Case Report
A 52-year-old patient with a non-contributory medical history reported to the Department of Conservative Dentistry and Endodontics, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India, with pain in upper right back tooth region. The patient gave a history of pain for past two weeks. Oral and radiographic examination revealed an impacted right maxillary third molar (tooth number 18) and Class II dental caries involving distal aspect of right maxillary second molar (tooth number 17) with no evidence of periapical radiolucency [Table/Fig-1a]. Based upon the clinical and radiographic findings, the diagnosis was established as impacted in tooth number 18 and acute irreversible pulpitis in tooth number 17. Patient was advised analgesics and extraction of tooth number 18 followed by endodontic therapy in tooth number 17 (as presence of tooth number 18 was compromising on the pre-endodontic restoration and seal in tooth number 17). A week later the patient was scheduled for endodontic therapy in tooth number 17.
a) Preoperative radiograph; b) Access cavity preparation; c) Working length determination; d) Obturation radiograph.
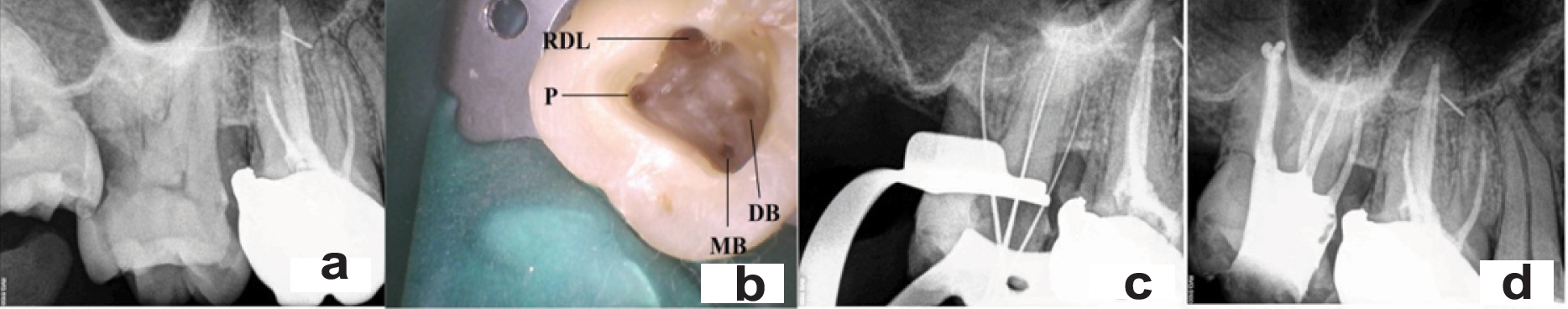
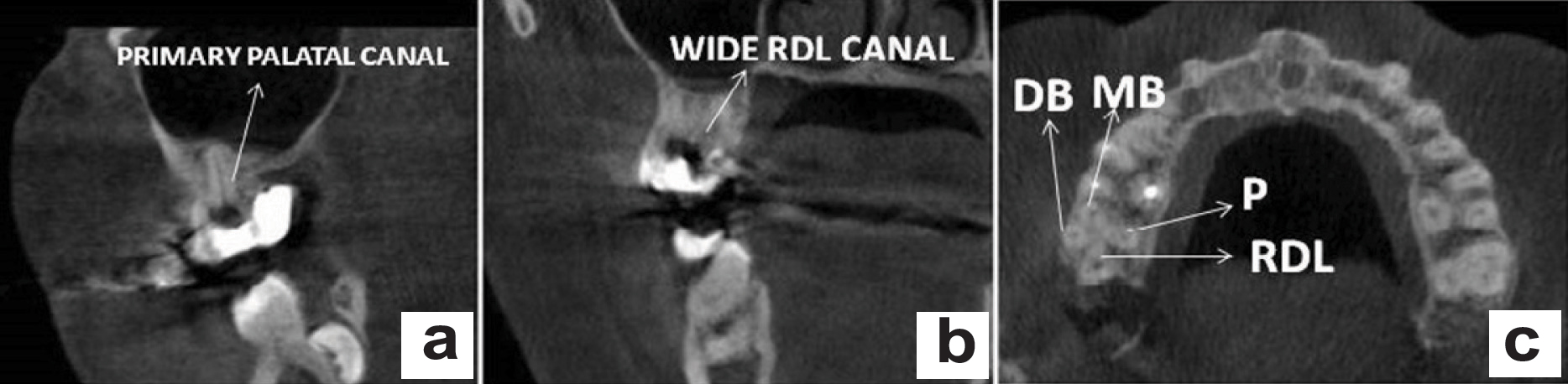
Clinically, it was noticed that the second molar showed an unusual occlusal morphology and an obscure radiographic image of the roots [Table/Fig-1a]. Local anaesthesia was administered. Caries was excavated and restored with composite as pre-endodontic restoration under rubber dam isolation. Access opening was done and three canals (mesiobuccal-MB, distobuccal-DB and palatal canal-P) were negotiated. A fourth root canal orifice in the distopalatal aspect of the pulpal floor was observed on detailed visualization under the dental operating microscope [Table/Fig-1b]. The working length was determined using Root ZX II (J. Morita, Tokyo, Japan) and confirmed radiographically. Radiographic examination revealed the presence of an accessory root in palatal aspect of tooth number 17 [Table/Fig-1c]. After irrigation with 2.5% sodium hypochlorite (NaOCl), the canals were dried with paper points and filled with 0.2% chlorhexidine gluconate gel (Laboratorios KIN SA, Barcelona, Spain) and temporized. Hence, to further confirm the presence of RDL, CBCT was taken to visualize the unusual anatomy of tooth number 17 [Table/Fig-2] [1].
CBCT images: a) Coronal section showing primary palatal canal; b) Coronal section showing wide radix distolingualis canal; c) Axial section showing four root canals in 17.
During the second visit, after confirming the anatomy with CBCT, the canals were instrumented with M two rotary system (VDW, Munich, Germany) to size 25/06 in MB and DB canals and size 35/06 in P canal. Enlargement was done upto # F5 ProTaper Universal rotary system (Dentsply-Maillefer, Ballaigues, Switzerland) in RDL root because the initial apical size was 25 in this canal. The wide distolingual canal in a case of RDL which is evident in the preoperative radiograph was rather unusual. Copious irrigation with 2.5% NaOCl was performed during the instrumentation phase. Then, after drying the canals with paper points, master cone radiograph was taken and obturated using lateral condensation technique in the three primary canals. Whereas, in the RDL root, thermo plasticized obturation was done with Elements B obturating system (Kerr-dental Plymouth, Massachusetts) in order to achieve a three dimensional obturation of the pulp space [Table/Fig-1d]. F5 size was used as the master cone for down pack in the RDL root followed by a back fill. AH plus (Dentsply, Maillefer, Ballaigues, Switzerland) was used as the sealer. Finally, the cavity was restored with composite as core material followed by Porcelain Fused to Metal (PFM) crown.
Discussion
Undetected extra roots or canals are recognized as a major reason for failure of root canal treatment according to Vertucci FJ et al., and Cantatore G et al., [2,3]. Inspite of the various clinical and diagnostic aids available, the exact location of the orifice and the number of root canals varies in any individual tooth. Cohen S and Burns RC stated that extra canals are often left untreated as they are not located [4]. A thorough knowledge of the anatomic morphology, careful attention in locating additional root canals, appropriate use of magnification devices is necessary to perform successful endodontic therapy.
The incidence of second palatal root in maxillary second molar teeth has been reported to be only 1.4%, according to Pecora JD et al., (1992). Among the 370 maxillary molars examined in the study, the fourth canal was located mainly in relation to the mesiobuccal root [5].
When a maxillary second molar presents with an additional root, literature has represented three common variations - an accessory palatal root, an accessory buccal root, an accessory mesial root or distal root. Though, the exact aetiology is not known, it could be related to the splitting of Hertwigs epithelial root sheath to form two similar roots or by folding of the Hertwigs epithelial root sheath that develops into a separate accessory root by exogenic or endogenic factors during root development [6].
When complex canal anatomies are detected, clinically successful endodontic therapy can be established respecting technical and biological principles. The most important diagnostic aids in endodontics include conventional radiographs, dental operating microscope and CBCT. To locate additional canals in endodontic diagnosis, to determine the effectiveness of cleaning and shaping, obturation and guttapercha removal, CBCT is widely used in Endodontics. It enables highly accurate visualization of the external as well as the internal anatomy and obtains multiple slices of roots and their respective root canals [1,7].
The present case report discusses the endodontic management of a maxillary second molar with RDL. Although, it is a very rare situation, four rooted maxillary second molars exist.
According to Christie WH et al., RDL Type 1 maxillary molars have two widely divergent palatal roots that are often long and tortuous. The buccal roots of these teeth are often “cow-horn” shaped and less divergent. Four separate root apices are seen on the radiograph. Type 2 has four separate and parallel roots; the roots are short and have blunt apices. Type 3 has four roots; the MB, MP and DP roots are grouped together while the DB root is separate and may diverge distobuccally [8]. Barratto-Filho F et al., modified the classification and added Type 4 in which the maxillary molar has four roots and the accessory palatal root is fused with the MB root in the coronal two thirds [9].
According to Carlsen O and Alexanderson V the MP and DP accessory roots with affinity to the pronounced MP and DP parts of the crown are called radix mesiolingualis and RDL, respectively [10]. The present case report falls under Type 2 of Carlson O and Alexanderson V’s classification, but however, cannot be categorized under Christie WH et al., classification.
Libfeld H and Rotstein I reported an occurrence rate of 0.4% in a sample of 1200 teeth, presumably on the maxillary second molar, but did not mention a lower occurrence rate on the first molar [11].
Christie WH et al., reported in their retrospective study, about the low incidence of double palatal roots and found that one case could be expected in a period of three years. In 40 years of clinical practice, they found that only 14 maxillary second molars had two palatal roots [8].
In Indian population, Neelakantan P et al., examined the root and canal morphology of 220 maxillary first molars using CBCT, and found that two palatal roots have an incidence of 0.9% (2/220), whereas none of the second molars had four roots, making this case report a rare occurrence in Indian population [7].
The most common internal canal morphology of the palatal root is a single palatal root with a single root canal extending till the apical foramen [6,7,12]. Aberrant morphological changes, include distopalatal root with one root canal, which divides into two and then merges to exit through a single apical foramen [13,14].
In the present case report, during the clinical examination it was observed that the coronal morphology was unusual with an extra cusp on the distopalatal aspect making the palatal side wider than the buccal side. The presence of an accessory root was suspected by periodontal probing in the buccal cervical region that revealed the bifurcation of the roots. This morphology combined with the preoperative periapical radiograph image, raised a suspicion of an additional root in relation to the distal aspect. Alenazy MS et al., reported that based on morphological features, maxillary molars with double palatal roots usually show prominent palatal cusps, causing the crown size to be relatively larger than normal [13]. Instead of a usual palatal root shadow, a double periodontal ligament space was also visualized on the initial periapical radiograph in the present case. According to Shin SJ et al., and Ghoddusi J et al., for successful clinical management, an extra root may be suspected when double Periodontal Ligament Spaces (PDLs) are seen on one root side or if PDLs overlap over adjacent roots radiographically [15,16].
In the present case report, the initial access cavity preparation was triangular in outline. According to the laws of orifice location 1 and 2 – the MB, DB and Palatal orifices were located at the junction of the cavity walls and the floor. Careful examination of the floor with diagnostic aids (such as Loupes, Dental Operating Microscope) under adequate illumination and probing with DG-16 endodontic explorer in relation to the distopalatal aspect of the pulpal floor enabled locating two additional canal orifices [1,8]. Now the access cavity outline was modified to a rectangular or trapezoidal shape so as to establish a straight line access to the apical third of all the root canals as per Schilders mechanical objectives. The broad coronal access with the removal of the pulp stone (located in between the two additional canal orifices on the distopalatal aspect) revealed clearly the opening of a single wide canal orifice of the RDL root. According to Yang B et al., the distance between the two palatal canal orifices was greater than the distance between the two buccal canal orifices which was 2.84 mm and 2.15 mm respectively. Hence, the access cavity was modified from triangular to trapezoidal outline [17].
Benenati FW et al., suggested that the formation of palatogingival groove on the lingual aspect may indicate the presence of two palatal roots [18]. Versiani MA et al., classified four rooted maxillary second molars into Type I, II, III based on the divergence of the two separate palatal roots. The present case report can be classified under Versiani type I configuration were the palatal roots were widely divergent and longer than the buccal roots that were less divergent and cow-horn shaped [19].
CBCT was used in this case to confirm the presence of the RDL root. CBCT provides multiplanar reformation by creating 3D images in five different planar orientations namely axial, coronal, saggital, oblique and curved. CBCT is now being extensively used in endodontics for diagnosis and treatment planning; identification of unusual canal morphology; locating and assessment of periapical pathologies, root fractures, external and internal root resorption [1,6,7].
The following play an important role in identification of extra palatal roots:
Periodontal pockets/or gingival recession enables identification of palatal root bifurcations;
Palatogingival groove;
Enamel pearls located at the furcation area of two palatal roots;
Identification of external radicular aberrations by periodontal probing;
Additional pronounced cusp on the buccal or lingual surface of the crown;
Multiple periapical radiographs with root outlines not clear;
Absence of the palatal root in between the MB and DB roots in a straight angled radiograph and doubling of PDL space;
Pattern of pulp chamber floor- with two palatal roots the pulpal floor is quadrangular in shape [20].
Case reports and in vitro studies by various authors reporting morphological variations in the palatal roots of maxillary molars have been represented [Table/Fig-3, 4] [1,9,12-16,18,20] [7-11,17,19].
Maxillary molars with morphological variations in palatal roots- Case I Reports [1,9,12-16,18,20].
| Author name | Year | No.of roots | Other details |
|---|
| Martins J.N.R et al., [1] | 2013 | 4 | Two palatal roots in maxillary second molar |
| Baratto-Filho F et al., [9] | 2002 | 4 | Two separate palatal roots with distinct canals in maxillary first molar |
| Nayak G et al., [12] | 2016 | 4 | Quadrangular shaped pulp chamber floor with four orifices (MB, DB, RML, RDL) in maxillary first molar |
| Alenazy MS and Ahmad IA [13] | 2015 | 4 | Two palatal roots in maxillary second molar |
| Holderrieth S and Gernhardt CR [14] | 2009 | 3,4 | Bifurcation of the palatal canal in maxillary first and second molars |
| Shin SJ et al., [15] | 2007 | 4 | Two palatal roots in two maxillary second molars |
| Ghoddusi J et al., [16] | 2008 | 4 | Two palatal roots in maxillary second molar |
| Benenati FW [18] | 1985 | 4 | Maxillary second molar with two palatal roots and palato gingival groove |
| Rajalbandi S et al., [20] | 2013 | 4 | Two short buccal roots (MB and DB) and two long palatal roots (RML and RDL) in maxillary first molar |
Maxillary molars with morphological variations in palatal roots: In vitro studies [7-11,17,19]
| Author name | Year | No. of roots | Other details |
|---|
| Neelakantan P et al., [7] | 2010 | 1,2,3 or 4 | 425 maxillary molars, two palatal roots in 0.9 % first molars and 0% second molars |
| Christie WH et al., [8] | 1991 | 3,4 | 16 maxillary molars with two palatal roots-87.5% and 12.5% incidence in maxillary second and first molars respectively |
| Baratto-Filho F et al., [9] | 2002 | 4 | Two separate palatal roots with distinct canals in maxillary first molar |
| Carlsen O and Alexandersen V [10] | 2000 | 4 | 145 permanent maxillary molar two separate / non separate palatal roots RDL and RML(mesiolingualis) observed |
| Libfeld H and Rotstein I [11] | 1989 | 3,4 | 0.4 % incidence of two palatal roots among 1200 maxillary second molars |
| Yang B et al., [17] | 2013 | 3,4 | Two palatal roots in 14 out of 1957 maxillary molars (1.12% in maxillary second molar and 0.31% in maxillary first molar) |
| Versiani MA et al., [19] | 2012 | 4 | 25 maxillary second molars with four roots selected - size, root curvature, no.of root canals, fusion, occurrence of enamel pearls etc was examined. |
Conclusion
Although, the probability of having double palatal roots in maxillary second molars is low, this variation should be considered to establish success of endodontic therapy. It is imperative for a clinician to apply the knowledge of variation in the clinical crown anatomy and radiographic appearance to a possible aberration in root canal morphology before starting the endodontic treatment. Besides the conventional diagnostic tools, it is recommended to perform root canal treatment under the dental operating microscope as it provides proper magnification and illumination of the operating field.
[1]. Martins JNR, Quaresma S, Barbosa JM, Quaresma MC, Anderson C, Four rooted maxillary second molar confirmed with cone beam computed tomography-a case reportGiormale Italiano di Endodonzia 2013 27(1):38-44. [Google Scholar]
[2]. Vertucci FJ, Root canal morphology and its relationship to endodontic proceduresEndod Top 2005 10:3-29. [Google Scholar]
[3]. Cantatore G, Berutti E, Castellucci A, Missed anatomy: Frequency and clinical impactEndod Top 2006 15:3-31. [Google Scholar]
[4]. Cohen S, Burns RC, Pathways of the pulp 1998 7th edMissouriMosby [Google Scholar]
[5]. Pecora JD, Woelfel JB, Sousa Neto MD, Issa EP, Morphology study of the maxillary molars part II: Internal anatomyBraz Endod J 1992 3(1):53-57. [Google Scholar]
[6]. Ahmed HM, Abbott PV, Accessory roots in maxillary molar teeth: A review and endodontic considerationsAust Dent J 2012 57(2):123-31. [Google Scholar]
[7]. Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL, Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian populationJ Endod 2010 36(10):1622-27. [Google Scholar]
[8]. Christie WH, Peikoff MD, Fogel HM, Maxillary molars with two palatal roots: A retrospective clinical studyJ Endod 1991 17(2):80-84. [Google Scholar]
[9]. Baratto-Filho F, Fariniuk LF, Ferreira EL, Pecora JD, Cruz-Filho AM, Sousa-Neto MD, Clinical and macroscopic study of maxillary molars with two palatal rootsInt Endod J 2002 35(9):796-801. [Google Scholar]
[10]. Carlsen O, Alexandersen V, Radix mesiolingualis and radix distolingualis in a collection of permanent maxillary molarsActa Odontol Scand 2000 58(5):229-36. [Google Scholar]
[11]. Libfeld H, Rotstein I, Incidence of four-rooted maxillary second molars: Literature review and radiographic survey of 1,200 teethJ Endod 1989 15(3):129-31. [Google Scholar]
[12]. Nayak G, Aeran H, Singh I, Radix mesiolingualis and radix distolingualis: A case report of a tooth with an unusual morphologyRestor Dent Endo 2016 41(4):322-31. [Google Scholar]
[13]. Alenazy MS, Ahmad IA, Double palatal roots in maxillary second molars: A case report and literature reviewSaudi Endod J 2015 5(1):56-60. [Google Scholar]
[14]. Hoderrieth S, Gernhardt CR, Maxillary molars with morphological variations of the palatal root canals: A report of four casesJ Endod 2009 35(7):1060-65. [Google Scholar]
[15]. Shin SJ, Park JW, Lee JK, Hwang SW, Unusual root canal anatomy in maxillary second molars: Two case reportsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 104(6):e61-65. [Google Scholar]
[16]. Ghoddusi J, Mesgarani A, Gharagozloo S, Endodontic re-treatment of maxillary second molar with two separate palatal roots: A case reportIran Endod J 2008 3(3):83-85. [Google Scholar]
[17]. Yang B, Lu Q, Bai QX, Zhang Y, Liu XJ, Liu ZJ, Evaluation of the prevalence of the maxillary molars with two palatal roots by cone beam CTZhonghua Kou Qiang Yi Xue Za Zhi 2013 48(6):359-62. [Google Scholar]
[18]. Benenati FW, Maxillary second molar with two palatal canals and a palatogingival grooveJ Endod 1985 11(7):308-10. [Google Scholar]
[19]. Versiani MA, Pecora JD, de Sousa-Neto MD, Root and root canal morphology of four rooted maxillary second molars: A micro-computed tomography studyJ Endod 2012 38(7):977-82. [Google Scholar]
[20]. Rajalbandi S, Shingte SN, Sundaresh KJ, Mallikarjuna R, Aberration in the palatal root of the maxillary first molarBMJ Case Rep 2013 2013:008641 [Google Scholar]