Granular Cell Tumour of the Tongue: Report of a Case
Swati Goel1, Manish Goel2
1 Reader and Head, Department of Oral Medicine and Radiology, Eklavya Dental College and Hospital, Kotputli, Jaipur, Rajasthan, India.
2 Research Officer, Department of Pulmonary Medicine, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swati Goel, Pocket C-60A, Gangotri Enclave, Alaknanda, New Delhi-110019, India.
E-mail: Swatigarg610@gmail.com
Dorsal surface, Epithelial hyperplasia, Growth
A 60-year-old female patient presented with a complaint of growth on the dorsal surface of tongue since one year. Growth was initially small but gradually increased to the present size within six months. Since six months there was no increase in the size of the growth. The patient gave no history of trauma, pain, bleeding, ulceration or pus discharge. Past dental history, medical history, family history and drug history was non contributory. Intraoral examination revealed a well circumscribed soft tissue sessile growth with a smooth surface, oval shape and measured 0.8 x 0.5 cm approximately on the dorsal surface of tongue in the midline. The growth was pinkish pale in colour. Characteristic loss of gustatory papillae of the overlying mucosa was seen. There was no bleeding or pus discharge associated with growth. On palpation, growth was firm in consistency with no regional lymphadenopathy. The borders were clearly palpable. There was no tenderness on palpation [Table/Fig-1]. A provisional diagnosis of fibroma was given.
Intraoral photograph shows single sessile growth on the dorsal surface of tongue in the midline.

H and E section at 10X showed stratified squamous epithelium with subjacent fibrovascular connective tissue showing aggregates of cells with granular cytoplasm.
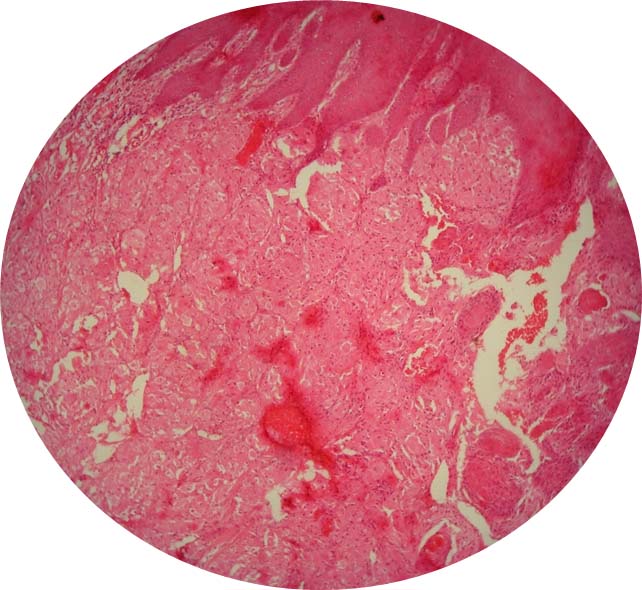
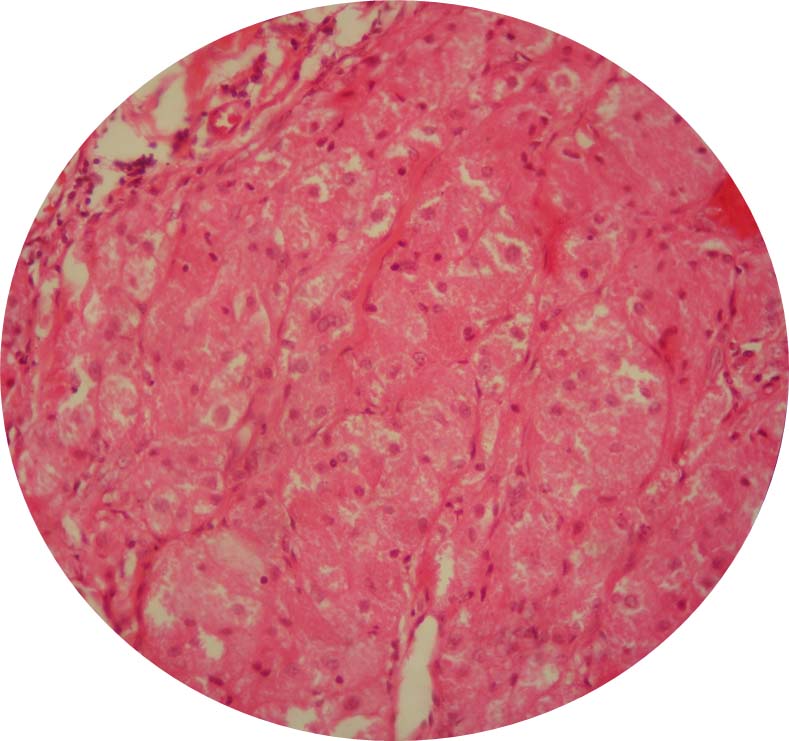
Patient was advised haematological tests and the results were within the normal limits. Excisional biopsy was performed under local anaesthesia which was subjected to histopathological examination. The haematoxylin-eosin stained sections showed stratified squamous keratinising epithelium, fibrovascular connective tissue and striated muscle. The connective tissue showed aggregates of large round cells with eosinophilic granular cytoplasm extending between muscle bundles. Based on histopathological findings, the final diagnosis of Granular Cell Tumour was made [Table/Fig-2,3]. Patient was recalled after one week and satisfactory healing was seen [Table/Fig-4].
H and E section at 40X showed aggregates of large round cells with vesicular nuclei and eosinophilic granular cytoplasm infiltrating striated muscle fibre.
Postoperative intraoral photograph shows complete excision of growth with satisfactory healing.

Discussion
Abrikossoff tumour is also known as Granular Cell Tumour (GCT) and is usually discovered accidentally [1]. In the past, GCT has been referred to as granular cell myoblastoma, granular cell neurofibroma or granular cell schwannoma because of the uncertainty surrounding its aetiology. The origin of this tumour has been associated with striated muscle, histiocytes, fibroblasts, myoepithelium and nerve cell connective tissue [2]. GCT occurs most frequently in the fourth to sixth decade of life [3]. Women are more affected than men, with a female: male ratio of 2:1 [4]. Most GCTs are found on the head and neck region with tongue as most common site for occurrence but tumours of buccal mucosa, hard palate, lip, gingiva, uvula and parotid gland have also been reported. They are also seen in skin, gastrointestinal tract, respiratory tract, nervous system, male and female reproductive tract and bronchus [3]. Clinically, GCT of the oral cavity appears as a single, sessile, smooth nodular mass with less than 2 cm in diameter. The surface appears pink in colour. The nodular mass is firm to hard in consistency covered by intact overlying mucosa [5]. Benign connective and neural tumours such as fibromas, lipomas, neuromas, neurofibromas, pleomorphic adenoma of the minor salivary glands of the tongue should be included in the differential diagnosis of GCT [2].
Diagnosis of GCT is clinically difficult because of the similarity in shape and colour with other epithelial lesions; therefore the histological examination will help in establishing the definitive diagnosis. Histologically, GCT is poorly circumscribed and is composed of numerous strands and sheets of large polyhedral cells. These cells have abundant pale cytoplasm filled with numerous eosinophilic coarse granules and small round or oval nuclei as reported in our case.
Treatment of choice for GCT consists of surgical excision regardless of the lesion being solitary or multifocal with safety margins [5]. Due to incomplete removal of the lesion, local recurrence is possible in about 15% of cases [4]. Because of the resistance of the tumour and potential carcinogenic effect of such treatment, radiation and chemotherapy are not recommended for the benign lesions but are recommended for treatment of malignant forms of the lesion [1]. Patients are advised follow up at periodic intervals due to possibility of recurrences and malignant transformation [4].
[1]. Gopinath D, Beena VT, Padmakumar SK, Sugirtharaj G, Granular cell tumour of tongue: Report of two casesIndian J Oral Sci 2016 7:47-50. [Google Scholar]
[2]. Daniels JSM, Granular cell tumour of tongue: A case report The Saudi Dental Journal 2009 21:75-78. [Google Scholar]
[3]. Nagaraj PB, Ongole R, Bhujanga-Rao BR, Granular cell tumour of the tongue in a 6-year-old girl-a case reportMed Oral Patol Oral Cir Bucal 2006 11:E162-64. [Google Scholar]
[4]. Sousa FB, Osterne RLV, Matos Brito RG, Alves APNN, Soares ECS, Costa FWG, Oral granular cell tumour: A study of twelve cases in a Brazilian populationJ Clin Exp Dent 2010 2(4):e178-82. [Google Scholar]
[5]. Prieto-Oliveira P, Vitorino Cardoso S, Zumbaio Mistro F, Kignel S, de Sousa SCOM, Brazão-Silva MT, Typical Aspects of the Granular Cell Tumour of the Oral CavityInternational Journal of Otolaryngology and Head & Neck Surgery 2014 3:318-22. [Google Scholar]