Lead Level in Umbilical Cord Blood and its Effects on Newborns Anthropometry
Akbari-Nassaji Neda1, Sabeti Fahimeh2, Ziaei Kajbaf Tahereh3, Fakharzadeh Leila4, Nazari Zahra5, Cheraghian Bahman6, Cham Kouri Narges7
1 MS, Department of Nursing, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran; Abadan School of Medical Sciences, Abadan, Iran.
2 MS, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran; Department of Pediatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
3 Associate Professor, Department of Pediatrics, Aboozar Children’s Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
4 MS, Department of Nursing, Abadan School of Medical Sciences, Abadan, Iran.
5 MS, Nanotechnology Research Center, Department of Toxicology, School of Pharmacy, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
6 PhD Scholar, Department of Biostatistics and Epidemiology, Research Center for Infectious Diseases of Digestive System, School of Public Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
7 PhD Student, Department of Pharmacology and Toxicology, Abadan School of Medical Sciences, Abadan, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Ms. Sabeti Fahimeh, MS, Department of Pediatric Nursing, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
E-mail: sabetifa@yahoo.com
Introduction
High concentration of blood lead is accompanied by adverse health effects on growth of foetus and the newborn.
Aim
The aim of this study was to determine umbilical cord blood lead level and its relationship with birth weight, length and head circumference of the newborns in Abadan, Iran.
Materials and Methods
In this cross-sectional study, 3 ml blood was collected from the umbilical cord vein in 147 newborns, immediately after the birth. Blood lead was measured using atomic absorption spectrophotometry. Data collection instruments included demographic questionnaire (age of mother, gestational age, newborn gender, job and education of mother) and also data registration form (umbilical cord blood lead concentration, weight, length, and head circumference of newborn). Data was analyzed with SPSS software version 16.0.
Results
The mean of umbilical cord blood lead was determined 0.65±0.32 µg/dl (0.3-1.35 µg/dl). The decrease of birth weight with increased blood lead level was small and was not statistically significant. There was reverse significant correlation between umbilical cord blood lead level and birth length and head circumference. There was no significant correlation between blood lead and other variables such as age, weight, education and job of mother and gestational age.
Conclusion
Umbilical blood lead level was determined <5 µg/ dl. Excess of umbilical cord blood lead caused decreasing birth weight, length and head circumference of the newborns.
Birth weight, Blood lead, Fetal development
Introduction
Lead is a neurotoxic metal that is widespread in the environment [1]. Industrial activities, environmental pollution, agricultural technology and processed foods are the main sources of lead [2]. Lead exists in water, food, soil, air, dust, paint, toy, lead glazed ceramic pottery and battery [3]. The first reports of lead poisoning were published in early 19th century in England. Blood lead level of the women who were exposed to lead in workplace or house was reported to be high and a relationship was found between high blood lead levels and low birth weight [4]. Lead causes adverse effects in blood, neural and renal systems and damage of the organs depends on exposure to lead and absorption and desorption [5]. The developing foetus and children are vulnerable to adverse health effects of lead. Lead is easily absorbed through skin, respiration and digestion [6]. The pregnant women who were in touch with lead since childhood, lead is highly stored in their bones and discharged from bones during pregnancy and breastfeeding and enters the blood again [7]. In these women, more than 85% of the lead entering the body is absorbed and is transferred from placenta to foetus and causes serious adverse health effects in foetus. Umbilical cord blood lead level of 10 µg/dl is accompanied by adverse effects such as miscarriage, premature birth, low birth weight [8] and higher level of lead causes more serious complications such as fetal abnormalities, brain injury, hearing and visual impairment and even death [5,6]. According to Agency for Toxic Substance and Disease Registry (2007), there are adverse effects such as neurodevelopmental defect, delay in reproductive system, neurobehavioral effects, reduction of GFR and reduced heme synthesis in PbBs < 0 µg/dl [6]. So, U.S. Preventive Services Task Force (USPSTF) suggests routine screening of pregnant women and children about concentration of the blood lead [9]. In 2010, the US Centers for Disease Control (CDC) [3], and the American College of Obstetricians and Gynecologists recommended that B-Pb should be <5 µg/dl in the pregnant women [10].
Results of the studies conducted on lead level of mother and birth outcome are controversial. Some previous studies found significant reverse relationship between level of umbilical cord blood lead and newborn anthropometry [1,5,11-14]. In other studies, there was no relationship between high umbilical cord blood lead and weight, length and head circumference of the newborn [15,16]. Considering the results in the previous studies and that birth weight is a predictor factor of growth and development and survival of the newborn [5] and low birth weight is one of the important factors of mortality [17], and 5-12% incidence of low birth weight in Iranian newborns [18,19,20], in addition to, relation between blood lead of mother and umbilical cord blood lead in newborns [9,21,22], also, the presence of refinery and petrochemical industries in the middle of Abadan, the researchers carried out this study. Results of this research can be applied in health planning of mothers and newborns. The aim of this study was to determine umbilical cord blood lead level and its relationship with birth weight, length and head circumference of the newborns in Abadan, Iran.
Materials and Methods
This study was a cross-sectional study that was done from June to September 2013 for four months. Ethics approval for the study was obtained from Ethical Committee of Ahvaz Jundishapur University of Medical Sciences. All mothers participated in the study with informed consent. Sampling was done with non probability sampling. In this way, all newborn that had the inclusion criteria since start of the study were selected as sample and this continued until reaching final size of the sample.
Participants: The research population included mothers and newborns in Abadan hospitals. To determine the sample size, mean estimate formula of was used. (α=0.05, б=28.5, d=5). In this study, 147 samples were included. Inclusion criteria for the participant was, 15–49 years old, full term and single pregnancy. The exclusion criteria included mothers with acute, chronic and metabolic diseases, habit of smoking, severe stress in pregnancy and twin pregnancy.
Data collection and analysis: Data collection instruments included demographic questionnaire (age of mother, gestational age, newborn gender, job and education of mother) and also data registration form (umbilical cord blood lead concentration, weight, length, and head circumference of newborn). A total of 3 ml blood was collected from umbilical cord vein using heparin as anticoagulant, immediately after the birth. The samples were kept under cold conditions in cold box and sent to Biochemical Laboratory of Abadan School of Medical Sciences. Tests were performed by a single individual and with atomic absorption spectrophotometry equipped with GTA 120 graphite furnace, Varian model. All statistical analysis was performed using SPSS software version 16.0. A p≤0.05 was set as the level of statistical significance. Descriptive statistics were reported as mean ±SD. Means of two and more than two groups were compared with t-tests or parametrical equivalence (Mann–Whitney) and Kruskal– Wallis test. Spearman correlation coefficient was calculated for correlation between two quantitative variables.
Results
Blood lead concentrations in these sample were low (<5 µg/dl). Characteristics of mothers and newborns at time of study enrollment and mean and standard deviation of umbilical cord blood lead, birth weight, length and head circumference are given in [Table/Fig-1,2].
Characteristics of mothers and newborns at the time of study enrollment(n=147).
| Variables | No. (%) Mean±SD |
|---|
| Newborn: |
| Sex | Male | 52.4% (77) |
| Female | 47.6% (70) |
| Weight | ≤2500 g | 5.4% (9) |
| ≥2500 g | 94.6 (138) |
| Mother: |
| Age (years) | 25.4±5.1 |
| Weight (Kg) | 72.6±10.3 |
| Gestational Age (weeks) | 38.3±3.82 |
| Urban / Rural | Urban | 88.4% (130) |
| Rural | 11.6% (17) |
| Education of mother | Less than high school | 21.8% (32) |
| High school | 51.6% (76) |
| Some college or bachelor degree | 26.6% (39) |
| Job status | Housewives | 95.2% (140) |
| Employed | 4.8% (7) |
Mean and standard deviation of umbilical cord blood lead concen- I tration, birth weight, length and head size.
| Variables | Mean | SD |
|---|
| Lead concentration (μg/dl) | 0.65 | 0.32 |
| Weight (g) | 3167.55 | 438.29 |
| Length (cm) | 49.25 | 3.18 |
| Head circumference | 34.32 | 1.48 |
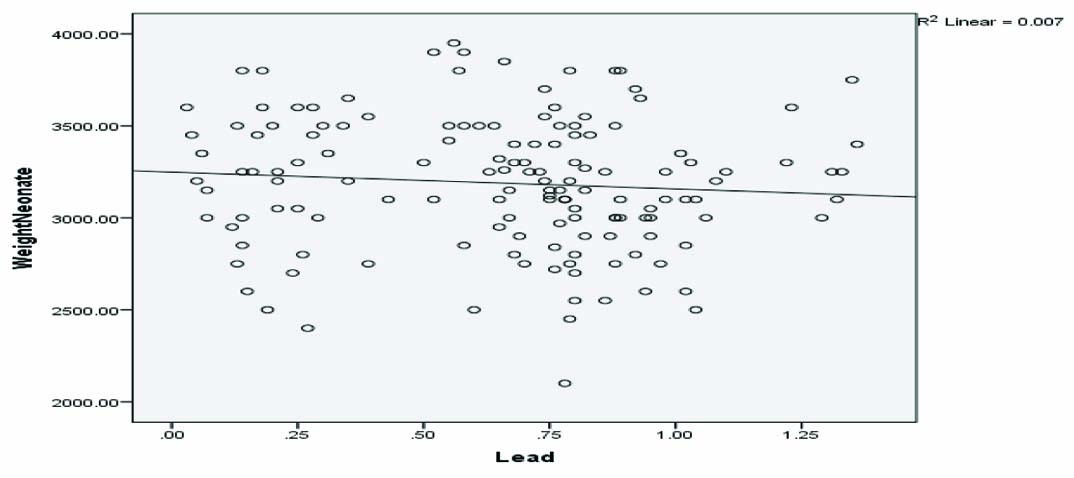
Relationship between blood lead and birth weight was studied with Spearman correlation coefficient and the decrease of birth weight with increase blood lead was small, it was not significant (p=0.092, r=-0.141) [Table/Fig 3].
Relationship between umbilical cord blood lead and newborn birth weight.
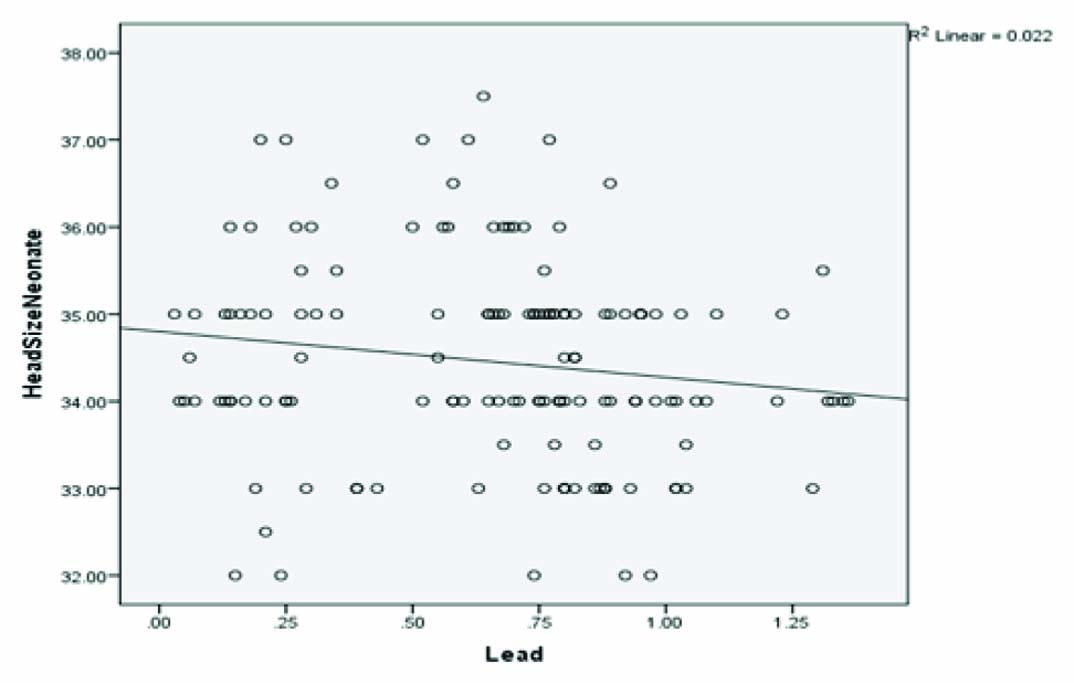
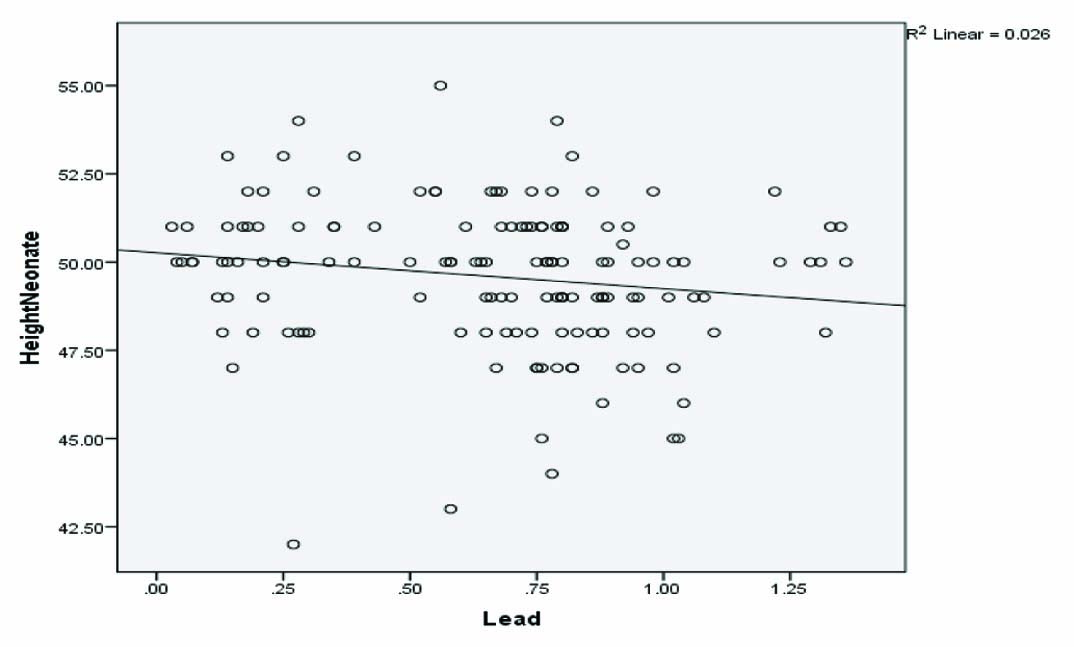
A significant correlation was found between length and head circumference of newborn and umbilical cord blood lead (r=-0.22, p=0.008), (r=-0.20, p=0.01) [Table/Fig-4,5].
Relationship between umbilical cord blood lead and newborn head circumference.
Relationship between umbilical cord blood lead and newborn birth length.
To determine relationship between gender of neonate and blood lead, independent t-test was used and no significant correlation was obtained (t=1.07, df=147, p=0.29). Relationship between umbilical cord blood lead and other variables of age, weight and education of mother was also studied and no significant correlation was found in any case. No significant relationship was reported between umbilical cord blood lead and residential place with Mann–Whitney test (p=0.74) and job of parents with Kruskal–Wallis test (p=0.71).
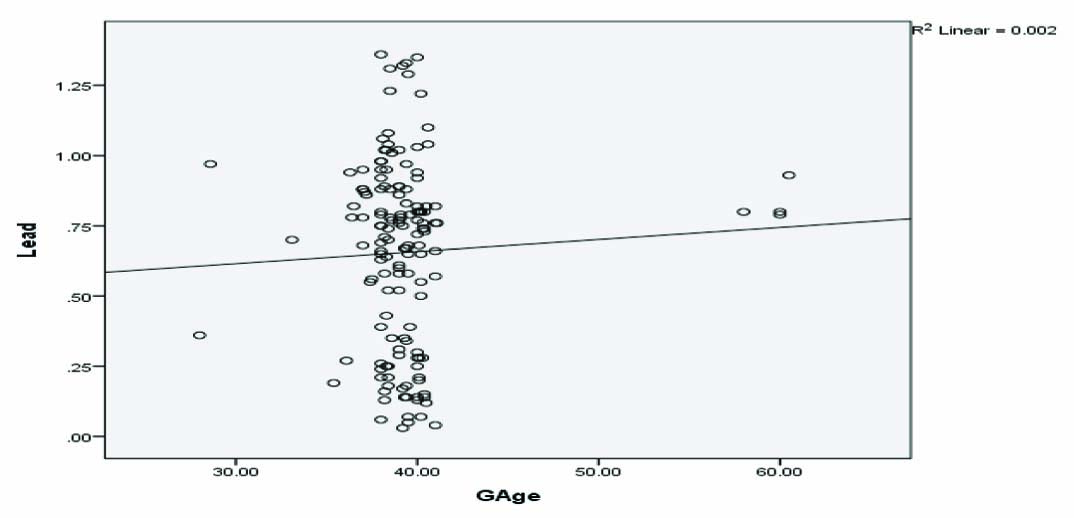
No significant relationship was reported between gestational age and umbilical cord blood lead based on Spearman correlation coefficient (r=-0.08, p=0.28) [Table/Fig-6].
Relationship between umbilical cord blood lead and gestational age.
Discussion
In this study, mean umbilical cord blood lead was determined as 0.65±0.32 µg/dl (0.3-1.35 µg/dl) and blood lead was <5 µg/dl. Some previous studies had similar results [21,23,24,25]. Umbilical cord blood lead was reported to be 0.015±0.009 µg/dl in France and 0.3±0.5 µg/dl in Portugal [23]. Based on studies by Zentner LE et al., Schell CM et al., and Al-Jawadi AA et al., the umbilical cord blood lead level were reported as 3.9µg/dl, 1.58µg/dl, 3.26±1.91µg/ dl respectively [5,21,24]. In the study by Lee MG et al. blood lead level of women of reproductive age (20-49 years) was determined 1.8 µg/dl in America [25].
Blood lead level of neonate depends on exposure of mother to lead in environment, its storage in body and lead release in blood in pregnancy and its passage from placenta to foetus [7,21]. Also maternal diet and nutritional status during pregnancy affects blood lead level. Diet containing vitamin D, calcium, iron and zinc affects on reduction of neonatal blood lead level. Specially, relationship between high calcium level of mother and low lead level of neonate has been proved in some studies [21,24,26,27]. Lead and calcium have similar chemical structure and lead can potentially impair normal fetal bone growth by removing calcium from bone and replacing it with calcium in bone [26]. In study by Rothenberg in 1996 in Mexico, high consumption of milk in pregnancy was accompanied by low lead level in neonates [27]. Al-Jawadi AA et al. in Iraq showed that consumption of milk and its products in pregnancy and high calcium of mother were effective in prevention of blood lead level of mother and high iron of mother has protective role against umbilical cord blood lead level [24]. Results of study by Schell CM et al. also confirm that high Vitamin D, calcium and iron of mother has protective role against lead. So, increase in two standards of deviation in iron and calcium of mother reduces neonate blood lead level to 0.77 µg/dl or reduces mean neonate blood lead level by 45% [21].
In the present study, results showed the decrease of birth weight with increase B-Pb was small and was not statistically significant. Also, there was reverse statistically significant correlation between umbilical cord blood lead level and length and head circumference that means when umbilical blood lead increases, the length and head circumference decreases. This finding is similar to result of study by Taylor CM et al. They found evidence for adverse effects of maternal B-Pb on the incidence of preterm delivery, birth weight, head circumference and crown heel length [1]. In study by Ramadan ELSawi I et al., there was significant difference between reduction of Hb level, gestational age, weight, length, head circumference and high lead level compared with low lead level in neonates [12]. In study by Falcon N et al., there was no significant correlation between umbilical cord blood lead and these two variables [15]. West WL et al., in their study didn’t obtain significant relationship between mother’s lead level and birth weight in neonates above 2500 g and below 2500 g [16]. In study by Zhu M et al. on mothers with low lead level below 10 µg/dl, umbilical cord blood lead levels of between 5 and 10 µg/dl had relationship with reduction of neonate weight by 61-87g [13].
Based on findings of the study, there was no statistically significant relationship between gender of neonate, gestational age, job and education of mother and blood lead level of neonates. In study by Patel AB and Prabhu AS in India, there was significant relationship between gestational age and umbilical cord blood lead level. In this way, increase of mean umbilical cord blood lead level to 1 µg/ dl, gestational age was reduced by one week. Also, there was no significant relationship between education of mother and living in painted old houses and umbilical cord blood lead level [28]. In study by Zhu M et al., there was no relationship between lead level and premature birth and Small for Gestational Age (SGA) [13].
Limitation
Limitation of study was the small sample size and lack of assessing maternal nutritional parameters.
Conclusion
Maternal lead level caused adverse effects on birth outcomes. So, screening of pregnant women about concentration of the blood lead and giving information to pregnant women on sources of lead, how to prevent exposure and nutrition is necessary.
[1]. Taylor CM, Golding J, Emond AM, Adverse effects of maternal lead levels on birth outcomes in the ALSPAC study: a prospective birth cohort studyBJOG 2015 122:322-28. [Google Scholar]
[2]. Rahman A, Hakeem A, Blood Lead Levels during Pregnancy and Pregnancy Outcome in Karachi WomenJ Pak Med Assoc 2003 53:529-33. [Google Scholar]
[3]. Centers for Disease Control and PreventionEttinger AS, Wengrovitz AG, Portier C, Brown MJ, Guidelines for the identification and management of lead exposure in pregnant and lactating women 2010 cited 2017 May 14Atlanta, GACenters for Disease Control and PreventionAvailable from: https: //www.cdc.gov/nceh/lead/publications/leadandpregnancy2010.pdf [Google Scholar]
[4]. Popko J, Olszewski S, Hukałowicz K, Markiewicz R, Borawska MH, Szeparowicz P, Lead, Cadmium, Copper and Zinc Concentrations in Blood and Hair of Mothers of Children with Locomotor System Malformations PolishJournal of Environmental Studies 2003 12(3):375-79. [Google Scholar]
[5]. Zentner LE, Rondo PH, Mastroeni SS, Lead Contamination and anthropometry of the New born BabyJournal of tropical Pediatrics 2006 52(5):369-71. [Google Scholar]
[6]. ATSDR (Agency for toxic substance and Disease Registry)Toxicological profile for lead Atlanta: US. Department of Health and human service 2007 cited 2017 May 14Available from: https://www.atsdr.cdc.gov/toxprofiles/tp13-p.pdf [Google Scholar]
[7]. Lozoff B, Jimenez E, Wolf AW, Angelilli ML, Zatakia J, Jacobson SW, Higher infant blood lead levels with longer duration of breast feedingJ Pediatr 2009 155(5):663-67. [Google Scholar]
[8]. Cleveland LM, Minter ML, Cobb KA, Scott A, German VF, Lead Hazards for Pregnant women and children: Part 2AJN 2008 108(11):40-47. [Google Scholar]
[9]. U.S.Preventive Services Task ForceScreening for elevated Blood Lead Levels in Children and Pregnant women: Recommendation StatementAmerican Family Physician 2007 76(5):691-94. [Google Scholar]
[10]. American College of Obstetricians and GynecologistsLead screening during pregnancy and lactation. Committee opinion number 533.2012cited 2017 May 14Available from: http://www.acog.org/-/media/Committee-Opinions/Committee-on-Obstetric-Practice/co533.pdf?dmc=1&ts=20150301T0410069060 [Google Scholar]
[11]. El-Dee K SEM, Mohammed ZT, Fathy HM, Mohamed SA, Lead Levels in Maternal and Newborns Blood and Hair and Their Impact on Neonatal Anthropometric MeasurementsBull. Egypt. Soc. Physiol. Sci 2013 33(1):107-22. [Google Scholar]
[12]. Ramadan ELSawi I, Helmy ELSaid M, Umblical cord-blood lead levels and pregnancy outcomeJournal of Pharmacology and Toxicology 2013 8(3):98-104. [Google Scholar]
[13]. Zhu M, Fitzgerald EF, Gelberg KH, Lin SH, Druschel CHM, Maternal Low-Level Lead Exposure and Fetal GrowthEnvironmental Health Perspectives 2010 118(10):1471-75. [Google Scholar]
[14]. Chen PC, Pan I, Wang JD, Parental Exposure to Lead and Small for Gestational Age BirthsAmerican Journal of Industrial Medicine 2006 49:417-22. [Google Scholar]
[15]. Falcon M, Vinas P, Luna A, Placental Lead and outcome of PregnancyToxicology 2003 185(1-2):59-66. [Google Scholar]
[16]. West WL, Knight EM, Edwards CH, Manning M, Spurlock B, James H, Maternal Low Level Lead and Pregnancy OutcomesJ. Nutr 1994 124:981S-986S. [Google Scholar]
[17]. Ratzon R, Sheiner E, Shoham-Vardi I, The role of prenatal care in recurrent preterm birthEur J Obstet Gynecol Reprod Biol 2011 154:40-44. [Google Scholar]
[18]. Alijahan R, Hazrati S, Mirzarahimi M, Pourfarzi F, Ahmadi Hadi P, Prevalence and risk factors associated with preterm birth in Ardabil, IranIran J Reprod Med 2014 12(1):47-56. [Google Scholar]
[19]. Golestan M, Akhavan Karbasi S, Fallah R, Prevalence and risk factors for low birth weight in Yazd, IranSingapore Med J 2011 52(10):730-33. [Google Scholar]
[20]. Roudbari M, Yaghmaei M, Soheili M, Prevalence and risk factors of low birth weight infants in Zahedan, Islamic Republic of IranEastern Mediterranean Health Journal 2007 13(4):838-45. [Google Scholar]
[21]. Schell LM, Denham M, Stark AD, Gomez M, Rovenscroft J, Parsons PJ, Maternal blood lead concentration, diet during pregnancy, and anthropometry predict neonatal blood lead in a socioeconomically disadvantaged populationEnvironmental Health perspectives 2003 111(2):192-200. [Google Scholar]
[22]. Shannon M, Severe Lead Poisoning in PregnancyAmbulatory Pediatrics 2003 3(1):37-39. [Google Scholar]
[23]. Al-Saleh I, Shinwaria N, Mashhour A, El Din Mohamed G, Rabah A, Heavy metals (lead, cadmium and mercury) in maternal, cord blood and placenta of healthy womenInternational Journal of Hygiene and Environmental Health 2011 214:79-101. [Google Scholar]
[24]. Al-Jawadi AA, Al-Mola ZWA, Al-Jomard RA, Determinants of maternal and umbilical blood lead levels: across-sectional study, Mosul, IraqBMC Research Notes 2009 2:47 [Google Scholar]
[25]. Lee MG, Chun OK, Song WO, Determinants of the Blood Lead Level of US Women of Reproductive AgeJournal of the American College of Nutrition 2005 24(1):01-09. [Google Scholar]
[26]. Potula V, Report from the CDC: is lead exposure a risk factor for bone loss?J Women Health 2005 14:461-64. [Google Scholar]
[27]. Rothenberg SJ, Karchmer S, Schnaas L, Perroni E, Zea F, Salinas V, Maternal influences on cord blood lead levelsJ Expo Anal Environ Epidemiol 1996 6(2):211-27. [Google Scholar]
[28]. Patel AB, Prabhu AS, Determinants of Lead Level in Umbilical Cord BloodIndian Pediatrics 2009 46(17):791-93. [Google Scholar]