Ameloblastic Carcinoma: A Case Report
Mallika Kishore1, Sunil R Panat2, Ashish Aggarwal3, Nitin Upadhyay4, Nupur Agarwal5
1Post Graduate Student, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, U.P, India.
2Professor & Head, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, U.P, India.
3Senior Lecturer, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, U.P, India.
4Senior Lecturer, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, U.P, India.
5Senior Lecturer, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, U.P, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mallika Kishore, Post Graduate Student, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, U.P, India.
E-mail: dr.mallika.kishore01@gmail.com
Ameloblastic carcinoma is a rare malignant lesion with characteristic histologic features and behavior that dictates more aggressive surgical approach than that of a simple ameloblastoma. Here we present a case of ameloblastic carcinoma of the mandible in a 30-year-old male patient with a clinical course of typical aggressiveness and extensive local destruction.
Metastases, Odontogenic carcinoma, Surgical resection
Case Report
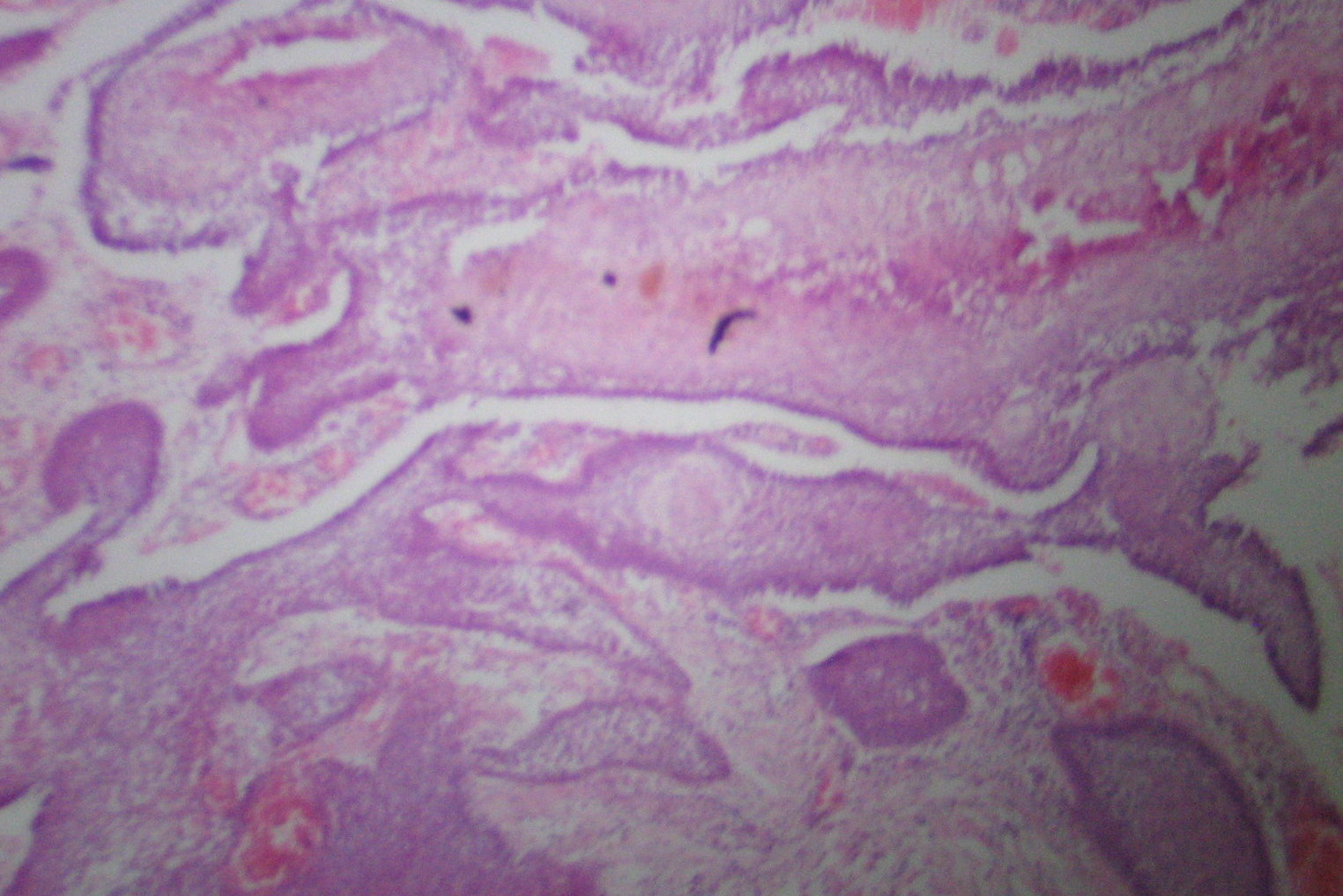
A 30-year-old male patient reported to the Department of Oral medicine and Radiology, Institute of Dental Sciences, Bareilly, UP with a chief complaint of swelling on right lower third of face since six months. On examination a swelling was present over the right angle ramus region of mandible extending from preauricular area to mid of right cheek anteroposteriorly and 1 cm away from corner of the mouth to the base of mandible superoinferiorly. Swelling was approximately 5x3 cm in size and roughly oval in shape. The skin over swelling was normal in colour and texture with a presence of a extraoral draining sinus. On palpation swelling was mildly tender, hard in consistency, smooth, with well-defined margins with local rise in temperature. Intraorally a solitary ill defined swelling was present on the right side of posterior mandibular tooth region extending from mesial surface of mandibular right second premolar to retromolar pad area [Table/Fig-1]. Overlying mucosa was reddish pink in colour, rough in texture. On palpation mildly tender, firm to hard in consistency. On the basis of history and clinical examination provisional diagnosis of ameleoblastoma was given. Differential diagnosis of odontogenic myxoma was considered. Patient was subjected to routine radiographic examination. Mandibular occlusal radiograph showed loss of cortical plate. Orthopantomograph revealed a well defined multilocular radioluscency extending from mesial aspect of right mandibular second premolar to ramus area [Table/Fig-2]. OPG also revealed loss of lower border of mandible with resorption of both mesial and distal roots with respect to right mandibular first molar. Excisional biopsy was done which showed follicles of odontogenic epithelium lined peripherally by tall columnar cells and central stellate reticulum like cells within a scanty connective stroma [Table/Fig-3]. The surface showed parakeratinized stratified squammous epithithelium of gingiva, features suggestive of ameloblastic carcinoma .So, a final diagnosis of ameleoblastic carcinoma was made. In the treatment apron incision was given along with supramyohyoid neck dissection and right side hemimandilectomy was done. Level 1,2 and 3 lymph nodes were removed followed by primary closure.
Discussion
Ameloblastic carcinoma (AC) is an extremely rare odontogenic epithelial malignant tumor, only 70 cases were reported in the English literature between 1984–2011 [1]. The typical ameloblastoma begins as a slowly destructive asymptomatic and intraosseous expansion, being a lesion that tends to expand and infiltrate, rather than perforate the bone are clinical characteristics that contribute to the possible identification of ameloblastomas whereas clinically, ameloblastic carcinomas are more aggressive than most typical ameloblastomas. Perforation of the cortical plate, extension into surrounding soft tissue, numerous recurrent lesions and metastasis, usually to cervical lymph nodes, can be associated with ameloblastic carcinomas [2]. There is a male predominance; the male/female ratio varies according to authors between 1.4/1–2.4:1 [3]. Ameloblastic carcinoma and ameloblastoma can have a similar radiographical appearance; however, certain imaging features may aid the diagnostic distinction [4]. Radiographically both lesions can be radiolucent, either unilocular or multilocular, which generally has a honeycomb appearance with tooth root resorption. Both lesions often have distinct borders, slight marginal sclerosis without periosteal new bone formation, loss of lamina dura, resorption of the tooth apex and tooth displacement except for the presence of focal radiopacity, apparently reflecting dystrophic calcification in ameloblastic carcinoma [1,3,5]. In the recent WHO classification, a distinction was made between ameloblastoma, malignant ameloblastoma and ameloblastic carcinoma [6]. Malignant ameloblastoma differs from ameloblastoma due to the presence of metastases. They both have the same benign histology [7]. Ameloblastic carcinoma has malignant cytologic features regardless of the presence of metastases. In ameloblastoma, metastases are uncommon. When they occur, lungs are involved in over 80% of cases [8]. Surgical resection is the treatment of choice. En bloc removal with 1–2 cm of normal bone margin is the safest surgical modality to ensure disease-free survival. This method has resulted in local recurrence rates of less than 15% [9]. There is controversy regarding radiotherapy of ameloblastoma and it is considered radioresistant tumour[1]. ACs can recur locally 0.5–11 years after definitive therapy. Distant metastasis is usually fatal. The most common site for a distant metastasis is the lung, followed by bone, liver, and brain [10].
Extraoral swelling with pus discharge


Histopathological picture
Conclusion
Ameloblastoma shows a variety of histologic and biologic behavior ranging from benign to frank malignancy. Although AC is rare, it is important to rule it out in patients presenting with toothache or mobile teeth in association with persistent jaw swelling, pain and rapid growth through prompt radiological and histopathologic investigations. Its diagnosis is therefore very important to give proper treatment for better prognosis.
[1]. A Benlyazid, M Lacroix-Triki, R Aziza, A Gomez-Brouchet, M Guichard, J Sarini, Ameloblastic carcinoma of the maxilla: case report and review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 104(6):e17-24. [Google Scholar]
[2]. RL Corio, LI Goldblatt, PA Edwards, KS Hartman, Ameloblastic carcinoma: a clinicopathologic study and assessment of eight cases.Oral Surg Oral Med Oral Pathol. 1987 64(5):570-76. [Google Scholar]
[3]. GT Arotiba, AL Ladeinde, JT Arotiba, SO Ajike, VI Ugboko, OF Ajayi, Ameloblastoma in Nigerian children and adolescents: a review of 79 cases.J Oral Maxillofac Surg 2005 63(6):747-51. [Google Scholar]
[4]. RP Elzay, Primary intraosseous carcinoma of the jaws. Review and update of odontogenic carcinomasOral Surg Oral Med Oral Pathol 1982 54(3):299-303. [Google Scholar]
[5]. V Naik, AD Kale, Ameloblastic carcinoma: a case reportQuintessence Int. 2007 38(10):873-79. [Google Scholar]
[6]. M Amzerin, Z Fadoukhair, R Belbaraka, M Iraqui, S Boutayeb, H M’rabti, T Kebdani, K Hassouni, N Benjaafar, BK El Gueddari, H Errihani, Metastatic ameloblastoma responding to combination chemotherapy: case report and review of the literatureJ Med Case Rep 2011 :5-491.. [Google Scholar]
[7]. LM Ciment, AJ Ciment, Malignant ameloblastoma metastatic to the lungs 29 years after primary resection: a case reportChest. 2002 121(4):1359-61. [Google Scholar]
[8]. JM Henderson, JR Sonnet, C Schlesinger, RA Ord, Pulmonary metastasis of ameloblastoma: case report and review of the literature.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 88(2):170-76. [Google Scholar]
[9]. L Dorner, AJ Sear, Smith GTA case of ameloblastic carcinoma with pulmonary metastases.Br J Oral Maxillofac Surg 1988 26(6):503-10. [Google Scholar]
[10]. R Datta, JS Winston, G Diaz-Reyes, TR Loree, L Myers, MA Kuriakose, NR Rigual, WL JR Hicks, Ameloblastic carcinoma: report of an aggressive case with multiple bony metastasesAm J Otolaryngol 2003 24(1):64-69. [Google Scholar]