Cisplatin Induced Acute Myocardial Infarction and Dyslipidemia
Lalith Prabhakar Hanchate1, Shimpa Rakesh Sharma2, Sadhana Madyalkar3
1 Senior Resident, Department of General Medicine, Padmashri Dr D Y Patil Hospital and Research Institute, Kolhapur, Maharashtra, India.
2 Professor, Department of General Medicine, D Y Patil Medical College, Kolhapur, Maharashtra, India.
3 Junior Resident, Department of General Medicine, D Y Patil Medical College, Kolhapur, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shimpa Rakesh Sharma, 5th Floor, Sai Villa, Karande Mala, Tarabai Park, Kolhapur-416005, Maharashtra, India.
E-mail: shimpasharma@gmail.com
Myocardial infarction commonly occurs due to rupture of atherosclerotic plaque in the coronary arteries and is manifested on coronary angiography. Myocardial infarction with angiographically normal coronary arteries can occur due to hypercoagulable state, coronary spasm, embolism, arteritis, congenital condition and drugs. Illicit drugs such as cocaine, amphetamines and marijuana are known to cause myocardial infarction. Of the many medications that are associated with cardiovascular toxicity, chemotherapeutic agents form a large group with both acute and delayed cardiotoxicity. We present a case of acute myocardial infarction in a patient with no organic coronary artery disease on the Bleomycin, Etoposide and Cisplatin (BEP) regimen for treatment of testicular seminoma. Patient developed symptoms of Acute Coronary Syndrome (ACS) after his third cycle of the regimen. This case highlights the need for prior careful cardiovascular evaluation, close monitoring and use of strategies to prevent cardiovascular morbidity in patients on cisplatin therapy.
Anterior myocardial infarction, Coronary angiography, Coronary vasospasm, Testicular seminoma
Case Report
A 30-year-old male presented with acute retrosternal chest pain radiating to the left arm. He gave history of testicular seminoma for which he had already received three cycles of the BOP regimen and was to receive the fourth cycle the next day. He was a non smoker, non obese person doing regular moderate exercise. Family history was not remarkable. Routine check-up before chemotherapy was normal.
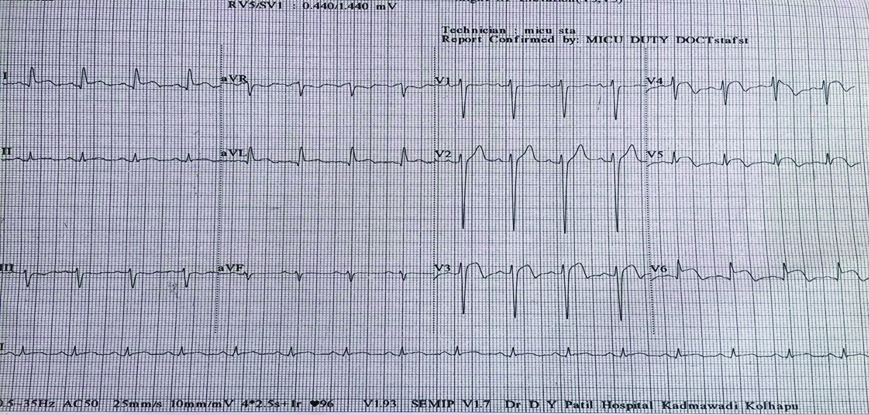
On examination patient had heart rate of 120 bpm, blood pressure of 150/100 mm Hg, waist-hip ratio of 0.95, body mass index of 21 kg/m2 and third heart sound (S3 gallop) with bilateral basal fine crepitations on auscultation. Electrocardiogram (ECG) revealed elevation of the ST segment in anterolateral leads [Table/Fig-1].
ECG at time of presentation.
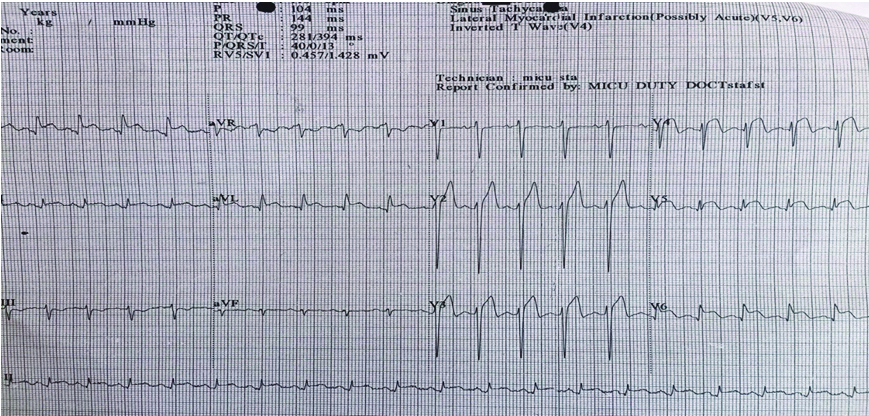
In the medical intensive unit, qualitative troponin T test was positive. As per standard ACS protocol thrombolysis with Streptokinase (STK) was followed by routine management and intravenous furosemide for acute failure. Routine investigations are shown in [Table/Fig-2]. Patient was relieved of chest pain and post-STK ECG showed lowering of J-point elevation [Table/Fig-3]. ECG after 24 hours of STK is seen in [Table/Fig-4].
Laboratory investigations on day 1, 2, and 7.
| Day 1 | Troponin Τ - Positive | CPK-MB - 22 | Troponin τ - 0.05 ng/ml |
|---|
| Hb - 12.8 gm/dl | TC - 4900/cumm | DC - normal |
|---|
| Platelet - 8.42 lacs/cumm | RBS - 99.2 mg/dl |
| Day 2 | T Cholesterol-246 mg/dl | LDL - C: 185 mg/dl | HDL - C:37.4 mg/dl |
| TG - 117 mg/dl | CPK-MB - 25 mmol/dl | HbA1c - 6.1 |
| Day 7 | Blood Sugars: Fasting - 116 mg/dl Post meal (1 hour) - 142.8 mg/dl (2 hours) - 85 mg/dl | |
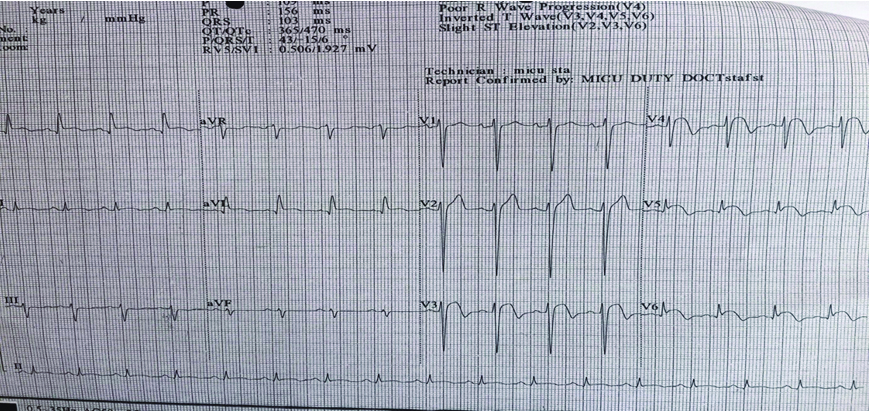
ECG after 24 hrs (Post-STK).
Detailed history and examination with available investigations, led to a suspicion of cisplatin-induced coronary vasospasm. In view of possibility of cisplatin causing coronary spasm and the fact that atherosclerotic coronary artery disease could not be ascertained angiographically due to financial constraints, oral low dose diltiazem was started the next day.
Subsequent investigations revealed hypercholesterolemia, elevated Low Density Lipoprotein Cholesterol (LDL-C) and low levels of High Density Lipoprotein Cholesterol (HDL-C) [Table/Fig-2] with normal levels of Triglycerides (TG). Creatine Phosphokinase Myocardial fraction (CPK-MB) levels were 22 ng/ml and 25 ng/ml on first and second day.
Two dimensional echocardiography done on day three showed anterolateral wall hypokinesia and severe Left Ventricular (LV) dysfunction with LV ejection fraction of 35%. ECGs done on day two and thereafter showed persistent J-point and ST-elevation, though patient was asymptomatic. Dose of oral diltiazem was increased simultaneously monitoring patient for signs or symptoms of ventricular failure. Patient underwent coronary angiography on day five which showed sluggish flow in left anterior descending artery with no thrombus [Table/Fig-5].
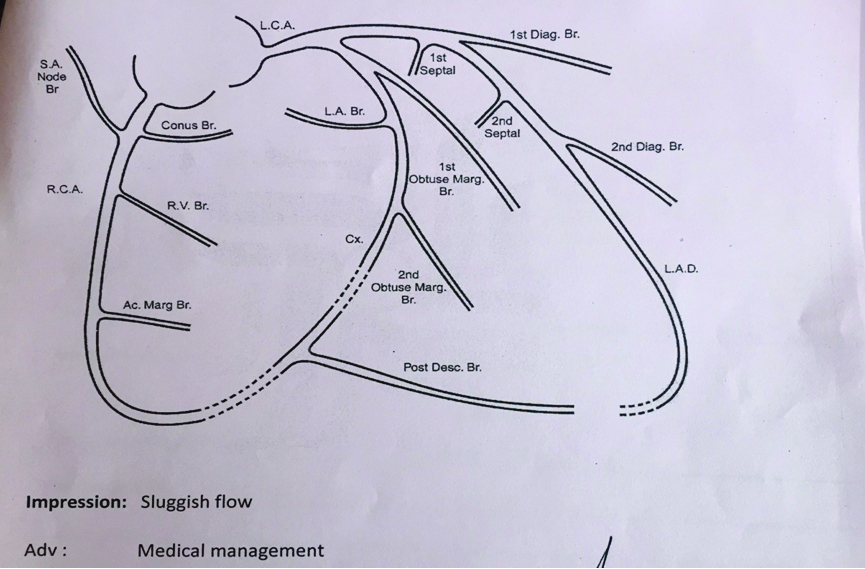
Diagnosis of cisplatin induced ACS was entertained as both dyslipidemia and coronary vasospasm can be explained by cisplatin usage. Patient did not have family history of cardiovascular event, obesity, metabolic syndrome or hypertension amongst common known risk factors. Further use of cisplatin was withheld. The patient then shifted to another larger city for further treatment and was lost to follow up.
Discussion
Myocardial infarction commonly occurs due to rupture of atherosclerotic plaque in the coronary arteries, manifest on coronary angiography. Myocardial infarction with angiographically normal coronary arteries may be due to non atherosclerotic causes including hypercoagulable states, coronary spasm, embolism from endocarditis or myxomas, arteritis and congenital conditions and drugs. Illicit drugs such as cocaine, amphetamines and marijuana are known to cause myocardial infarction. Medications such as ergot alkaloids, diethylstilbesterol, antibiotics and chemotherapeutic agents are also identified as causative factors for this disease [1].
Cisplatin (cis–diamminedichloroplatinumis) is a chemotherapeutic agent used widely in a variety of malignancies such as ovarian, testicular, head, neck and small cell lung cancer. It is associated with cardiovascular toxicity, gastrointestinal toxicity, myelotoxicity, ototoxicity and neurotoxicity, with the chief dose limiting toxicity being nephrotoxicity experienced by 20% of patients [2].
Pathophysiology: There are ‘Type I’ (Anthracyclines-like) and ‘Type II’(Trastuzumab-like) chemotherapy related cardiac dysfunction. Type I results in irreversible cell damage, while Type II leads to loss of contractility, cell hibernation or myocardial stunning, showing more reversibility [3].
Adverse effects: Acute adverse effects are chest pain, distress, palpitations or elevated cardiac enzymes indicative of myocardial infarction [4]. Cisplatin is also known to cause supraventricular tachycardia, bradycardia, repolarisation changes, left bundle branch block, ischaemic events, myocardial infarction and vascular toxicities including Raynaud’s phenomenon [3]. Delayed complications include those that are seen up to 10-20 years after remission such as hypertension, left ventricular hypertrophy and myocardial ischemia or infarction [5].
Mechanisms: Cisplatin cardiotoxicity is mediated through a direct action on myocytes or due to production of Reactive Oxygen Species (ROS) which induce oxidative stress and are pro-thrombotic. Cardiotoxicity has been explained by the result of oxidative stress on the cardiac cells with ensuing lipid peroxidation which causes physical injury and functional damage, the mechanism accounting for elevation of the leaked cardiac enzymes and markers i.e., troponin I [6].
The drug is also known to alter potassium and magnesium levels within and outside the cells predisposing to arrhythmias. Direct action on myocardial sodium channels has also been indicted in their genesis [7].
Acute vascular toxicity due to cisplatin can occur during or soon after chemotherapy is administered and has been attributed to vasospastic angina by some authors [8,9]
Elevated levels of cholesterol, LDL-C and TG have been reported in patients on cisplatin therapy [10-12]. Other researchers have also presented conflicting findings [13]. Elevated levels of total cholesterol reported by Raghavan D et al., revealed an absolute rise in cholesterol levels in 14 out of 17 patients and hypercholesterolemia in 7 out of 17 patients (41%) of cisplatin treated testicular tumors. No specific lipid pattern was noted in their study [11]. Our patient had raised total cholesterol levels in addition to elevated LDL-C levels and low HDL levels though TG levels were normal.
Prevention: Studies on prevention of cardiotoxicity of chemotherapeutic agents have proposed use of dexrazoxane, statins, beta-blockers, angiotensin-convertase enzyme inhibitors, and neuregulin-1 amongst others [5].
Conclusion
Cisplatin is a commonly used chemotherapeutic agent for a variety of malignancies. This case highlights the need to be aware of the acute life-threatening cardiac complications of the drug and also its effect on lipid profile. Prevention of Cardiovascular (CV) side effects can be minimized with use of statins. Regular CV monitoring of all patients especially those not on preventive therapy must be done.
[1]. El Menyar AA, Drug-induced myocardial infarction secondary to coronary artery spasm in teenagers and young adultsJ Postgrad Med 2006 52(1):51-56. [Google Scholar]
[2]. Sawant SP, Prakruthi J, Daddi AD, Ghosh J, Joshi A, Dhir AA, Cisplatin-induced cartiotoxicity–two case reportsOncoreview 2015 5(4):A145-50. [Google Scholar]
[3]. Csapo M, Lasar L, Chemotherapy induced cardiotoxicity: pathophysiology and preventionClujul Med 2014 87(3):135-14. [Google Scholar]
[4]. Berliner S, Rahima M, Sidi Y, Teplitsky Y, Zohar Y, Nussbaum B, Acute coronary events following cisplatin-based chemotherapyCancer Invest 1990 8(6):583-86. [Google Scholar]
[5]. Yeh ET, Tong AT, Lenihan DJ, Yusuf W, Swafford J, Champion C, Cardiovascular complications of cancer therapy diagnosis, pathogenesis and managementCirculation 2004 109:3122-31. [Google Scholar]
[6]. Nuver J, Smit AJ, van der Meer J, van den Berg MP, van der Graaf WT, Meinardi MT, Acute chemotherapy-induced cardiovascular changes in patients with testicular cancerJ Clin Oncol 2005 23:9130-7. [Google Scholar]
[7]. Raja W, Mir MH, Dar I, Banday MA, Ahmad I, Cisplatin induced paroxysmal supraventricular tachycardiaIndian J Med Paediatr Oncol 2013 34(4):330-32. [Google Scholar]
[8]. Fukuda M, Oka M, Itoh N, Sakamoto T, Mori H, Hayakawa A, Vasospastic angina likely related to cisplatin containing chemotherapy and thoracic irradiation for lung cancerIntern Med 1999 38:4368 [Google Scholar]
[9]. Rao AS, Kumar R, Narayanan GS, A rare case of cisplatin-induced acute myocardial infarction in a patient receiving chemoradiation for lung cancerJ Can Res Ther 2015 11:983-85. [Google Scholar]
[10]. Wang G, Su C, Yin T, Paclitaxel and platinum based chemotherapy results in transient dyslipidemia in cancer patientsMolecular and Clinical Oncology 2017 6:261-65. [Google Scholar]
[11]. Raghavan D, Cox K, Childs A, Grygiel J, Sullivan D, Hypercholesterolemia after chemotherapy for testis cancerJ Clin Oncol 1992 10(9):1386-89. [Google Scholar]
[12]. Boes H, Proost JH, Nuver J, Bunskoek S, Gietemal JQ, Geubels BM, Long-term exposure to circulating platinum isassociated with late effects of treatment in testicular cancer survivorsAnnals of Oncology 2015 26:2305-10. [Google Scholar]
[13]. Ellis PA, Fitzharris BM, George PM, Robinson BA, Atkinson CH, Coils BM, Fasting plasma lipid measurements following cisplatin chemotherapy in patients with germ cell tumorsJ Clin Oncol 1992 10:1609-14. [Google Scholar]