Case Report
A 44-year-old male patient, a tailor by profession reported to the Department of Oral medicine and Radiology, Sri Ramachandra University, Chennai, Tamil Nadu, India, in April 2014 with a chief complaint of an ulcer on the surface of the tongue for past five years. History of present illness revealed that the patient was apparently well five years back when he noticed an ulcer on the dorsal surface of the tongue in the year 2008, which was small initially, subsided on its own in a few days, associated with pain and burning sensation and persisted for about a month and healed on its own. It was recurrent in nature and when it appeared subsequently it gradually increased in size and he underwent biopsy in 2008 whose reports were unavailable with the patient. He was prescribed a topical application of 0.1% triamcinolone acetonide for a period of 15 days after which he was symptom free for about three years. Patient gave a history of recurrence of the ulcer from about one year and an increase in size to attain the present size. The patient underwent a biopsy in December 2013, which was reported as “inflammatory non-malignant granulomatous ulcer of the oral mucosa. The presence of plasma cells argues to exclude the possibility of associated systemic Crohn’s disease.” He was then prescribed dexamethasone rinses and prednisolone 5 mg three times a day for 15 days but had no relief. He complained of inability to eat properly due to the presence of burning sensation along with the pain which appeared in the past two months.
Patient had no relevant medical history, no known drug allergy and not under any prolonged medication. No history of previous hospitalization was present. He did not give any history of gastrointestinal disturbances, distress, cramps or loss of hair. He had no history of smoking, alcohol or any form of deleterious habits. On general clinical examination, patient had no signs of anaemia, cyanosis, clubbing, jaundice and pedal oedema. His vital signs were in normal range and on clinical examination of systems, no abnormal findings were observed.
On temporomandibular joint examination, no abnormal findings were observed. No facial asymmetry was noted. On regional lymph node examination, a single submandibular lymph node was palpable on both sides.
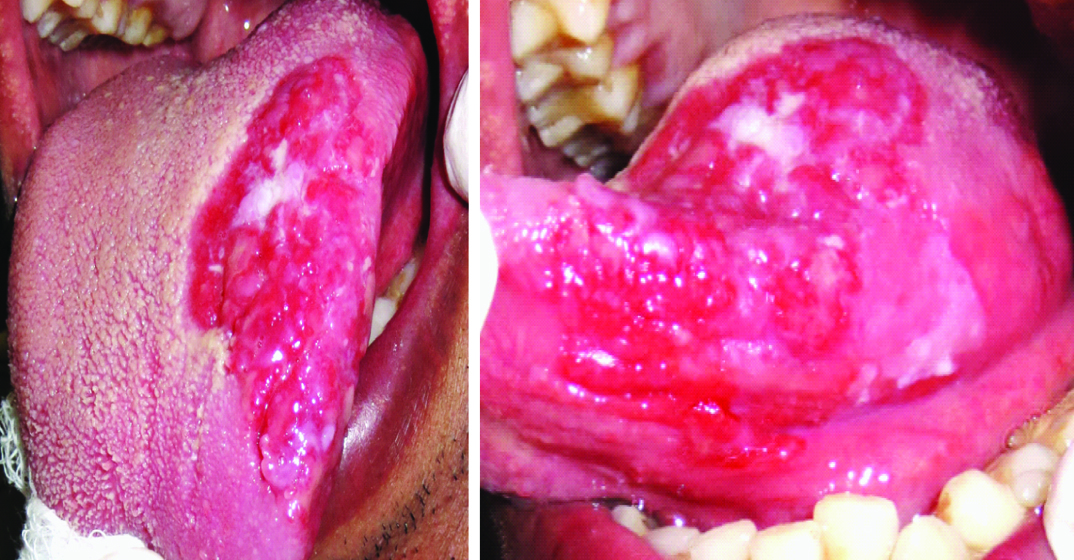
On intraoral inspection of the lesion, a single, well defined bright red erythematous plaque like area was evident in the left dorsal surface of the tongue, approximately measuring about 4 cm x 4 cm in dimension, extending from the midline to the left lateroventral surface of the tongue and 1 cm behind the tip of the tongue to approximately 2 cm in front of the base of the tongue. Surface appeared erythematous and mildly wrinkled with grayish white hyperkeratotic areas intermingled with the presence of irregularities on the anterior margin. Surrounding area was mildly erythematous. Lateral and ventral surfaces over the lesion had three erosions which were about 1 cm x 1 cm in size each. On palpation, all the inspectory findings of size, shape, site, margins and extent was confirmed. It was tender, firm in consistency with no induration and bleeding on palpation. No discharge was evident. Pain and burning sensation were present on palpation [Table/Fig-1]. Haematological parameters were within normal limits. HIV was non reactive and random blood glucose was 120 mg/dl.
Clinical picture of the red lesion over the dorsal, lateral and ventral surface of the tongue.
A smear was taken and sent for cytological examination which revealed sheets of RBCs along with mixed inflammatory cells.” X-ray chest PA view was taken to rule out any granulomatous disease like tuberculosis or sarcoidosis and it had shown no abnormal findings. An Incisional biopsy of the tongue was done under local anaesthesia, which showed stratified squamous epithelium with top to basilar dysplastic changes. The underlying connective tissue showed intense chronic inflammatory infiltrate which was suggestive of “carcinoma in situ.”
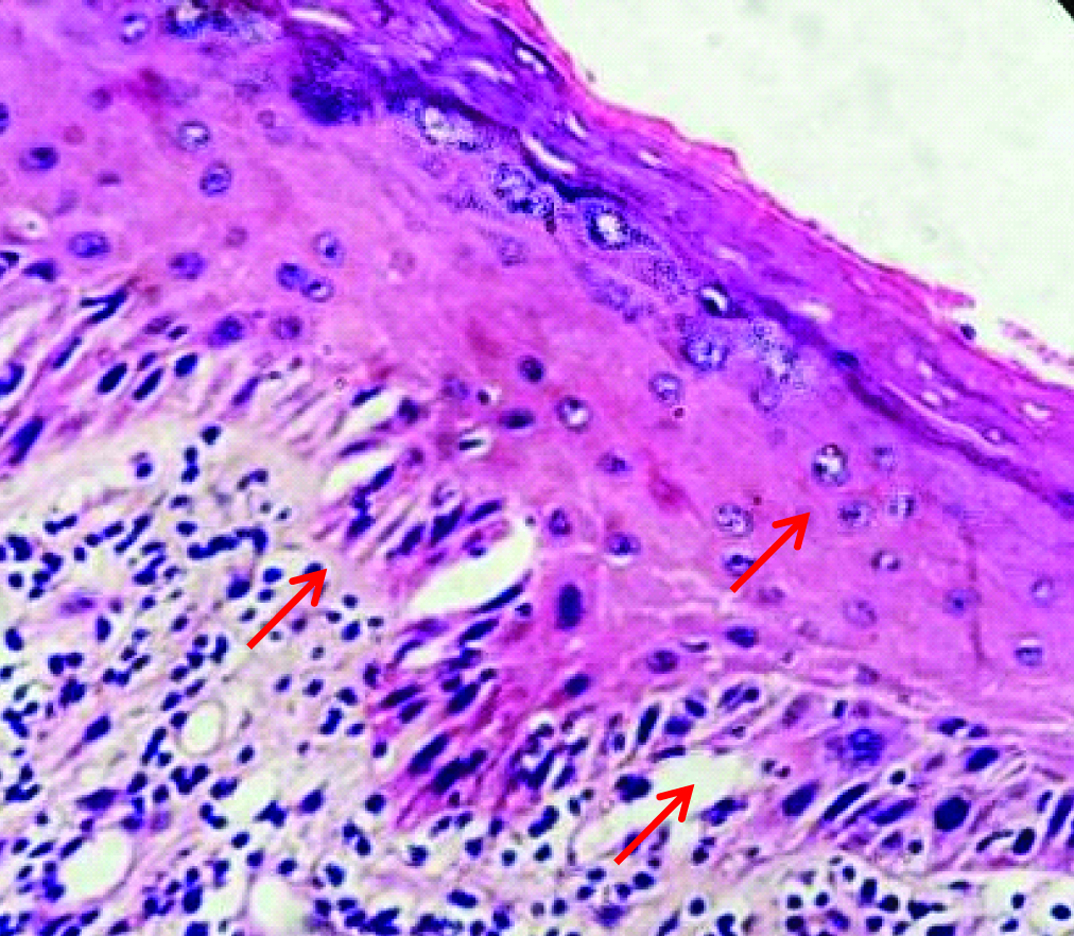
A wide local excision was done which on histopathology examination showed ulcerated tissue infiltrated by sheets of chronic inflammatory cells and lymphoid follicles, at places lined by squamous epithelium exhibiting moderate to severe dysplasia. The inferior margin showed moderate dysplasia of lining squamous epithelium and posterior margin showed mild dysplasia of lining squamous epithelium which suggested a final diagnosis of erythroplakia of tongue with severe dysplasia [Table/Fig-2]. Since the complete lesion was excised patient was not given any medication. He was kept on a review for two years every three months and he reported with no signs of recurrence with healed tissue evident [Table/Fig-3].
H&E stain 40x view of squamous epithelium exhibiting moderate to severe dysplasia.
Three month follow up intraoral photograph post excision.

Discussion
Red lesions occurring on the tongue may be associated with developmental deformities, inflammation, vasodilatation, injuries, infection, allergies, extravasation of blood, erosion of the mucosa, premalignancies and malignancies, radiation and idiopathic causes. Most lesions occurring on the tongue heal fast owing to the rich blood supply and if a lesion does not heal within 10-14 days, it must be biopsied for further evaluation and diagnosis [1-3]. Erythroplakia is known as a specific disease entity which needs a differentiation from other specific or nonspecific inflammatory lesions, which can only be done in most cases by biopsy [4]. In the present case a clinical differential diagnosis of erythroplakia, erosive oral lichen planus, erythematous candidiasis, oral pemphigus, and ulcerative granuloma secondary to eosinophilia, carcinoma of the tongue, sarcoidosis and oral lesion secondary to Crohn’s disease were considered.
Erythematous lesions surrounded by whitened striae are the conventional clinical manifestation of erosive oral lichen planus which is a chronic autoimmune disease that affects the skin, genital mucosa, the oral mucosa, scalp, and nails. Atrophic or erosive lichen planus is clinically significant because burning sensation or pain or both often are present [5].
Erythematous candidiasis is a common opportunistic oral infection. It appears bright red in colour similar to that seen in the present case and may be asymptomatic or associated with a burning sensation and pain. A cytologic smear is useful in confirming the clinical diagnosis [5].
Lesions of pemphigus vulgaris which is a chronic mucocutaneous disease manifest initially in the oral cavity and then spread to the mucous membranes and skin [6]. Oral lesions typically depict a chronic course, causing blisters, erosions, and ulcers. The prevalence of oral involvement sometimes varies. One recent study showed that Bulgarian patients had lesser frequency of oral lesions (66%) when compared to Italian (83%) and Israeli (92%) patients [7]. Erosions and ulcers are the main features of oral pemphigus which initially occur as vesiculobullous lesions which rupture and ulcerate. Ulcers heal slowly, but scarring is rare [8]. Pemphigus rarely remains localized during its clinical course [9]. The predicament of why the disease is localized in some patients and involves multiple sites in some is an issue of interest and concern [10].
Ulcerative granuloma secondary to eosinophilia is a rare self-limited oral condition mostly occurring in the sixth and seventh decades of life that manifests as a solitary ulceration varying in size from few millimeters to several centimeters, with elevated and indurated borders and with peripheral erythema, a white or yellowish base and fibrinous membrane affecting mostly the tongue, buccal mucosa or lip. Pain may hinder food intake. It may regress spontaneously in less than a month with or without recurrence and may sometimes be associated with enlarged regional lymph nodes [11].
Carcinoma of the tongue, oral squamous cell carcinoma usually takes varied clinical forms. It may resemble a leukoplakia, a verrucous leukoplakia, an erythroleukoplakia, or an erythroplakia, and may develop into a necrotic looking ulcer with irregular, raised indurated borders, or into a broad based exophytic mass with a surface texture which may be verrucous, pebbled or smooth. When traumatized, oral squamous cell carcinoma bleeds readily and often becomes superficially secondarily infected. Pain may or may not be present unless secondarily infected. Large lesions may interfere with normal speech, mastication or swallowing [12].
Sarcoidosis is a disorder which involves multiple systems and most commonly affects young adults. It may be acute or insidious in onset where acute onset cases show a spontaneous resolution and progressive fibrosis may occur in cases with insidious onset. The diagnosis is confirmed by clinicoradiographic findings of hilar lymphadenopathy, pulmonary infiltration, ocular and skin lesions and histological evidence of epithelioid granuomas in more than one system [13].
Crohn’s Disease (CD) is an autoimmune disorder of the Gastrointestinal (GI) tract with oral involvement identified in upto 80% of patients which may precede GI involvement in some cases. Oral lesions present as persistent lip swelling, cobble stoning of the oral mucosa, mucogingivitis, deep linear or serpiginous ulcerations which may be associated with pain, impairment of oral function, and psychosocial stress [14].
Erythroplakia clinically appears as a solitary, flat or depressed lesion with a smooth or granular surface and is most commonly caused by the use of tobacco and alcohol [15]. It is prevalent in middle aged and elderly males and varies between 0.02% and 0.83% varying in size from 1 cm to larger than 4 cm in size [16]. It was first described by Queyrat in 1911 as occurring on the glans penis and representing a premalignant process [4]. Erythroplakia is defined as ‘‘a fiery red patch that cannot be characterized clinically or pathologically as any other definable disease”. Tobacco and alcohol are commonly considered important aetiologic factors. The possible role of C. albicans may be present. Shear described erythroplakia as three variants: 1) Homogeneous erythroplakia – lesion that appeared flat, velvety, with uniformly red appearance; 2) Granular erythroplakia – red lesions with granular surface; 3) Speckled erythroplakia/ erythroleukoplakia – predominantly red lesion speckled with white spots. Histopathologically, it usually shows some degree of dysplasia and in some cases carcinoma in situ or invasive carcinoma. Early detection and immediate surgical excision are recommended due to its high malignant transformation rate of 90% [15].
It was described that a high prevalence of p53 mutations may be present in premalignant oral erythroplakia though, the causes for this lesion are unknown, a few authors have presumed it to have similar causes as that of oral squamous cell carcinoma. The tissue microscopically may exhibit severe epithelial dysplasia or carcinoma in situ or invasive cell carcinoma. The high malignant transformation rate owes to early effective treatment being mandatory. Surgery, either by cold knife or by laser, is the recommended therapy. Surgical excision may be used in lesions with severe epithelial dysplasia or carcinoma in situ [16].
Conclusion
Widespread red lesions in the oral cavity are left undiagnosed unless they turn symptomatic due to lack of public awareness and knowledge. Any red lesion in the oral cavity should be evaluated with a proper history from the patient. In the present case report, the history was taken in detail and a variety of lesions were analysed for clinical symptoms as differential diagnosis, since there was no particular known aetiology. Since erythroplakia is diagnosed mainly based on clinical and histopathological exclusion of other lesions or disease, this wide spread lesion was diagnosed as erythroplakia. Thus, a proper history and a varied differential diagnosis are extremely important in diagnosis and management of any red lesion of oral cavity.
[1]. Sunil A, Kurien J, Mukunda A, Deepthi BA, Common superficial tongue lesionsIndian Journal of Clinical Practice 2013 23(9):534-42. [Google Scholar]
[2]. Venkataraman BK, Diagnostic Oral Medicine 2013 1st ed [Google Scholar]
[3]. Mangold AR, Torgerson RR, Rogers RS, Diseases of the tongueClinics in Dermatology 2016 34(4):458-69. [Google Scholar]
[4]. Shafer WG, Waldron CA, Erythroplakia of the oral cavityCancer 1975 36(3):1021-28. [Google Scholar]
[5]. Flores IL, Santos-Silva AR, Coletta RD, Vargas PA, Lopes MA, Widespread red oral lesionsThe Journal of the American Dental Association 2013 144(11):1257-60. [Google Scholar]
[6]. Dagistan S, Goregen M, Miloglu O, Çakur B, Oral pemphigus vulgaris: a case report with review of the literatureJournal of Oral Science 2008 50(3):359-62. [Google Scholar]
[7]. Brenner S, Tur E, Shapiro J, Ruocco V, D’avino M, Ruocco E, Pemphigus vulgaris: environmental factors. Occupational, behavioral, medical, and qualitative food frequency questionnaireInternational Journal of Dermatology 2001 40(9):562-69. [Google Scholar]
[8]. Scully C, Challacombe SJ, Pemphigus vulgaris: update on etiopathogenesis, oral manifestations, and managementCritical Reviews in Oral Biology & Medicine 2002 13(5):397-408. [Google Scholar]
[9]. Zaraa I, El Euch D, Kort R, Sellami M, Mokni M, Makni S, Localized pemphigus: a report of three casesInternational Journal of Dermatology 2010 49(6):715-16. [Google Scholar]
[10]. Nguyen T, Ahmed AR, Pemphigus vulgaris localized to the tongueJournal of Dermatological Case Reports 2014 8(2):55 [Google Scholar]
[11]. Doyle JL, Geary W, Baden E, Eosinophilic ulcerJournal of Oral and Maxillofacial Surgery 1989 47(4):349-52. [Google Scholar]
[12]. Feller L, Lemmer J, Oral squamous cell carcinoma: epidemiology, clinical presentation and treatmentJ Cancer Ther 2012 3:263-68. [Google Scholar]
[13]. James DG, A clinicopathological classification of granulomatous disordersPostgraduate Medical Journal 2000 76(898):457-65. [Google Scholar]
[14]. Woo VL, Oral manifestations of crohn’s disease: a case report and review of the literatureCase Reports in Dentistry 2015 2015:830472 [Google Scholar]
[15]. Grover CM, Malik NS, Kumar A, Parshuram V, Potentially malignant disorders-an updateJournal of Advanced Medical and Dental Sciences Research 2014 2(3):56-61. [Google Scholar]
[16]. Yardimci G, Kutlubay Z, Engin B, Tuzun Y, Precancerous lesions of oral mucosaWorld Journal of Clinical Cases: WJCC 2014 2(12):866 [Google Scholar]