Tufted Angioma of Eyelid in an Adult - A Case Report
Jyoti Verma1, Anshul Singh2, Vatsala Misra3, S. P. Singh4
1 Junior Resident, Department of Pathology, M.L.N Medical College, Allahabad, Uttar Pradesh, India.
2 Assistant Professor, Department of Pathology, M.L.N Medical College, Allahabad, Uttar Pradesh, India.
3 Professor and Head, Department of Pathology, M.L.N Medical College, Allahabad, Uttar Pradesh, India.
4 Director and Professor, Department of Ophthalmology, Regional Institute of Ophthalmology, M.L.N. Medical College, Allahabad, U.P., India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyoti Verma, Moti Lal Nehru, Medical College, Allahabad, Uttar Pradesh-211001, India.
E-mail: jyoti.gsvm@gmail.com
Tufted Angiomas also known as angioblastomas /Angioblastoma of Nagakawa are rare vascular neoplasms localised to the skin and subcutaneous tissues with the upper trunk and neck being most common sites. They are mainly seen in children but a few cases in juveniles and adults have been reported. We hereby report this case, a 40-year-old male who presented with a right lower lid, painless, slowly progressive, firm swelling diagnosed as Tufted Angioma on histopathology and immunohistochemistry.
Angioblastoma, Immunohistochemistry, Vascular neoplasm
Case Report
A 40-year-old male presented with a right lower lid painless, gradually progressive swelling for the past 2 years. There was no preceding history of trauma, cutaneous lesion, infection or any drug intake. No physical or systemic abnormality was noted. Patient had normal haemogram, coagulation profile and immune status. Lesion was excised and submitted for histopathological examination.
Biopsy specimen received was a single, irregular, firm, reddish brown piece of tissue measuring 0.5x0.5cm in size and was processed as such.
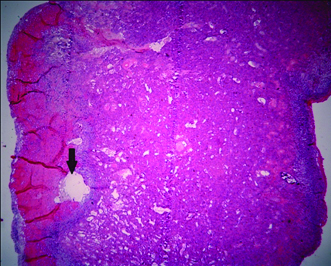
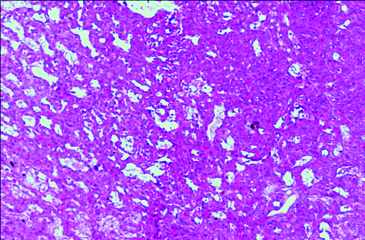
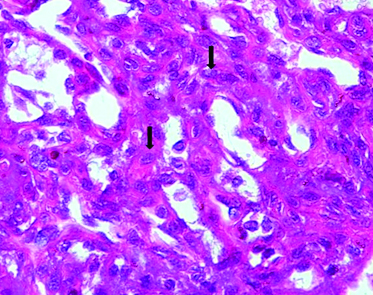
The haematoxylin and eosin – stained sections [Table/Fig-1,2 and 3] were examined and showed fragments of stromal tissue of eyelid with relatively circumscribed ovoid foci of closely packed capillaries scattered throughout the stroma with surrounding pericytic proliferation. Capillaries were bloodless and were lined by plump endothelial cells. Dilated lymphatic like vessels were seen in close approximation to capillary aggregates. No well-defined epithelial lining was seen. No significant mitotic figures were identified.
Lobular aggregates of capillaries with peripheral dilated lymphatics (arrow) in Tufted Angioma. (H&E x4).
Closely packed proliferating capillaries with Pericytic proliferation. (H&E x200).
Pericyte (arrow) proliferation surrounding capillaries lined by plump endothelial cells. (H&E x400).
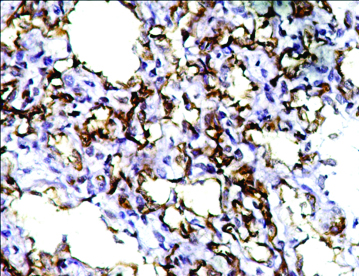
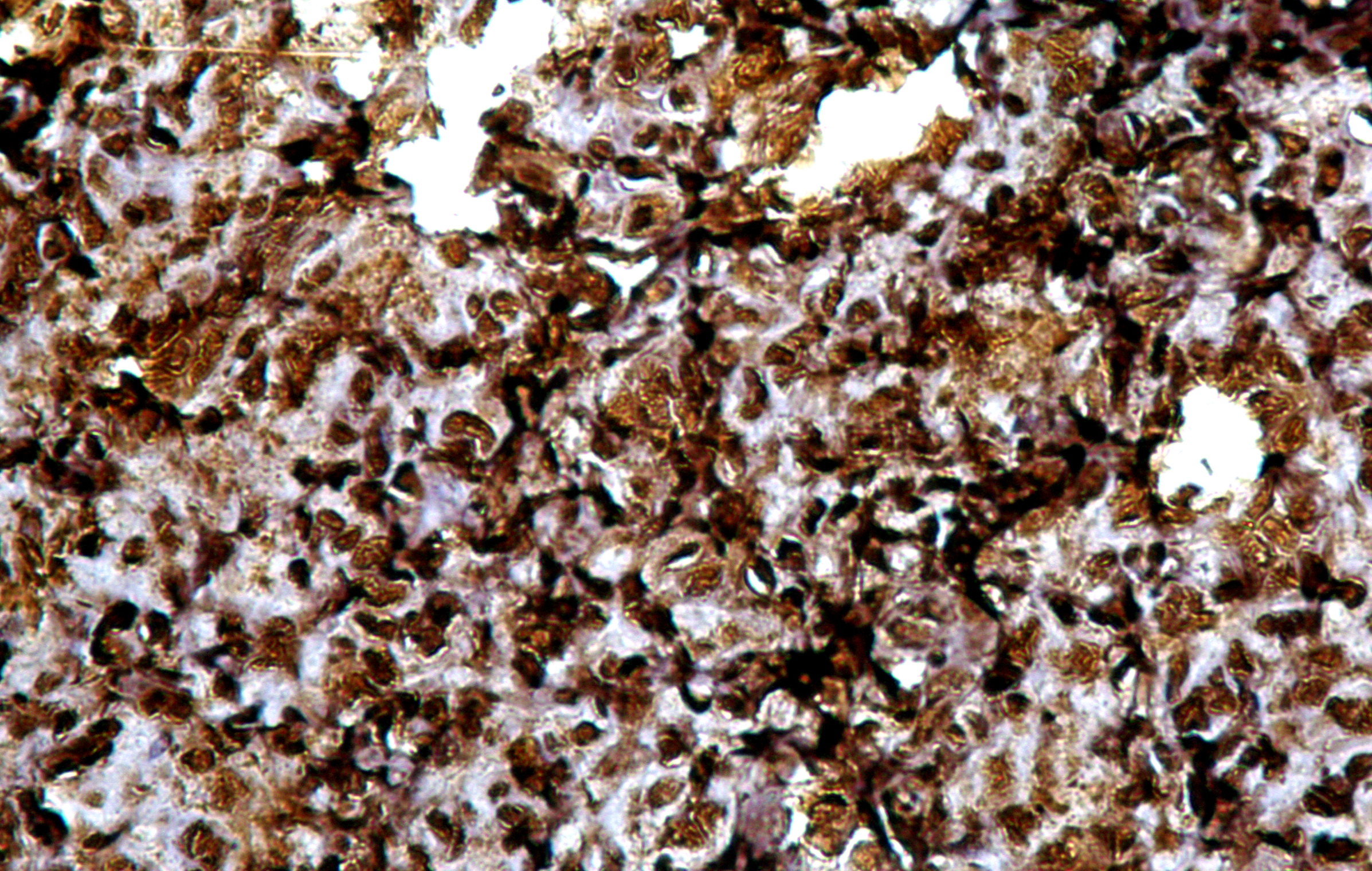
On immunohistochemistry, the endothelial cells lining the capillaries were positive for CD 34 [Table/Fig-4] and the pericytic cells showed diffuse strong positivity for SMA [Table/Fig-5].
Endothelial cells lining capillaries showing CD34 positivity. (IHC x400).
Pericytic cells showing diffuse strong positivity for SMA. (IHC x400).
Hence the final diagnosis of tufted angioma was established on the basis of clinical presentation, histopathological examination and immunohistochemistry. Post biopsy performance of the patient could not be assessed as he didn’t turn up.
Discussion
Tufted Angioma (TA) is a rare, slowly progressive benign vascular tumour with variable clinical presentation. Most cases (60-70%) of TA develop before the age of five years and fewer than 10% of cases with TA occur after the age of 50 years. There is no sex predilection [1]. TA usually presents as a solitary nodule, papule or plaque predominantly over neck, upper thorax and shoulders [2] with face, scalp and proximal extremities being rare sites of involvement. TA may even be multifocal. The lesion progresses slowly over months to years and size of the lesion can be variable [3]. TA is usually asymptomatic but may be found associated with tenderness, hyperhidrosis and hypertrichosis [1,4,5]. Occasionally, TA may be associated with the Kasabach-Merritt syndrome (KMS) [2]. If patient presents with ecchymotic patches or petechiae, clinician should be alert as it may have developed into KMS.
TA are discrete, round to ovoid shaped, vascular tufts of densely packed but poorly canalized capillaries. These capillaries are usually lined by round to oval and sometimes spindled, plump endothelial cells which are randomly dispersed in the dermis in a “cannonball distribution” [6]. Occasionally they may be seen extending into the subcutaneous tissue. Predominant component of TA is formed by the pericytes which surround these capillaries. These pericytic cells are bland looking, have oval to slightly elongated nuclei with scant cytoplasm and indistinct cell boundaries. On IHC, the endothelial cells are reactive for numerous markers including CD31, CD34 and von Willebrand factor (factor VIII) [7]. These angiomatous lobules are surrounded by dilated, crescent shaped lymphatic spaces. The epidermis and cutaneous appendageal structures of the dermis are usually uninvolved. Oedema and inflammation is absent.
TA needs to be differentiated from various other non-neoplastic as well as neoplastic vascular lesions like capillary haemangioma, Kaposiform haemangioendothelioma, Kaposi’s sarcoma and low grade angiosarcoma depending on the age [1,6,8–10] [Table/Fig-6,7].
D/D of tufted angioma in children.
| Features | Tufted Angioma | Kaposiform Haemangioen Dothelioma | Capillary Haemangioma |
|---|
| Microscopy | Cannon ball nests, lobular aggregates of spindle and polygonal cells with interspersed endothelial cell lining capillaries.Pericyte rich epithelioid nodules(-) | Cannon ball nests with glomeruloid structures (+) with prominent lymphatic network surrounding tumour lobules.Pericyte rich epithelioid nodules (+) | Cannon ball nests and glomeruloid structures (-) |
| IHC | (+) | Well formed capillaries (+)Neoplastic spindle cells focally (+)Slit like vessels (vWF -ve) | (+) |
| CD34, CD31, vWF |
| SMA | Pericytes diffusely (+) | Pericytes focally (+) | NA |
| D2 40 | Cannon ball like capillaries (-)Surrounding Dilated vessels (+) | Peripheral KS like proliferating capillaries (+)Surrounding dilated vessels(-) | NA |
| GLUT 1 | NA | (-) | (+) |
D/D of tufted angioma in adults.
| Features | Tufted Angioma | Kaposi Sarcoma | Low Grade Angiosarcoma |
|---|
| Endothelial cells | Appear plump to slightly spindled | Spindling is prominent | Cells are atypical and mildly pleomorphic |
| Vascular Spaces | Bloodless | Blood filled | Sinusoid like spaces |
| Nuclear Atypia | Not seen | Present in nodular stage | Mild to moderate |
| Collagen | Absent | NA | Dissected collagen |
| Mitosis, necrosis, haemorrhage | Absent | May be present | Present |
| IHC | CD 34,CD31+ SMA+(pericytes) | Factor VIII positiveHHV 8 positive | CD 34,CD31, factor VIII+ |
Till date, only two cases of TA in eyelid in adults have been reported [7]. Our case was similar to them on all basis except for Ki-67 which showed low proliferation index, and which was not done in our study [7].
Cases with clinical suspicion of TA should undergo a complete haemogram (including platelet count), coagulation profile and full screening for disseminated intravascular coagulation to exclude consumptive coagulopathy and Kasabach- Merritt Syndrome (KMS). Currently, the risk of association of KMS in patients presenting with tufted angioma of eyelid is not very well known. Some studies have reported spontaneous regression of TA, albeit rarely [11,12]. Magnetic Resonance Imaging (MRI) studies have proven useful in the evaluation of the depth of invasion and extent of growth of TA [2].
Conclusion
This case of Tufted angioma gains special consideration due to its unusual site of involvement and age of presentation. Based on this fact, TA needs differentiation from various other vascular lesions of eyelid, especially in adults. Also, it is essential to get a detailed physical and haematological work up done in all cases diagnosed with eyelid TA, to exclude rare association of Portwine stain and Kasabach-Merritt Syndrome.
Abbreviations
TA: Tufted Angioma; KMS: Kasabach-Merritt syndrome; D/D: Differential Diagnosis; KS: Kaposi’s sarcoma.
[1]. Eduardo C, Vascular tumours: tumours and tumour-like conditions of blood vessels and lymphaticsIn Histopathology of skin 2009 10th editionNew DelhiWolters Kluwer:1007-1056.Edited by Elder DE [Google Scholar]
[2]. Goldman MP, Bowes LE. Tufted Angioma. [Last acsessed on 2009 Nov 25.]. Available At: http://emedicine.medscape.com/article/1086612 [Google Scholar]
[3]. Ghosh SK, Bandyopadhyay D, Ghosh A, Biswas SK, Barma KD, Acquired multifocal tufted angiomas in an immunocompetent young adultIndian J Dermatol 2011 56:412-14. [Google Scholar]
[4]. Schaffer JV, Fangman W, Bossenbroek NM, Meehan SA, Kamino H, Tufted angiomaDermatol Online J 2008 14:20 [Google Scholar]
[5]. Cho KH, Kim SH, Park KC, Lee AY, Song KY, Chi JG, Angioblastoma (Nakagawa)–is it the same as tufted angioma?Clin Exp Dermatol 1991 16:110-13. [Google Scholar]
[6]. North PE, Kincannon J, Vascular neoplasms and neoplastic-like proliferations. In: Bolognia JL, Jorizzo JL, Rapini RP, editorsDermatology 2008 2nd edSt. LouisMosby-Elsevier:1771-94. [Google Scholar]
[7]. Mittal R, Tripathy D, Tufted angioma (Angioblastoma) of eyelid in adults-report of two casesDiagnostic Pathology 2013 8:153 [Google Scholar]
[8]. Jones EW, Orkin M, Tufted angioma (angioblastoma): a benign progressive angioma, not to be confused with Kaposi’s sarcoma or low-grade angiosarcomaJ Am Acad Dermatol 1989 20:214-25. [Google Scholar]
[9]. Alberola FT, Betlloch I, Montero LC, Nortes IB, Martínez NL, Paz AM, Congenital tufted angioma: case report and review of the literatureDermatol Online J 2010 16:2 [Google Scholar]
[10]. Hebeda CL, Scheffer E, Starink TM, Tuftedangioma of late onsetHistopathology 1993 23:191-93. [Google Scholar]
[11]. Browning J, Frieden I, Baselga E, Wagner A, Metry D, Congenital, self-regressing tufted angiomaArch Dermatol 2006 142:749-51. [Google Scholar]
[12]. Ishikawa K, Hatano Y, Ichikawa H, Hashimoto H, Fujiwara S, The spontaneous regression of tufted angioma: a case of regression after two recurrences and a review of 27 cases reported in the literatureDermatology 2005 210:346-48. [Google Scholar]