Visceral Leishmaniasis in an Immunocompromised Patient: Diagnostic Bone Marrow Cytomorphology
Manjari Kishore1, Garima Baweja Madaan2
1 Senior Resident, Department of Pathology, PGIMER, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
2 Consultant Pathologist, Department of Pathology, PGIMER, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manjari Kishore, A1, 1/10A, Sector-5, Rajender Nagar, Sahibabad, Ghaziabad-201005, Uttar Pradesh, India.
E-mail: drmanjarik@gmail.com
Immunodeficiency, Megakaryocytes, Pulmonary tuberculosis
Dear Editor,
Visceral leishmaniasis (VL), commonly known as Kala-azar is usually found throughout the tropical and subtropical regions of the world [1]. The usual haematological manifestations are pancytopenia, myelofibrosis, myelodysplasia and haemophagocytosis [2]. We present a case of an immunocompromised female who initially came to hospital with features of tuberculosis but on further evaluation she was diagnosed with heavy infestation of bone marrow with Leishmania Donovan (LD) bodies.
A 35-year-old female, resident of northern India (non-endemic zone of VL) presented to hospital with complaints of fever and cough for two months which was intermittent in nature with evening rise of temperature. She also complained of abdominal pain, decreased appetite and loss of weight. On per abdominal examination, marked splenomegaly was noted. Ultrasound abdomen also showed evidence of marked splenomegaly and mild hepatomegaly.
The patient was a known case of Human Immunodeficiency Virus infection (HIV) and after hospitalisation, she was also found to have pulmonary tuberculosis with strong Montaux test and raised ESR. Her complete blood count revealed Haemoglobin of 8.5 gm/dl, leucopenia with total leucocyte count of 1200/µl; however, her platelet count was adequate on smear.
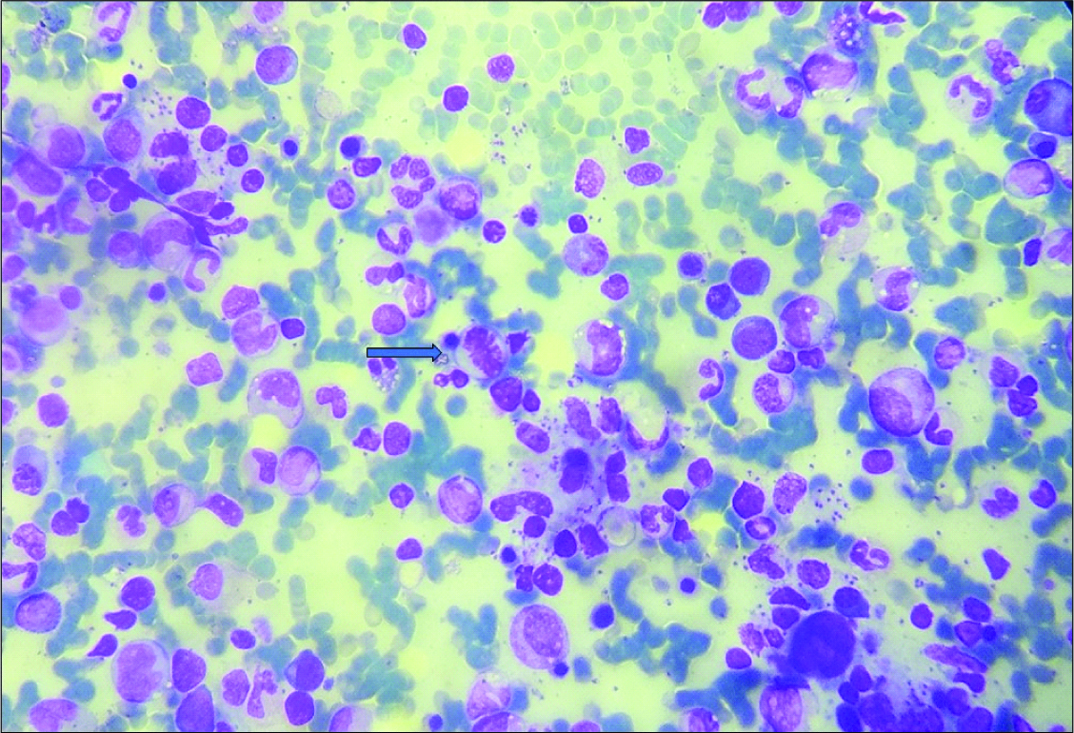
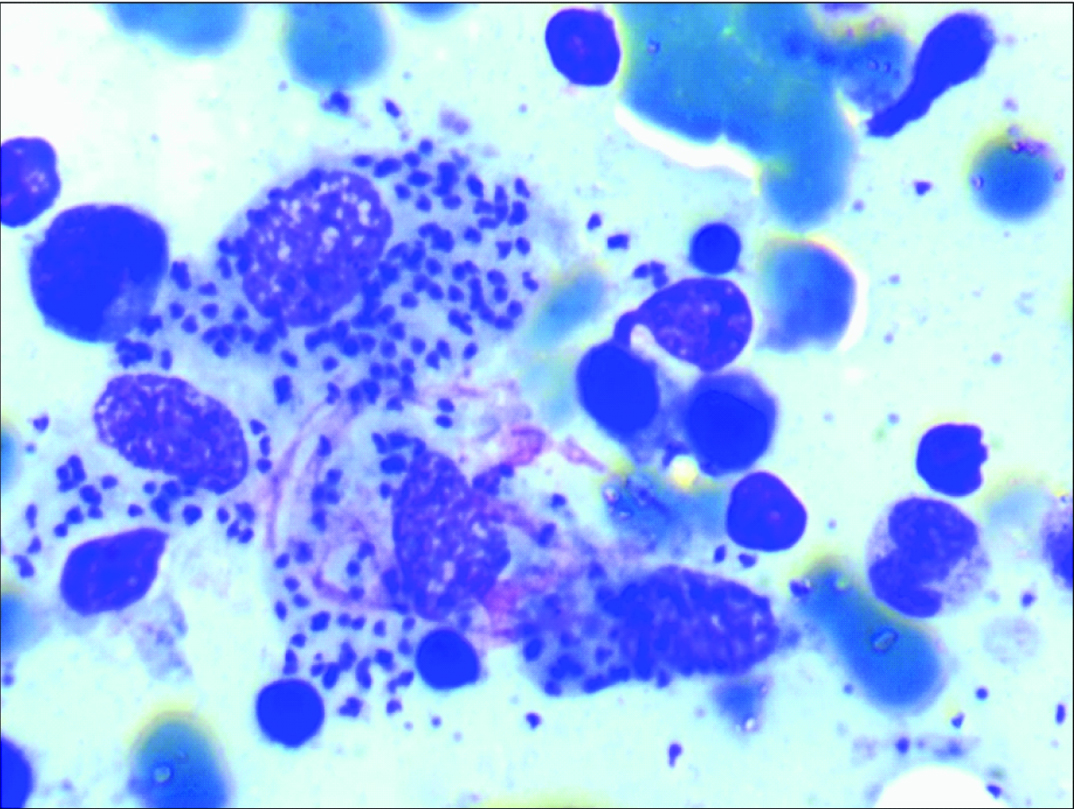
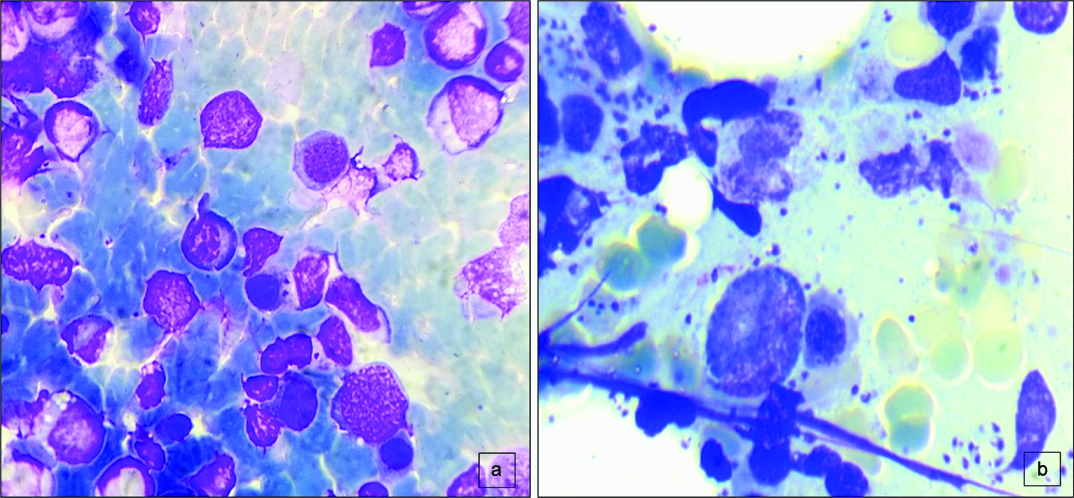
Bone marrow examination was advised and smears showed high cellularity with a Myeloid- Erythroid ratio (M:E ratio) of 1.2:1. Erythroid series cells showed normoblastic reaction with features of mild dyserythropoeisis. Myeloid series cells were seen in all stages of maturation with mild prominence of eosinophils and its precursors. Megakaryocytes were adequate in number and were functional. Plasma cells were prominent constituting 5-6% of all nucleated cells. Scattered histiocytes were noted with numerous LD bodies lying intracellularly. Many extracellular LD bodies were also seen. LD bodies were noted in myeloid cells, erythroid cells and few megakaryocytes [Table/Fig-1,2 and -3]. No granuloma or any atypical cells were noted. RK39 antibody test was also found to be positive in this case. An impression of “VL with extensive bone marrow involvement” was made in an immunocompromised individual.
Bone marrow aspirate smear showing haematopoietic cells along with numerous intracellular and extracellular LD bodies (Giemsa 10X). A mitotic figure is also noted (arrow).
High power view showing extracellular and intracellular LD bodies within the myeloid and erythroid cells (Leishman 40X).
a) BMA showing LD bodies in erythroid cells (Giemsa 20X); b) LD bodies seen in Megakaryocyte (Leishman 20X).
VL is caused by flagellated protozoan, Leishmania donovani and is transmitted by the bite of sandfly, Phlebotomous [1-3]. Its non-flagellate form is widely distributed in the macrophages of reticuloendothelial system. The patients usually present with fever, malaise and severe splenomegaly. The overall incidence and prevalence of kala-azar cases per year are 0.5 and 2.5 million, respectively, of which more than 90 percent of the world’s VL cases are from the Indian subcontinent [1,4]. A further increase in incidence of VL as an opportunistic infection is noted in India after the emergence of AIDS epidemic [4].
The diagnosis of VL is made by demonstration of the parasite by microscopic examination of material obtained by bone marrow aspiration and biopsy [5]. Extracellular location is also commonly noted. LD body is small in size and has an oval to round shape with nucleus and a kinetoplast. In heavily parasitized patients, LD bodies can be demonstrated in buffy coat preparation of blood.
Leishmania HIV coinfection is a major concern in India, as there can be wide dissemination of organisms to various other organs and patients can present with atypical features. Previously, few cases of association of VL with TB and AIDS have been reported where VL was found masquerading as myelodysplasia and even pulmonary tuberculosis [2,4].
Our case demonstrated the clinical utility of bone marrow examination in an immunocompromised adult female patient with HIV positivity. The prompt recognition of the cytomorphological features of LD bodies in BMA smears helped in providing an early diagnosis of VL. Apart from that, tuberculosis was also diagnosed in the same patient with other ancillary techniques. Hence, the coinfection of TB and VL in HIV positive patient with heavy infestation of bone marrow with LD bodies makes this a rare presentation.
[1]. Desjeux P, Alvar J, Leishmania/HIV co-infections: Epidemiology in EuropeAnn Trop Med Parasitol 2003 97:3-15. [Google Scholar]
[2]. Kopterides P, Halikias S, Tsavaris N, Visceral leishmaniasis masquerading as myelodysplasiaAm J Hematol 2003 74:198-99. [Google Scholar]
[3]. Agarwal S, Narayan S, Sharma S, Kahkashan E, Patwari AK, Hemophagocytic syndrome associated with visceral leishmaniasisIndian J Pediatr 2006 73:445-46. [Google Scholar]
[4]. Yaduvanshi A, Jain M, Jain SK, Jain S, Arora S, Visceral leishmaniasis masquerading as tuberculosis in a patient with AIDSPostgrad Med J 1999 75:732-34. [Google Scholar]
[5]. Kumar PV, Vasei M, Sadeghipour A, Sadeghi E, Soleimanpour H, Mousavi A, Visceral Leishmaniasis: Bone marrow biopsy findingsJ Pediatr Hematol Oncol 2007 29:77-80. [Google Scholar]