An Unusual Cause of Organizing Pneumonia: Hydrocarbon Pneumonitis
Kuruswamy Thurai Prasad1, Sahajal Dhooria2, Amanjit Bal3, Ritesh Agarwal4, Inderpaul Singh Sehgal5
1 Assitant Professor, Department of Pulmonary Medicine, PGIMER, Chandigarh, India.
2 Assitant Professor, Department of Pulmonary Medicine, PGIMER, Chandigarh, India.
3 Professor, Department of Histology, PGIMER, Chandigarh, India.
4 Professor, Department of Pulmonary Medicine, PGIMER, Chandigarh, India.
5 Assitant Professor, Department of Pulmonary Medicine, PGIMER, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Inderpaul Singh Sehgal, Department of Pulmonary Medicine, PGIMER, Chandigarh-160012, India.
E-mail: inderpgi@outlook.com
Hydrocarbon pneumonitis is a type of acute exogenous lipoid pneumonia due to the aspiration of petroleum products. The clinical and radiological features of this condition are non-specific and the diagnosis is usually missed if a careful history is not taken. Herein, we describe a 24-year-old male who was referred to us with a diagnosis of Interstitial Lung Disease (ILD) and was later found to have hydrocarbon pneumonitis.
Acute interstitial pneumonia, Aspiration pneumonia, Lipoid pneumonia
Case Report
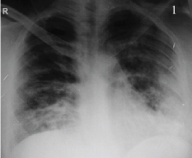
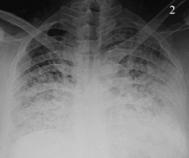
A 24-year old male, previously a healthy individual, was referred to us with dry cough and dyspnoea. One month back, the patient presented at another hospital with acute onset dyspnoea. There was no history of wheezing, cough, hemoptysis, chest pain or fever. He was normotensive (mean arterial blood pressure of 88 mmHg) and oxygen saturation by pulse oximetry (SpO2) was 84% while breathing ambient air. Chest radiograph revealed ill-defined alveolar and reticular opacities in the bilateral mid and lower zones [Table/Fig-1]. His echocardiogram did not reveal any underlying cardiac abnormality and his renal function tests were normal. One day after hospitalization, his breathlessness worsened and a repeat chest radiograph on day six showed an increase in the opacities, suggestive of Acute Respiratory Distress Syndrome (ARDS) [Table/Fig-2]. He was treated empirically as a case of Community Acquired Pneumonia (CAP), with broad spectrum intravenous antibiotics (ceftriaxone, 2 grams twice daily and azithromycin, 500 mg once daily) and supplemental oxygen therapy. With treatment, his respiratory failure improved, but he continued to have dry cough and dyspnoea. He was referred to our center with a provisional diagnosis of ILD due to persistence of reticulonodular opacities [Table/Fig-3].
Chest radiograph on day one showing ill-defined alveolar and reticular opacities in bilateral lower zones;
Chest radiograph on day six showing extensive bilateral alveolar and reticulonodular opacities;
Chest radiograph at three weeks showing reticular opacities in bilateral mid and lower zones.

On presentation to our center, the patient was comfortable, with a pulse rate of 82 beats per minute and a respiratory rate of 22 breaths per minute. Oxygen saturation by pulse oximetry was 93% while breathing room air. Rest of the systemic examination was normal.
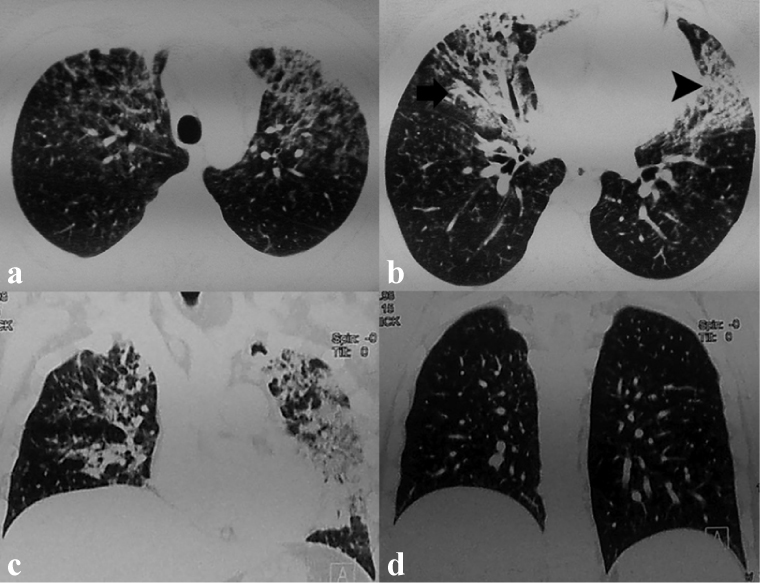
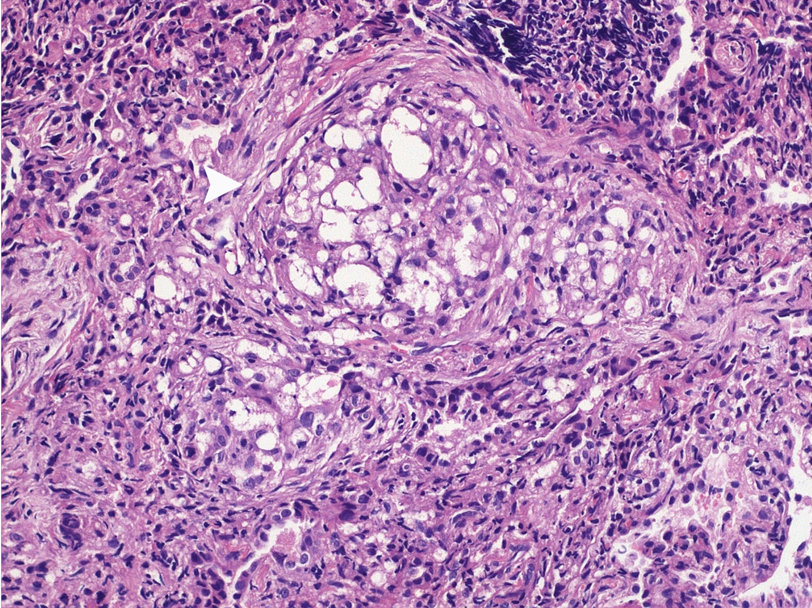
Blood investigations including complete haemogram and routine biochemistry were unremarkable [Table/Fig-4]. Antinuclear Antibody (ANA) and Antineutrophil Cytoplasmic Antibody (ANCA) were negative. High Resolution Computed Tomography (HRCT) of the thorax revealed bilateral patchy consolidation and ground glass opacities with septal thickening in the bilateral upper lobes, right middle lobe and left lingula [Table/Fig-5]. Pulmonary function testing showed mild restriction. During six-minute walk test, he could walk up to 350 meters and SpO2 decreased to 86%. Flexible bronchoscopy was done to perform Broncho-Alveolar Lavage (BAL) and Trans-Bronchial Lung Biopsy (TBLB). BAL showed predominance of macrophages with few neutrophils and lymphocytes. TBLB depicted lipid laden macrophages within the alveoli and the interstitium causing interstitial widening and fibrosis, a feature consistent with lipoid pneumonia [Table/Fig-6]. On further probing, patient gave history of frequent siphoning of diesel from automobiles at his place of employment, but denied any episode of accidental aspiration.
| Parameter | Patient Value | Reference Range |
|---|
| Hemoglobin (12-18 g/L) | 11.8g/L | 12-18g/L |
| Total leukocyte count | 12 x 109/L | 4-11 X 109/L |
| Platelet count | 151 x 109/L | 150-400 X 109/L |
| Blood urea nitrogen | 2.02 mmol/L | 2.5-7.1 mmol/L |
| Serum creatinine | 53.05 pmol/L | 50-120 Mmol/L |
| Serum albumin | 34 g/L | 34-48 g/L |
| Serum bilirubin | 10.26 pmol/L | 5.1-22 Mmol/L |
| Aspartate transaminase | 38U/L | 2-40U/L |
| Alanine transaminase | 32U/L | 2-41U/L |
| Alkaline phosphatase | 38U/L | 42-128U/L |
| Serum calcium | 2.15mmol/L | 2.2-2.6 mmol/L |
| Serum phosphorus | 0.87 mmol/L | 0.81-1.4 mmol/L |
| Serum sodium | 138 mmol/L | 135-145 mmol/L |
| Serum potassium | 3.6 mmol/L | 3.5-5 mmol/L |
| FVC | 3.12 L (68% of predicted value) | 4.62 L* |
| FEV1 | 2.72 L (71% of predicted value) | 3.83 L* |
| FEV1/FVC | 87.2 % | 83.5 %* |
FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; FEV1/FVC: ratio of forced expiration volume in 1 second and forced vital capacity
Predicted value for an individual of same ethnicity, age, sex, height
HRCT at three weeks showing consolidation, ground glass opacities, septal thickening and ill-defined nodules in bilateral upper lobes, right middle lobe and left lingula. Coronal lung sections showing involvement of the anterior lung fields and sparing of the posterior lung fields (a,b). Few centrilobular nodules with tree in bud appearance could be seen in the lower lobes (c,d).
Photomicrograph of transbronchial lung biopsy showing large fat spaces within alveoli surrounded by histiocytic reaction and fibroblastic proliferation. Surrounding lung parenchyma shows prominence of type 2 pneumocytes and collections of macrophages (Haematoxylin and Eosin, x200).
A final diagnosis of organizing pneumonia due to diesel aspiration was made. The patient was advised to refrain from the practice of siphoning petroleum products in the future. At follow up, eight weeks after symptom onset, there was complete spontaneous resolution of his symptoms.
Discussion
The index case highlights the importance of thorough history taking and tissue sampling in the diagnosis of hydrocarbon pneumonitis which is an important occupational hazard. Our patient was referred as a case of ILD, in whom organizing pneumonia and resolving phase of Acute Interstitial Pneumonia (AIP) were the initial diagnoses. The diagnosis of lipoid pneumonia could only be made after the histological demonstration of lipid laden macrophages and was corroborated later by a history of diesel siphoning. Although our patient could not recollect any episodes of aspiration, the acute onset of symptoms, the characteristic gravity-dependent distribution of radiological abnormalities, and the presence of numerous lipid laded macrophages in the lung biopsy support the diagnosis of hydrocarbon pneumonitis.
Lipoid pneumonia is a condition which is caused by accumulation of either exogenous or endogenous lipids in the lung parenchyma [1]. Hydrocarbon pneumonitis is an acute form of exogenous lipoid pneumonia caused by aspiration of mineral oils. The symptoms of hydrocarbon pneumonitis are non specific and include cough, dyspnoea, chest pain, fever, and rarely hemoptysis [1,2]. Some patients develop hypoxemia which may progress to ARDS, as in the index case during initial presentation [1,3]. However, patients who continue to siphon petroleum products may present with chronic symptoms [4,5]. This is because, mineral oils, being bland and non irritating in nature, gain entry into lungs without eliciting cough [6]. This fact is highlighted by the index case who could not recall any episode of aspiration and continued with diesel siphoning after recovery from acute illness.
The common radiological abnormalities include consolidation, ground glass opacities and centrilobular nodules [7]. Less frequently, pneumatoceles, large nodules, cavitating nodules, pleural effusion and spontaneous pneumothorax have also been described [7]. The finding of areas of fat attenuation within consolidation is considered to be a characteristic feature; however, it is non-specific, and may not be present in all cases [1,7,8]. The distribution of radiological abnormalities is related to the subject’s position at the time of aspiration [6]. Fuel siphoning is usually done in a leaning forward position and commonly involves the right middle lobe (as noted in the index case) [7].
The treatment of hydrocarbon pneumonitis is mainly supportive. Apart from anecdotal reports, there is no clear evidence of the benefits of corticosteroids and antibiotics in this condition [1]. Whole lung lavage has been reported to be beneficial in some cases [9]. The most important aspect is to recognize the cause of lipoid pneumonia (diesel siphoning in the index case) and institute corrective measures to prevent continuous damage. This usually results in complete radiological and functional recovery occurs regardless of the therapeutic strategy in 3-6 months [1,2]. The index case had spontaneous resolution of symptoms at follow up.
Conclusion
In conclusion, hydrocarbon pneumonitis is an important occupational hazard and can mimic other lung diseases including ILD leading to mismanagement. A high index of clinical suspicion and a detailed history enables diagnosis and prevent permanent damage.
FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; FEV1/FVC: ratio of forced expiration volume in 1 second and forced vital capacity
*Predicted value for an individual of same ethnicity, age, sex, height
[1]. Franzen D, Kohler M, Degrandi C, Kullak-Ublick GA, Ceschi A, Fire eater’s lung:Retrospective analysis of 123 cases reported to a National Poison CenterRespiration 2014 87:98-104. [Google Scholar]
[2]. Gentina T, Tillie-Leblond I, Birolleau S, Saidi F, Saelens T, Boudoux L, Fire-eater’s lung:Seventeen cases and a review of the literatureMedicine (Baltimore) 2001 80:291-97. [Google Scholar]
[3]. Shrivastava MS, Palkar AV, Karnik ND, Hydrocarbon pneumonitis masquerading as acute lung injuryBMJ Case Rep 2011 2011:pii:bcr0320114017 [Google Scholar]
[4]. Venkatnarayan K, Madan K, Walia R, Kumar J, Jain D, Guleria R, Diesel siphoner’s lung:Exogenous lipoid pneumonia following hydrocarbon aspirationLung India 2014 31:63-66. [Google Scholar]
[5]. Yampara Guarachi GI, Barbosa Moreira V, Santos Ferreira A, Sias SM, Rodrigues CC, Teixeira GH, Lipoid pneumonia in a gas station attendantCase Rep Pulmonol 2014 2014:358761 [Google Scholar]
[6]. Freiman DG, Engelberg H, Merrit WH, Oil aspiration (lipoid) pneumonia in adults:A clinicopathologic study of forty-seven casesArch Intern Med 1940 66:11-38. [Google Scholar]
[7]. Yi MS, Kim KI, Jeong YJ, Park HK, Lee MK, CT findings in hydrocarbon pneumonitis after diesel fuel siphonageAJR Am J Roentgenol 2009 193:1118-21. [Google Scholar]
[8]. Agarwal R, Low-attenuation consolidation - the most characteristic finding in lipoid pneumoniaEur J Intern Med 2006 17:307 [Google Scholar]
[9]. Russo R, Chiumello D, Cassani G, Maiocchi G, Gattinoni L, Case of exogenous lipoid pneumonia:Steroid therapy and lung lavage with an emulsifierAnesthesiology 2006 104:197-98. [Google Scholar]