Multimorbidity, the co-occurrence of two or more chronic conditions simultaneously, in an individual is increasingly becoming a global public health challenge [1]. Once thought to be a challenge for affluent countries alone, multimorbidity has emerged as the leading cause of death and disability in many Low and Middle Income Countries (LMICs) especially with socio-economic development and westernization of lifestyle [2]. However, multimorbidity is still understudied among the PLHIV; particularly in the LMICs which have a high burden of HIV/AIDS [3].
Multimorbidity has several adverse clinical implications because of reduced functional status and quality of life, and increased adverse drug events, medical costs, disability, and mortality [4]. HIV has become a chronic disorder enabling PLHIV to live longer after the arrival of ART [5]. This has lead to an increased risk of multimorbidity and an increased likelihood of Non-Communicable Diseases (NCDs) and other diseases [6,7]. HIV is associated with complex inter-linkages between HIV/AIDS and NCDs causing higher NCDs among PLHIV [8]. NCDs and other non-AIDS related events (coronary heart disease and myocardial infarction and subclinical atherosclerosis) have become the major causes of death in PLHIV in developing countries [9,10]. HIV infection and ART are also independent risk factors for diabetes, atherosclerosis, low bone density and a number of other chronic diseases [3]. Consequences of long term ART toxicities include, a state of chronic inflammation, lifestyle related risks for the disease and ageing [9]. The co-existence of multimorbidity in PLHIV is even more serious as they both significantly increase the health care utilization and out of pocket expenditures. Such catastrophic expenditures usually drive the patients and their families below poverty line [10].
A total number of 2.09 million and 103, 859 people were estimated to be living with HIV in India and the state of Odisha respectively [11]; Such dramatic numbers of PLHIV, demand immediate attention. Till now, there had been limited studies in India exploring multimorbidity among HIV/AIDS patients to the best of our knowledge. Additionally, considering the significant number of PLHIV in the state of Odisha, it is important to understand the patterns in the region. Hence, this study was conceived as an exploratory study with the objectives of finding the prevalence and the patterns of multimorbidity among PLHIV in Odisha, India.
Materials and Methods
This was a cross-sectional exploratory study conducted in one of the government ART centres of Bhubaneswar, Odisha, Eastern India, from November 2013 to December, 2013. This ART centre was chosen from eight ART centres of Odisha, because it caters to the maximum number of HIV/AIDS patients from the five neighbouring districts. Only those adult patients who had been receiving ART for more than one year were included. However, those who were unable to respond due to diminished cognitive abilities or the severity of the disorders and/or who were unwilling to consent for the study were excluded.
Being an exploratory study, there were no prior studies available with a prevalence estimate. We decided to include every fifth patient who attended the ART clinic and met the inclusion criteria considering the average daily patient load. By doing so, a sample size of 180 patients was calculated. Assuming a non-response rate of 20%, we finally decided to keep the sample size as 220, out of which 197 gave consent for taking part in the study.
Study Tool
Patient information was collected by four trained nurses using a structured questionnaire translated in the local language. The self-reported responses were corroborated with the information available from the patient’s health cards. Orientation and supportive supervision were given to the nurses to maintain data quality. The questionnaire comprised of five sections covering information on socio-demographic profile, HIV-ART status and confirmation date of being HIV positive, CD4 count, weight, functional status, co-existing chronic conditions (multimorbidity) and opportunistic infections. Any disease or condition that was present in a patient apart from HIV was treated as a co-morbid condition. We developed the table of diseases from patient chart listing and literature review on multimorbidity and HIV/AIDS, finally including those diseases which were of clinical significance. Under co-morbidities, variables like gastro-intestinal conditions included ulcer diseases like gastro-oesophageal reflux disease, chronic duodenal ulcer, gastric ulcer, and peptic ulcer disease while neural disorders comprised of neuropathy, hypomania, mania, depression, cyclothymia, mood disorder, bipolar disorder and dysthymia. Opportunistic infections included viral (Cytomegalovirus and Herpes Simplex Virus), bacterial (Mycobacterium avium and Salmonella) and fungal infections (Candidiasis, Coccidiomycosis, Cryptococcosis, Histoplasmosisand Pneumocystis cariniiinfection).
Statistical analysis
The data analysis was performed using Statistical Packages for the Social Sciences (SPSS) software version 20.0.
Results
[Table/Fig-1] shows the socio-demographic and the clinical details of the study participants. Out of 197, most were males (65.0%), from general caste (83.2%), had secondary level education (45.2%), employed (64.5%) and married (74.6%). The mean age of the sample was 36.1 {Standard Deviation (SD) 8.6} years. The median household income was 4000 (500-55,000) INR. Alcohol consumption (21.9%) and smoking (12.5%) were prevalent only among males; and from them, 31.0% were daily consumers of alcohol while 45.7% were current smokers.
Socio-demographic and clinical details of the study participants (N=197).
| Variable | Category | N(%) |
|---|
| Sex | Male | 128(65.0) |
| Female | 67(34.0) |
| Other | 2(1.0) |
| Caste | SC/ ST | 33(16.8) |
| Non-SC/ ST | 164(83.2) |
| Education | Illiterate | 25(12.7) |
| Primary | 60(30.5) |
| Secondary | 89(45.2) |
| College and above | 23(11.7) |
| Occupation | Employed | 127(64.5) |
| Unemployed | 70(35.5) |
| Marital status | Married | 147(74.6) |
| Widowed/divorcee/ separated | 34(17.3) |
| Single | 16(8.1) |
| History of alcohol consumption | Yes | 29(14.7) |
| No | 168(85.3) |
| Frequency of alcohol consumption | Rarely | 5(17.2) |
| Once in a month | 12(41.4) |
| Weekly | 3(10.3) |
| Daily | 9(31.0) |
| History of smoking | Never | 162(82.2) |
| Current smoker | 16(8.1) |
| Past smoker | 19(9.6) |
| CD4 count (cells/pl) | ≤; 200 | 107(54.3) |
| >200 | 90(45.7) |
| Mean duration since diagnosis | ≤1 year | 37(18.8) |
| 1-3 years | 101(51.2) |
| >3 years | 59(30.0) |
Among all, around half of the patients (51.2%) were on ART since one to three years. More than half (54.3%) were having CD4 cell counts less than 200 cells/µl and average weight of 47.9 (SD 8.9) kilograms.
The prevalence of different co-existing conditions in patients with multimorbidity is displayed in [Table/Fig-2].
Prevalence of chronic conditions (multimorbidity) among study participants (N=197).
| Chronic condition | N(%*) |
|---|
| Pulmonary tuberculosis | 56(28.4) |
| Gastro-intestinal conditions1 | 14(7.1) |
| Neural disorders2 | 10(5.1) |
| Anaemia | 10(5.1) |
| Hypertension | 5(2.5) |
| Sexually Transmitted Infection (STI) | 4(2.0) |
| Hepatitis B infection | 3(1.5) |
| Hepatitis C infection | 2(1.0) |
| Diabetes | 2(1.0) |
| Asthma-lung diseases | 1(0.5) |
| Arthritis | 1(0.5) |
| Others | 10(5.1) |
the percentages do not add up to 100 as the conditions are not mutually exclusive
Gastro-intestinal conditions include gastro-esophageal reflux disease, chronic duodenal ulcer, gastric ulcer, and peptic ulcer disease
Neural disorders include neuropathy, hypomania, mania, depression, cyclothymia, mood disorder, bipolar disorder, and dysthymia.
Out of 197, 47.7% (95% CI 41.0% to 55.0%) had multimorbidity. Overall, pulmonary tuberculosis (28.4%) was the most common co-existing chronic condition followed by ulcer diseases (7.1%), neural disorders (5.1%) and hypertension (2.5%). The most common dyad (combination of two diseases with HIV) pulmonary tuberculosis with ulcer diseases (N=3).
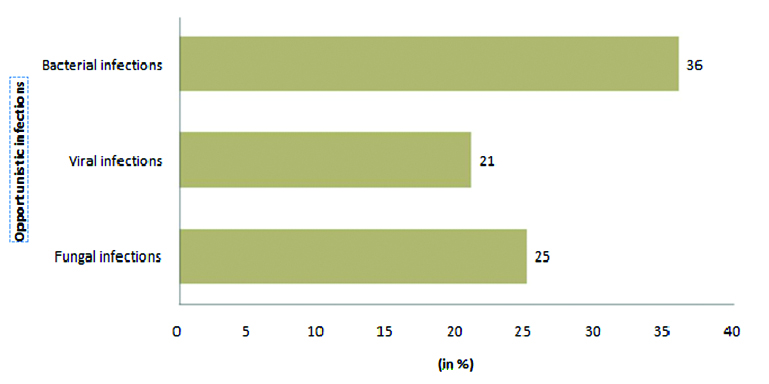
Of the total, 48.7% had opportunistic infections. [Table/Fig-3] depicts the prevalence of individual opportunistic infections. Many participants also experienced a multitude of symptoms and side effects other that co-morbidities due to the prolonged intake of ART; among which the most common was vomiting and nausea (16.2%). Other symptoms included pruritus, toothache, anorexia, bodyache, fatigue, weakness, haemoptysis, leucorrhoea, sleeplessness, and headache (<1%).
Opportunistic infections among the study participants (N=197).
*The percentages do not add up to 100 as the conditions are not mutually exclusive
Discussion
Our study aimed to find the prevalence of multimorbidity among HIV/ AIDS patients being treated in one of the government ART centers of Bhubaneswar, Odisha, Eastern India. Since, there is scarce literature examining the prevalence and patterns of multimorbidity among PLHIV; we decided to conduct an exploratory study among 197 adults who were taking ART since one year or more. Odisha has comparable health indicators with the rest of the country and Bhubaneswar being the capital city hence, was chosen as the study area.
In our study, majority were young males. Such a striking representation of men in the ART clinics was also seen in other Indian studies [12]. However, this may not represent the actual proportion of women suffering from AIDS because of multiple reasons. Firstly, the women might be hesitant in seeking optimum health care due to fear of stigma, ostracism and gender bias. The national level statistics published by National AIDS Control Organization (NACO) also reported that 89% of the AIDS affected patients belong to the age of 15-44 years [11]. Also, a younger age group is sexually more active and economically more productive requiring frequent travels and possibly contributing to the high prevalence of HIV in this group [13]. Another intriguing finding from our study was the education status. These findings were similar to other studies done in the Indian context where the majority of the people were literate [14]. It is assumed that less education can lead to less awareness about HIV/other sexually transmitted diseases and their mode of transmission. However, the lack of optimum sex education provided in Indian schools, particularly public schools might be a reason of low awareness and high prevalence of HIV [15].
What was worth noting that despite having HIV, a considerable proportion of the study participants were alcoholics and smokers; a reason attributable to the large number of males in the sample. These findings were similar to other studies from India as well across the world, where HIV positive males were more prone to addictive substances [16]. However, this indicates the lack of counselling of these patients by the counsellors and the health professionals and/ or the lack of compliance of the HIV patients.
In this study, the prevalence of multimorbidity was 47.7% (95% CI 41% to 55%) which is considerably a lot higher as compared to other studies conducted in India as well as across the world [17]. In a study conducted by Munshi Su et al., in Bangladesh, the prevalence of co-infections with HIV was found to be 18.64 % [18]. This is significantly low as compared the findings from the current study. Situation is alarming as nearly half of the PLHIV is diagnosed with multimorbid condition. In the previous studies, in India and abroad, this is commonly found in the range of one-third of the PLHIV. This issue becomes more important in light of the usual low health seeking behaviour among HIV positive people and the health providers missing the diagnosis of other co-existing conditions among the HIV positive people in place of HIV. The co-existing chronic diseases which were most common were (PTB, APD and hypertension) were consistent with findings from other studies [19].
In our study, the most common co-existing chronic condition was pulmonary tuberculosis (28.4%). Other studies from India have also reported high prevalence of pulmonary tuberculosis in HIV positive people [20]. A possible reason could be the young age of the population where tuberculosis is very common, mainly as a result of habits like smoking and indulging in outdoor occupations like manual labour where the chances of infection are the highest [21]. The knowledge of tuberculosis among HIV patients becomes very imperative as in a study conducted by Arora et al., 70.0% did not know the method of transmission of tuberculosis [22].
The high prevalence of multimorbidity among HIV positive people in this population is worth noting as with the advent of ART, their life span has increased and they have more chances of dying because of non-HIV related co-morbid conditions than due to HIV. Hence, patients should not only be counselled regarding the HIV infection but also about the existing co-morbidities [20]. Preventive measures aiming at behavioural change and maintaining a healthy lifestyle including timely screening tests should be incorporated at the primary levels of health care [23].
Another interesting finding which emerged from the study was the high prevalence of opportunistic infections despite undergoing ART. Usually, the prevalence of opportunistic infections decreases with ongoing ART [24,25]. However, in this case the patients who had high prevalence of opportunistic infections, could have been in the late stages of AIDS in which ART becomes refractory [26,27].
Many implications can be drawn from the findings of this study. For example, the health providers can utilize the ART visits by the patients as counselling sessions. For example, counselling can be given on: 1) medicine compliance issues; 2) avoiding dangerous habits like alcohol, tobacco and other substances; 3) dangerous drug interactions and side effects. Moreover, apart from medications, additional focus can also be given towards maintaining a healthy lifestyle (e.g., balanced diet, physical exercise, stress reduction and proper sleep routine).
This is the first study to report the prevalence and patterns of multimorbidity among HIV positive people in India using simple count of individual chronic conditions. Also, the first documented evidence about the pattern of multimorbidity in PLHIV from Odisha, India.
Being a single centre study, our findings may not be generalizable to study settings or geographic regions. Nonetheless, being an exploratory study involving HIV positive people, conducting the study in an ART centre deemed fit. Despite this, the findings obtained from the study can be used to develop a preliminary evidence base for the prevalence of multimorbidity among HIV positive people at a large ART centre. Also, since the collected data was self-reported, there might be chances of recall bias. However, data were cross-examined from the chart lists and health cards to the maximum possible extent to compensate for the recall bias. Even though self-reporting of data gives compromised information, it has been seen that it provides almost near-true results as compared to more complex measurement approaches [28]. Additionally, since in HIV research it is usually not possible to quantify the duration of HIV infection, we considered the duration of diagnosis as the length of time as the best approximation. Likewise, no information was available regarding the medication tolerance which needs to be addressed in future studies. Ideally, a control uninfected group could have given better prevalence estimates; which our study lacked. However, Goulet et al., reported from the findings of their study on a large sample that PLHIV are more likely to have co-morbidities as compared to their uninfected counterparts [29].
Conclusion
The study concludes that the prevalence of multimorbidity in HIV positive people is very high despite their young age. It was beyond the scope of this study to elicit the causes of individual co-morbid conditions. There is a pressing need for more epidemiological studies for quantifying multimorbidity and understanding its broad patterns and its associated factors in the HIV positive people at the population level. Furthermore, future studies should be directed at finding how the HIV positive people with multimorbidity are accessing health care and how providers are meeting the health care needs of this population. There is a need for the health systems to incorporate the management of complex chronic conditions in the routine treatment of AIDS and look past the traditional biochemical tests to determine the complexity of the disease. This would help in scaling up the health care delivery system through proper policy actions and devise tangible guidelines to conform ourselves to the changing needs of care for the PLHIV.
Funding
The authors did not receive any kind of financial support from any organization or institute.
Ethical Approval
The study protocol was approved by the Institutional Review Board (IRB) of Indian Institute of Public Health, Bhubaneswar (IRB No. IIPHB/ IEC/ 2013/ 003). Informed consent was confirmed by the IRB. Complete confidentiality and anonymity was ensured to all the study participants. The study was explained in detail to all the participants who were given full freedom to withdraw from the study if needed.
*the percentages do not add up to 100 as the conditions are not mutually exclusive
1Gastro-intestinal conditions include gastro-esophageal reflux disease, chronic duodenal ulcer, gastric ulcer, and peptic ulcer disease
2Neural disorders include neuropathy, hypomania, mania, depression, cyclothymia, mood disorder, bipolar disorder, and dysthymia.