Introduction
Over the last fifty years there has been dramatic change in the human environment, behaviours and way-of-life. These changes have resulted in escalating rates of metabolic syndrome not only in general population but also among people with mental illness. Various factors, like the lack of exercise, use of psychotropic medications and inadequate medical care leads to the increased risk of metabolic changes among people with mental illness. Hence, there is a greater need to evaluate metabolic syndrome in this population.
Aim
To find the prevalence of metabolic syndrome among psychiatric inpatients in Tertiary Care Hospital in Kashmir region of North India.
Materials and Methods
It was a cross-sectional study conducted at the Institute of Mental Health and Neurosciences, Kashmir, India. A total of 213 in-patients with a primary psychiatric diagnosis as per The International Classification of Diseases, Tenth Revision (ICD 10) Classification of Mental and Behavioural Disorders criteria were evaluated for the presence of metabolic syndrome. A modified National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criterion for the diagnosis of metabolic syndrome was used. All the intergroup comparisons for parametric data were done by Student’s t-test, whereas non-parametric data were analysed by Chi-square tests. A p-value <0.05 was considered statistically significant.
Results
The overall prevalence of metabolic syndrome was 34.74%. The prevalence was higher in females (43.3%) than males (28.5%) (p<0.05) and it increased with age, with the highest prevalence in the age group >50 years (p<0.05). Among the diagnostic subgroups, the prevalence was highest among patients with unipolar depression (45.0%), while it was lesser in patients with bipolar disorders (37.88%) and psychotic disorders (30.95%). Prevalence of metabolic syndrome was significantly higher (63.64%) among patients taking second generation antipsychotics (p<0.05).
Conclusion
Our study shows that metabolic syndrome is highly prevalent among psychiatric inpatients and needs to be addressed to prevent the risk for cardiovascular diseases.
Introduction
Metabolic syndrome refers to clustering of various cardiometabolic risk factors which includes truncal obesity, hyperglycemia, dyslipedimia and elevated blood pressure all that are likely associated to insulin resistance [1]. The syndrome has been given several names, including the ‘insulin resistance syndrome’, the ‘plurimetabolic syndrome’, and the ‘deadly quartet’ [2]. The three main aetiological factors for metabolic syndrome are: obesity and disorders of adipose tissue; insulin resistance; and a collection of independent factors like molecules of hepatic, vascular, and immunologic origin that are associated with specific components of the metabolic syndrome. Other risk factors are aging, pro inflammatory state, and hormonal changes [3].
Metabolic syndrome is highly prevalent in general population. When data from various studies across the world was analysed, which included population samples, aged 20 years and above, the prevalence rate varied from 8% (India) to 24% (United States) in men and from 7% (France) to 46% (India) in women [4]. The prevalence of metabolic syndrome is even higher in psychiatric populations. Studies across various countries with patients who have schizophrenia or schizoaffective disorder found indexes that varied between 28.4% and 62.4% [5-12]. Ample information is available which point towards the relationship between mood disorders and components of metabolic syndrome, such as obesity, hyperglycaemia, and diabetes mellitus [13].
Various factors like psychological stress, lack of exercise, poor diet, excessive smoking and inadequate medical care have been implicated in higher prevalence among psychiatric population [14]. However, the use of psychotropic medication stands out as one of the main cause for the higher prevalence of metabolic syndrome in psychiatric patients. Weight gain is a frequent side effect of many antipsychotics (like clozapine, olanzapine etc.,), mood stabilizers (valproic acid, lithium) and antidepressants (mirtazapine) [15,16]. Furthermore, many antipsychotics (like olanzapine) also have adverse effects on the glycidic and lipid metabolisms [17,18]. Hence, this study was conducted to assess the prevalence of metabolic syndrome in psychiatric inpatients, and correlate it with the psychiatric diagnoses of the patients and with the psychotropic medications used.
Materials and Methods
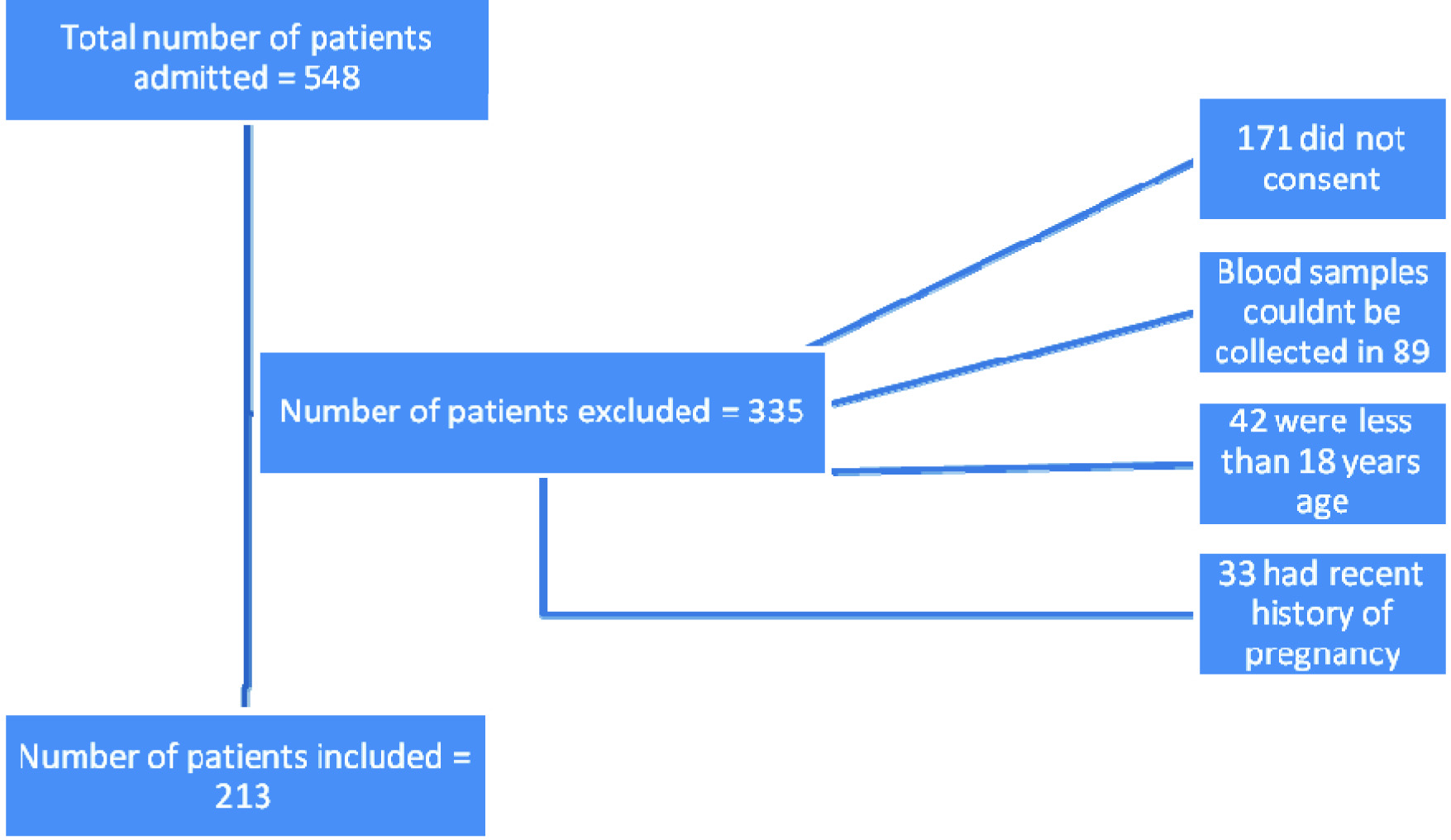
We conducted a cross-sectional study at a Tertiary Care Psychiatric Hospital. The study was approved by the Institutional Ethical Committee of the hospital. Every consecutive adult patient admitted in the Inpatient Department of the hospital during a period of one year from 1st January 2015 till 31st December 2015, was included in the study. Written informed consent was obtained from each patient; those who were incapable of consenting, the consent of their closest family member or custodian was taken. Those who did not consent or were less than 18 years of age or had a history of pregnancy in the last six months were excluded from the study. Out of the total of 548 patients admitted during the study period, 171 cases were excluded because the patients or their custodian did not give consent, 89 patients were admitted for one day only and hence their fasting blood samples could not be taken, 42 patients were less than 18 years age and 33 patients were either pregnant or had a history of pregnancy during past six months. Thus a total of 213 patients were eventually included in the study, as shown in the flowchart below [Table/Fig-1].
Flowchart depicting the number of participants included in study group.
The psychiatric diagnosis was confirmed by a consultant psychiatrist according to the ICD 10 Classification of Mental and Behavioural Disorders [19]. For the ease of analysis, the diagnoses were clubbed together in four broad groups (ICD-10 codes): psychoses (F20-F29), bipolar disorders (F30-31), unipolar depression (F32-F34), and remaining diagnostic groups (others).
The modified NCEP ATP III criterion for Asian population for Metabolic Syndrome diagnosis was used [20] according to which three or more of the following conditions were necessary for diagnosis:
Waist circumference > 90 cm for males and > 80 cm for females;
Triglycerides ≥ 150 mg/dl;
HDL levels < 40 mg/dl for males and < 50 mg/dl for females;
Blood pressure ≥ 130/ 85 mmHg;
Fasting glucose ≥ 100 mg/dl.
Waist Circumference (WC) was measured midway between the inferior border of ribs and the superior border of iliac crest, in a horizontal plane. These measurements were repeated thrice and their average was taken in all cases.
Systolic and diastolic blood pressures (SBP and DBP) were recorded twice at an interval of three minutes in the sitting position after a 15 minutes rest, and the mean was taken. For the measurement of High Density Lipoprotein (HDL), Tiglycerides (TG) and fasting plasma glucose levels, blood samples (3 ml) were drawn after 8-12 hours overnight fasting. Plasma glucose level was measured using the glucose oxidase-peroxidase enzymatic method [21] and lipid profile was measured by enzymatic assay on a Hitachi 704 system auto-analyser [22]. Out of the 213 patients, 87 were drug naïve while as 126 patients were on medication. For the ease of evaluation, medications used were clubbed together as FGA’s-First Generation Antipsychotics (includes haloperidol, trifluoperazine), SGA’s-Second Generation Antipsychotics (olanzapine, quetiapine, risperidone), antidepressants (escitalopram, fluoxetine), mood stabilizers (divalproex sodium, lithium) and multiple drugs (those on two or more drugs other than benzodiazepines).
Statistical Analysis
The results were subjected to appropriate statistical methods. Student’s t-test was used for comparison of all the inter group parametric data, while the non parametric data was analysed using the Chi-square test. A two-tailed p-value was used for calculating statistical significance. A p-value of <0.05 was taken as statistically significant.
Results
Of all the inpatients in the Psychiatric Hospital during the study period, 213 met the inclusion criteria. Of these, 42.26% were females and 57.74% were males. The mean age of the entire population was 38.26±11.4 years.
Majority (59.6%) were from rural background and from lower middle socioeconomic status (35.7%). The most commonly found diagnostic category was psychotic disorder (39.45%) followed by bipolar disorder (31%). About 41% of the study population was off psychotropic medication at the time of admission [Table/Fig-2] [23]. The prevalence of metabolic syndrome in the sample studied was 34.74% (n = 74; 95% CI: 22.7-36.9). The prevalence increased with age and it was highest in age group > 50 years. The prevalence among females was 43.3% (n = 39; 95% CI: 31.4-56.7), while the prevalence among males was 28.45% (n =35; 95% CI: 13.5-29.7); the difference between the genders was significant (p <0.05) [Table/Fig-3].
Socio demographic and clinical profile of study population [23].
| Variables | Sub Groups | Total Number (%) |
|---|
| Sex | Males | 123 (57.74) |
| Females | 90 (42.26) |
| Residence | Rural | 127 (59.62) |
| Urban | 86 (40.38) |
| Socio economic status (based on Kuppuswamy’s Socioeconomic Scale) [23] | Upper | 0 (0.00) |
| Upper middle | 48 (22.53) |
| Lower middle | 76 (35.68) |
| Upper lower | 69 (32.39) |
| Lower | 20 (9.39) |
| Diagnostic subgroups | Psychotic Disorders | 84 (39.45) |
| Bipolar Disorders | 66 (30.99) |
| Depressive Disorders | 40 (18.78) |
| Other Mental Disorders | 23 (10.80) |
| Treatment subgroups | On Treatment | 126 (59.15) |
| Off Treatment | 87 (40.85) |
Prevalence of metabolic syndrome as per gender and age group.
| Age Group (In years) | Metabolic Syndrome Prevalence in each Group | Total |
|---|
| Males | Females |
|---|
| 18-30 | 10.53% (4/38) | 17.86% (5/28) | 13.63% (9/66) |
| 31-40 | 27.27% (6/22) | 42.85% (6/14) | 33.33% (12/36) |
| 41-50 | 30.55% (11/36) | 44.44% (12/27) | 36.50% (23/63) |
| >50 | 51.85% (14/27) | 76.19% (16/21) | 62.50% (30/48) |
| Total | 28.45% (35/123) | 43.33% (39/90) | 34.74% (74/213) |
Among the diagnostic subgroups, the prevalence of MS was highest (45%) among those with depressive disorders [Table/Fig-4]. Among the treatment subgroups, the prevalence was highest among those taking SGA’s (63.64%) [Table/Fig-5].
Prevalence of metabolic syndrome as per diagnostic groups.
| Diagnostic Groups | Metabolic Syndrome | Total | p-value |
|---|
| Absent | Present |
|---|
| Psychotic Disorders | 58(69.05%) | 26 (30.95%) | 84(100.0%) | p = 0.4134* |
| Bipolar Disorders | 41(62.12%) | 25 (37.88%) | 66(100.0%) |
| Depressive Disorders | 22 (55.0%) | 18 (45.0%) | 40 (100.0%) |
| Other Mental Disorders | 18 (78.26%) | 5 (21.74) | 23(100.0%) |
Chi-square test is used.
Prevalence of metabolic syndrome as per psychotropic drugs received.
| Treatment received | Total No. of Patients | Metabolic Syndrome | p-value |
|---|
| Absent | Present |
|---|
| FGA’s | 12 | 9 (75%) | 3 (25%) | p<0.05* |
| SGA’s | 22 | 8 (36.36%) | 14 (63.64%) |
| Mood Stabilizers | 21 | 16 (76.19%) | 5 (23.81%) |
| Antidepressants | 17 | 15 (88.24%) | 2 (11.76%) |
| Multiple drugs | 54 | 27 (50%) | 27 (50%) |
FGA’s = First Generation Antipsychotics SGA’s = Second Generation Antipsychotics
Chi-square test showing difference among groups.
Among the individual metabolic abnormalities, low HDL levels (males<40 mg/dl, females<50 mg/dl) was the most common abnormality among all patients (52.11%) while as high diastolic blood pressure (≥85 mmHg) was least common abnormality (17.84%). Metabolic syndrome was most commonly associated with elevated waist circumference (88.89%) and least associated with high (≥85 mmHg) diastolic pressure (34.21%). Metabolic syndrome and its relationship with clinical variables are shown in [Table/Fig-6].
Prevalence of metabolic syndrome as per individual metabolic abnormalities.
| Individual Metabolic Abnormalities | Number of Patients (% of Total) | Metabolic Syndrome | p-value* |
|---|
| Absent | Present |
|---|
| Increased Waist Circumference (males>90 cm, females>80 cm) | 54 (25.35%) | 6 (11.11%) | 48 (88.89%) | <0.05 |
| Low HDL levels (males<40 mg/dl, females<50 mg/dl) | 111 (52.11%) | 55 (49.55%) | 56 (50.45%) | 0.9244 |
| High Triglycerides (>150 mg/dl) | 90 (42.25%) | 34 (37.78%) | 56 (62.22%) | <0.05 |
| High Systolic Blood pressure (≥130 mm Hg) | 68 (31.92%) | 40 (58.82%) | 28 (41.18%) | 0.1773 |
| High Diastolic Blood pressure (≥85 mmHg) | 38 (17.84%) | 25 (65.79%) | 13 (34.21%) | 0.9203 |
| High Fasting plasma glucose (≥100 mg/dl) | 69 (32.39%) | 36 (52.17%) | 33 (47.83%) | <0.05 |
| Increased BMI (≥25) | 69 (32.39%) | 44 (63.77%) | 25 (36.23%) | 0.761 |
HDL = High Density Lipoprotein BMI= Body Mass Index
Using chi-square test
Discussion
The overall prevalence of metabolic syndrome in our study was 34.74%. Our results are comparable to the other studies which had similar study design as ours. In a North Indian study by Mattoo SK and Mohan Singh S, among the 90 patients included in the study, the prevalence of MS was 37.8% [24]. In a recent study in Hong Kong by Bressington DT et al., the overall prevalence of MS found was 35% [25].
Among the diagnostic subgroups, the prevalence of metabolic syndrome was highest among those with depressive disorders (45%) followed by those with bipolar disorders (37.8%). These results are comparable to numerous studies done across the world as shown in [Table/Fig-6]. Similarly, the prevalence of metabolic syndrome among patients with psychotic disorders was 30.95%. Prevalence rates of metabolic syndrome have varied from 26% to 52.2% in various cross-sectional studies [Table/Fig-7] [24-32].
Summary of various studies on prevalence of MS in patients with psychiatric disorders [24-32].
| Study | Prevalence of Ms |
|---|
| Depressive Disorders |
| Mattoo SK and Mohan Singh S [24] | 52.2% |
| Teixeira PJR and Rocha FL [26] | 48.1% |
| Kinder LS et al., [27] | 50% |
| Bipolar Disorders |
| Teixeira PJR and Rocha FL [26] | 38.3% |
| Chang HH et al., [28] | 33.9% |
| Psychotic Disorders |
| Malhotra N et al., [29] | 26% |
| Pallava A et al., [30] | 27.5% |
| Sugawara N et al., [31] | 36% |
| Medeiros-Ferreira L et al., [32] | 36.8% |
MS= metabolic syndrome
In our study, the prevalence of metabolic syndrome was highest (63.64%) in patients on SGA’s, followed by those on multiple (≥2) drugs (50%). The prevalence was lesser in patients on mood stabilizers, first generation antipsychotics and antidepressants. These findings are in accordance with numerous studies in literature. Yumru M et al., studied the atypical antipsychotics (also called second generation antipsychotics SGA’s) related metabolic syndrome in bipolar patients. Atypical Antipsychotic taking patients had significantly higher MS rates than the others (χ2=10.47 df=2 p= 0.005). Also, atypical antipsychotic taking patients had significantly higher metabolic syndrome rates than mood stabilizers taking patients (χ2=8.86 df=1 p=0.003) [33]. In a recent study on 210 patients with schizophrenia, Gupta A et al., found that olanzapine was the most potent antipsychotic to induce metabolic syndrome followed by clozapine [34]. Corell CU et al., in his study evaluated the risk of metabolic syndrome in patients on antipsychotic polypharmacy. He concluded that compared with antipsychotic monotherapy, polytherapy was associated with elevated rates of metabolic syndrome (50.0% vs. 34.3%, p=0.015) [35]. In another study by Misawa E et al., results suggested that antipsychotic polypharmacy may be independently associated with an increased risk of having pre-metabolic syndrome, even after adjusting for patients’ lifestyle characteristics as compared with monotherapy [36]. In our study, the prevalence of metabolic syndrome was highest (88.89%) in patients with waist circumference above cut off levels followed by those with elevated triglyceride levels (62.22%). Thus, waist circumference emerged as the best predictor of metabolic syndrome among various metabolic parameters. Our results are in accordance with numerous studies which have shown similar results. In the study by Mattoo SK and Mohan Singh S, about 70% of the patients with waist circumference above cut off level as per IDF criteria had metabolic syndrome [24]. In our study, the mean value of each metabolic parameter like waist circumference, triglycerides and fasting blood sugar was significantly higher in patients with metabolic syndrome than those without metabolic syndrome. While as serum HDL levels, blood pressure and BMI were significantly lower in patients with metabolic syndrome as compared to patients without metabolic syndrome. Similar results have been obtained in various studies comparing individual metabolic parameters in those with and without mental illness [37-40].
Limitation
It was a hospital based study which may not be representative of other individuals with less complex illness presentations in the community. We could not compare our results with age and sex matched healthy controls.
Conclusion
Our study showed that the prevalence of metabolic syndrome among psychiatric inpatients in Kashmir was significantly high. Patients with unipolar depression or those on second generation antipsychotics had higher prevalence. Female gender and increasing age were associated with greater risk. Thus, we conclude that the people with major mental disorders are at greater risk of metabolic syndrome that impacts their morbidity and mortality. Hence, these patients should be routinely monitored for cardiometabolic risk factors during their treatment.
*Chi-square test is used.
FGA’s = First Generation Antipsychotics SGA’s = Second Generation Antipsychotics
*Chi-square test showing difference among groups.
HDL = High Density Lipoprotein BMI= Body Mass Index
*Using chi-square test
MS= metabolic syndrome
[1]. Eckel RH, Grundy SM, Zimmet PZ, The metabolic syndromeLancet 2005 365:1415-28. [Google Scholar]
[2]. Isomaa BO, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Cardiovascular morbidity and mortality associated with the metabolic syndromeDiabetes care 2001 24(4):683-89. [Google Scholar]
[3]. Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant C, Definition of metabolic syndrome: Report of the national heart, lung, and blood institute/American heart association conference on scientific issuesCirculation 2004 109:433-38. [Google Scholar]
[4]. Cameron AJ, Shaw JE, Zimmet PZ, The metabolic syndrome: Prevalence in worldwide populationsEndocrinol Metab Clin N Am 2004 33:351-35. [Google Scholar]
[5]. Heiskanen T, Niskanen L, Lyytikäinen R, Metabolic syndrome in patients with schizophreniaJ Clin Psychiatry 2003 64(5):575-79. [Google Scholar]
[6]. Basu R, Brar JS, Roy Chengappa KN, John V, Parepally H, Gershon S, The prevalence of the metabolic syndrome in patients with schizoaffective disorder–bipolar subtypeBipolar Disorders 2004 6(4):314-18. [Google Scholar]
[7]. Cohn T, Prud’homme D, Streiner D, Characterizing coronary heart disease risk in chronic schizophrenia: High prevalence of metabolic syndromeCan J Psychiatry 2004 49(11):753-60. [Google Scholar]
[8]. Kato MM, Currier MB, Gomez CM, Prevalence of metabolic syndrome in Hispanic and non-Hispanic patients with schizophreniaPrim Care Companion J Clin Psychiatry 2004 6(2):74-77. [Google Scholar]
[9]. McEvoy JP, Meyer JM, Goff DC, Nasrallah HA, Davis SM, Sullivan L, Prevalence of the metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES IIISchizophrenia research 2005 80(1):19-32. [Google Scholar]
[10]. Meyer J, Loh C, Leckband SG, Boyd JA, Wirshing WC, Pierre JM, Prevalence of the metabolic syndrome in veterans with schizophreniaJournal of Psychiatric Practice® 2006 12(1):5-10. [Google Scholar]
[11]. Hagg S, Lindblom Y, Mjorndal T, High prevalence of the metabolic syndrome among a Swedish cohort of patients with schizophreniaInt Clin Psychopharmacol 2006 21(2):93-98. [Google Scholar]
[12]. De Hert MA, van Winkel R, Van Eyck D, Hanssens L, Wampers M, Scheen A, Prevalence of the metabolic syndrome in patients with schizophrenia treated with antipsychotic medicationSchizophrenia research 2006 83(1):87-93. [Google Scholar]
[13]. Fredric C, Eilen AH, Elevated frequency of diabetes mellitus in hospitalized Manic-Depressive patientsAm J psychiatry 1999 159(9):1417-20. [Google Scholar]
[14]. Kumar CTS, Physical illness and schizophreniaBritish Journal of Psychiatry 2004 184:541 [Google Scholar]
[15]. Ferrannini E, Haffner SM, Mitchell BD, Hyperinsulinaemia: The key feature of a cardiovascular and metabolic syndromeDiabetologia 1991 34:416-22. [Google Scholar]
[16]. Abbasi F, Brown BW, Lamendola C, Relationship between obesity, insulin resistance, and coronary heart disease riskJ Am Coll Cardiol 2002 40:937-43. [Google Scholar]
[17]. Kahn BB, Flier JS, Obesity and insulin resistanceJ Clin Invest 2000 106:473-81. [Google Scholar]
[18]. Montague C, O’Rahilly S, The perils of portliness: Causes and consequences of visceral adiposityDiabetes 2000 49:883-88. [Google Scholar]
[19]. World Health OrganizationInternational statistical classification of diseases and health related problems, (The) ICD-10 2004 2nd EdGeneva, Switzerland [Google Scholar]
[20]. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Diagnosis and management of the metabolic syndrome an American Heart Association/National Heart, Lung, and Blood Institute scientific statementCirculation 2005 112(17):2735-52. [Google Scholar]
[21]. Bergmeyer HU, Bernt E, Bergmeyer HU, Determination of D-glucose with glucose oxidase and peroxidaseMethods of Enzymatic Analysis 1974 2nd editionNew YorkAcademic Press:1205-12. [Google Scholar]
[22]. Lentjes EG, Harff GA, Backer ET, Evaluation of the Hitachi 704 automatic analyserClin Chem 1987 33:2089-92. [Google Scholar]
[23]. Oberoi S, Updating income ranges for Kuppuswamy’s socio-economic status scale for the year 2014Indian Journal of Public Health 2015 59(2):156-56. [Google Scholar]
[24]. Mattoo SK, Mohan Singh S, Prevalence of metabolic syndrome in psychiatric inpatients in a tertiary care centre in north IndiaIndian Journal of Medical Research 2010 131(1):46-52. [Google Scholar]
[25]. Bressington DT, Mui J, Cheung EFC, Petch J, Clark AB, Gray R, The prevalence of metabolic syndrome amongst patients with severe mental illness in the community in Hong Kong –a cross sectional studyBMC Psychiatry 2013 13(1):87 [Google Scholar]
[26]. Teixeira PJR, Rocha FL, The prevalence of metabolic syndrome among psychiatric inpatients in BrazilRevista Brasileira de Psiquiatria 2007 29(4):330-36. [Google Scholar]
[27]. Kinder LS, Carnethon MR, Palaniappan LP, King AC, Fortmann SP, Depression and the metabolic syndrome in young adults: Findings from the national health and nutrition examination surveyPsychosom Med 2004 66:316-22. [Google Scholar]
[28]. Chang HH, Chou CH, Chen PS, Gean PW, Huang HC, Lin CY, High prevalence of metabolic disturbances in patients with bipolar disorder in TaiwanJournal of affective disorders 2009 117(1):124-29. [Google Scholar]
[29]. Malhotra N, Grover S, Chakrabarti S, Kulhara P, Metabolic syndrome in schizophreniaIndian Journal of Psychological Medicine 2013 35(3):227-40. [Google Scholar]
[30]. Pallava A, Chadda RK, Sood M, Lakshmy R, Metabolic syndrome in schizophrenia: A comparative study of antipsychotic-free/naïve and antipsychotic-treated patients from IndiaNord J Psychiatry 2012 66:215-21. [Google Scholar]
[31]. Sugawara N, Yasui-Furukori N, Sato Y, Umeda T, Kishida I, Yamashita H, Prevalence of metabolic syndrome among patients with schizophrenia in JapanSchizophr Res 2010 123:244-50. [Google Scholar]
[32]. Medeiros-Ferreira L, Obiols JE, Navarro-Pastor JB, Zúñiga-Lagares A, Metabolic syndrome and health-related quality of life in patients with schizophreniaActas Esp Psiquiatr 2013 41(1):17-26. [Google Scholar]
[33]. Yumru M, Savas HA, Kurt E, Kaya MC, Selek S, Savas E, Atypical antipsychotics related metabolic syndrome in bipolar patientsJournal of Affective Disorders 2007 98(3):247-52. [Google Scholar]
[34]. Gupta A, Dadheech G, Yadav D, Sharma P, Gautam S, Metabolic issues in schizophrenic patients receiving antipsychotic treatmentIndian Journal of Clinical Biochemistry 2014 29(2):196-201. [Google Scholar]
[35]. Correll CU, Frederickson AM, Kane JM, Manu P, Does antipsychotic polypharmacy increase the risk for metabolic syndrome?Schizophr Res 2007 89(1):91-100. [Google Scholar]
[36]. Misawa F, Shimizu K, Fujii Y, Miyata R, Koshiishi F, Kobayashi M, Is antipsychotic polypharmacy associated with metabolic syndrome even after adjustment for lifestyle effects?: A cross-sectional studyBMC Psychiatry 2011 11(1):118 [Google Scholar]
[37]. Heiskanen T, Niskanen L, Lyytikäinen R, Metabolic syndrome in patients with schizophreniaJ Clin Psychiatry 2003 64(5):575-79. [Google Scholar]
[38]. Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: A systematic review and meta-analysisWorld Psychiatry 2015 14(3):339-47. [Google Scholar]
[39]. Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M, Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders—a systematic review and meta-analysisSchizophrenia bulletin 2013 39(2):306-18. [Google Scholar]
[40]. Saenz BM, Guillena SR, de Diego BP, Comparison of metabolic syndrome between patients with severe mental disordersEuropean Psychiatry 2016 33:S283-84. [Google Scholar]