002 |
| 6MWT | 251.621±85.0631 | 339.31±120.948 | <0.001 |
Paired t-test for correlation of mean BNP and mean 6MWT with NYHA class at onset and six months follow up.
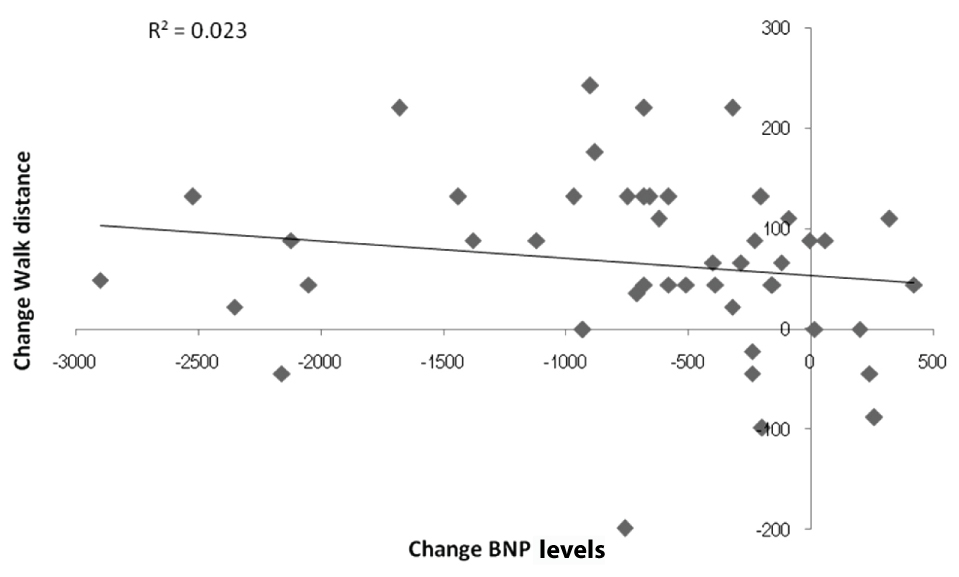
Paired t-test for association of mean BNP to mean 6MWT at baseline and after six months of optimal medical treatment showed significant improvement of mean 6MWT with reduction of BNP levels at six months follow up with a p-value of <0.001 [Table/Fig-2]. Higher BNP levels were noted at baseline in NYHA Class II than NYHA Class III. However, on follow up at six months it was noted that the reduction in BNP was greater in NYHA Class II than NYHA Class III. Pearson correlation for the significance (2 tailed) of change in BNP to change in 6MWT shows inverse correlation of change in BNP levels to the change in 6MWT [Table/Fig-3].
Scatter diagram depicting inverse correlation between change in 6MWT and change in BNP levels.
Discussion
Coronary artery disease is a leading cause of morbidity and mortality in India [13]. In a poor country with limited resources, medical management is the cornerstone of management in these patients as most of the patients cannot afford coronary interventions. Thus, objective assessment of effect of optimum medical management with 6MWT and BNP levels is important in deciding the effect of optimum medical therapy in these patients. This will help to formulate future research and medical interventions in these patients. There is very less data available where 6MWT and BNP levels have been compared in patients with Ischemic CMP. In a study done by Ziskoven D et al., showed that the mean BNP levels correlated better with 6MWT than NYHA class [14]. In our study also, it was seen that BNP levels had a significantly better inverse correlation with 6MWT than with NYHA functional class. In another study done by Jourdian P et al., it was seen that 6MWT gave more objective assessment of functional class than NYHA class which was consistent with our study [15]. It also showed that there was an inverse correlation between 6MWT and BNP levels. In a study done by Wieczorek ST et al., it was noted that patients of HF with reduced functional capacity and raised BNP (median 1080 pg/dl) had a poorer outcome with increased mortality [16]. In our study, one patient died of heart failure and this patient had very high BNP levels of more than 1000 pg/dl at the baseline. One patient had a sudden cardiac death at home and his baseline BNP levels were also more than 1000 pg/dl with LVEF of 20%. There are number of studies available on elevated BNP levels in patients with acute HF requiring hospitalization and its association with adverse outcomes including death [17,18]. The data on patients with Ischemic CMP attending the outpatient department is very minimal and can go a long way in stratifying the risk in patients.
In most studies mentioned above, the patients of chronic HF were classified into specific aetiologies, but in our study we studied the subset of patients with Ischemic CMP only and our results are comparable with the results of BNP levels in patients with diverse aetiology. Our study signifies the utility of BNP in Ischemic CMP. Our study shows that in patients with Ischemic CMP, BNP levels correlates well with functional status of the patient as assessed by 6MWT and with optimum medical therapy, there is improvement in the functional status with reduction in BNP levels. The strength of the study is that it was a first study assessing the association between 6MWT and BNP levels in the patients with Ischemic CMP.
Limitation
The limitations of our study are the small sample size, lesser duration of follow up of patients and significant loss to follow up (19/67). The patients were lost to follow up as they came from very long distances including the mountainous terrain. Only one patient was confirmed to have died of sudden cardiac arrest at home. Information of other patients who were lost to follow up is not available. However, only the patients who could be followed up were only included in the final analysis.
Conclusion
After optimum medical therapy in the patients with established Ischemic CMP, there was significant reduction in BNP levels and improvement in 6MWT at six months. BNP levels correlated better with 6MWT than with NYHA class. However, larger such studies and a longer duration of follow up is desirable to prove this association. It will be desirable to study the role of optimal medical management in ischemic CMP as most of the patients in developing countries are on medical management.
Paired t-test for correlation of mean BNP and mean 6MWT with NYHA class at onset and six months follow up.
[1]. The Criteria Committee of the New York Heart AssociationDiseases of the Heart and Blood Vessels: Nomenclature and Criteria for Diagnosis 1964 6th EditionBoston, MALittle, Brown [Google Scholar]
[2]. Harada ND, Chiu V, Stewart AL, Mobility-related function in older adults: assessment with a 6-minute walk testArch Phys Med Rehabil 1999 80(7):837-41. [Google Scholar]
[3]. Lord S, Menz H, Physiologic, psychologic, and health predictors of 6-minute walk performance in older peopleArchives of Physical Medicine And Rehabilitation 2002 83(7):907-11. [Google Scholar]
[4]. Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Richards AM, Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (NBNP) concentrationsLancet 2000 355:1126-30. [Google Scholar]
[5]. Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM, Two-, six-, and 12-minute walking tests in respiratory diseaseBritish Medical Journal Clinical Research Ed 1982 284(6329):1607-08. [Google Scholar]
[6]. Bibbins-Domingo K, Gupta R, Na B, Wu AH, Schiller NB, Whooley MA, N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart diseaseJAMA 2007 297(2):169-76. [Google Scholar]
[7]. Fitzgerald RL, Cremo R, Gardetto N, Chiu A, Clopton P, Bhalla V, Effect of nesiritide in combination with standard therapy on serum concentrations of natriuretic peptides in patients admitted for decompensated congestive heart failureAm Heart J 2005 150(3):471-77. [Google Scholar]
[8]. Maisel A, B-type natriuretic peptide levels: a potential novel “white count” for congestive heart failureJ Card Fail 2001 7:183-93. [Google Scholar]
[9]. Hutfless R, Kazanegra R, Madani M, Bhalla MA, Tata AT, Chen A, Utility of B-type natriuretic peptide in predicting postoperative complications and outcomes in patients undergoing heart surgeryJ Am Coll Cardiol 2004 43(10):1873-79. [Google Scholar]
[10]. Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breathJ Am Coll Cardiol 2004 44(6):1328-33. [Google Scholar]
[11]. Lam LL, Cameron PA, Schneider HG, Abramson MJ, Müller C, Krum H, Meta-analysis: effect of B-type natriuretic peptide testing on clinical outcomes in patients with acute dyspnea in the emergency settingAnnals of Internal Medicine 2010 153(11):728-35. [Google Scholar]
[12]. Felker GM, Shaw LK, O’Connor CM, A standardized definition of ischemic cardiomyopathy for use in clinical researchJournal of the American College of Cardiology 2002 39(2):210-18. [Google Scholar]
[13]. Gupta R, Mohan I, Narula J, Trends in coronary heart disease epidemiology in IndiaAnnals of Global Health 2016 82(2):307-15. [Google Scholar]
[14]. Ziskoven D, Forssmann WG, Holthausen U, Menz G, Addicks K, Rippegater G, Calcium calmodulin antagonists influences the release of cardiodilatin/ANP from atrial cardiocytesHandbook Endocrinology of the Heart 1989 :978-1409. [Google Scholar]
[15]. Jourdain P, Funck F, Bellorini M, Guillard N, Loiret J, Thebault B, Bedside B-type natriuretic peptide and functional capacity in chronic heart failureEur J Heart Fail 2003 5(2):155-60. [Google Scholar]
[16]. Wieczorek SJ, Hager D, Barry MB, Kearney L, Ferrier A, Wu AH, Correlation of B-type natriuretic peptide level to 6-min walk test performance in patients with left ventricular systolic dysfunctionClin Chim Acta 2003 328(1-2):87-90. [Google Scholar]
[17]. Januzzi JL, JrChen-Tournoux AA, Moe G, Amino-terminal pro-B-type natriuretic peptide testing for the diagnosis or exclusion of heart failure in patients with acute symptomsAm J Cardiol 2008 101(3A):29-38. [Google Scholar]
[18]. Baggish AL, van Kimmenade RR, Januzzi JL, JrThe differential diagnosis of an elevated amino-terminal pro-B-type natriuretic peptide levelAm J Cardiol 2008 101(3A):49-55. [Google Scholar]