Nevus of Ota”- A Rare Pigmentation Disorder with Intraoral Findings
Jitender Solanki1, Sarika Gupta2, Nisha Sharma3, Meenakshi Singh4, Sumit Bhateja5
1 Assistant Professor, Department of Public Health Dentistry, Vyas Dental College & Hospital, Jodhpur, Rajasthan, India.
2 Post Graduate Student, Department of Oral Medicine and Radiology, Vyas Dental College & Hospital, Jodhpur, Rajasthan, India.
3 Senior Lecturer Department of Periodontics, Vyas Dental College & Hospital, Jodhpur, Rajasthan, India.
4 Senior Lecturer Department of Prosthodontics, Jodhpur Dental College & Hospital, Jodhpur, Rajasthan, India.
5 Senior Lecturer Department of Oral Medicine and Radiology, Vyas Dental College & Hospital, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jitender Solanki, Assistant Professor, Department of Public Health Dentistry, Vyas Dental College & Hospital, Jodhpur, Rajasthan, India. Phone : 91-9571580558, E-mail : solankijitender@gmail.com
Nevus of Ota is a dermal melanocytosis seen along the distribution of ophthalmic and maxillary divisions of the trigeminal nerve. Only 12 cases so far have been reported in English literature and it is rare in Indian subcontinent. Most of the cases reported are in females and oral cavity is infrequently involved. Here, we report a rare case of unilateral Nevus of Ota in a 56-year-old male with oral manifestations.
Intra oral pigmentation, Nevi, Oral cavity, Palate, Unliateral
Case Report
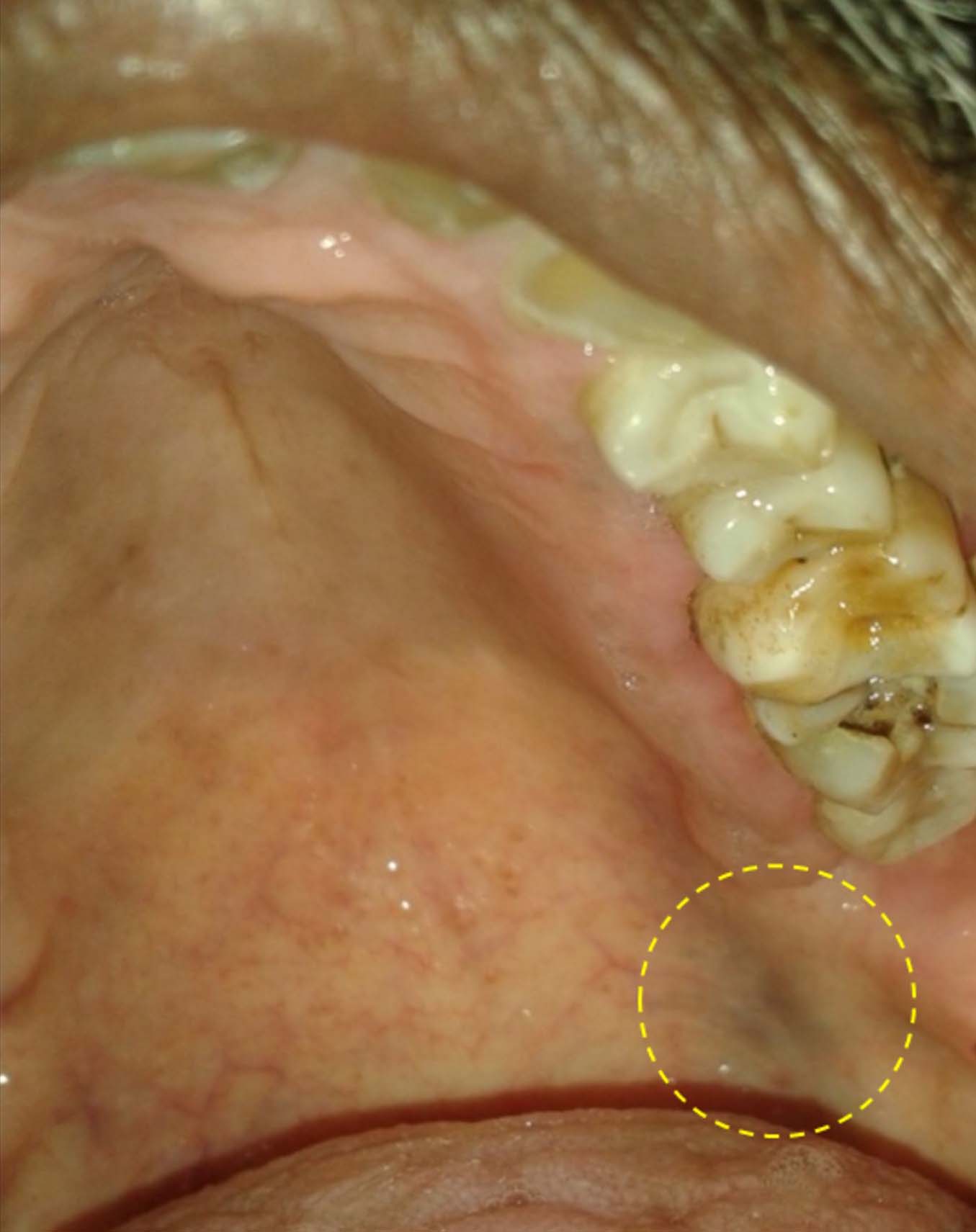
A 56-year-old male visited Department of Oral Medicine & Radiology of Vyas Dental College & Hospital, Jodhpur (India) with a chief complaint of decayed tooth in left lower back tooth region of mouth. There was no significant medical history reported. Extra orally, patient had asymptomatic, speckled, coalescing well-demarcated bluish black hyper pigmented macule on the left mid face involving temporal, frontal, zygoma and the maxillary sinus area [Table/Fig-1]. Bluish pigmentation in sclera of left eye was also observed [Table/Fig-2]. It was present since birth, and family history was noncontributory. Patient also reported that the macules turns dark, deep blue in color in extreme winter and summer seasons. It takes the present color after the weather changes. There was no relevant drug history and no history of photosensitivity. On intraoral examination, blackish discoloration approximately 2 cm in diameter with diffuse margins was evident on the left side of soft palate [Table/Fig-3]. There were also petechiae about two in number present along left retromolar trigone region of mouth. Patient was referred to dermatology for consultation, which did not report any abnormality other than discoloration of face. Auditory examination also did not reveal any discoloration of the auricle and tympanic membrane. A clinical diagnosis of Nevus of Ota was given with the consensus of dermatologist. The patient was not willing for any kind of treatment regarding the pigmentation. Patient was advised to report for regular follow up regarding nevus of ota. The dental treatment plan formulated for the patient was restoration of 36 & thereafter oral prophylaxis since patient had moderate amount of stains and calculus.
Bluish black hyper pigmented macule on the left mid face

Bluish pigmentation in sclera of left eye

Blackish discoloration on the left side of soft palate
Discussion
Nevus of Ota originally described as nevusfuscocaeruleus ophthalmomaxillaris by Ota and Tanino in 1939 is a dermal melanocytosis most commonly found in Japanese [1,2]. Isolated cases of delayed-onset acquired nevi of ota that first appear in adults, including in older patients, have been reported [3]. It is said to be most prevalent in Japan where the incidence among the dermatology outpatients lies between 0.2% to 1%. In Indians it is comparatively rare with the male to female sex ratio being 1:4.8 [4].
Pathophysiology although unconfirmed, yet postulated that Nevus of Ota & other dermal melanocytic disorders such as nevus of ota, blue nevus & mongoloin spots may represent melanocytes that have not migrated completely from neural crest to the epidermis during embryonic stage The two peak ages of onset in early infancy and in early adolescence suggest that hormones are a factor in the development of this condition [5].
After the onset nevus of ota may slowly and progressively enlarge and darken in color. Its appearance usually remains stable once adulthood is reached. The color and perception of nevus of ota may fluctuate depending on personal and environmental factors such as fatigue, menstruation , insomnia, and cloudy cold & hot weather conditions [6].
Nevus of Ota often occurs in association with nevus of Ito which is a dermal melanocytic condition affecting the shoulder area. It can also be associated with other cutaneous disorders and ocular disease. Benign cutaneous and leptomeningeal conditions associated with nevus of Ota are phakomatosis pigmentovasculari, nevus flammeus, Sturge-Weber syndrome, Takayasu disease, Klippel-Trenaunay syndrome, and neurofibromatosis [7].
Mishima classified nevus of Ota into three types depending on the extent and distribution of pigmentation [Table/Fig-4]. Thus our case will correspond to Type III classification, as there was involvement of areas innervated by second and third divisions of trigeminal nerve [8].
Mishima’s classification of nevus of ota
| Subtypes | Intensity | Pigmentation | Area involved |
|---|
| Type I | Mild | Light brown | Upper and lower eyelids and zygomatic area |
| Type II | Moderate | Deep slate Gray | Eyelids, zygomatic area, and base of nose |
| Type III | Intensive | Deep blue to brown | Affecting the first and second divison of trigeminal neuralgia |
Clinical differential diagnosis for skin lesions of nevus of Ota includes mongolian spot, melasma, blue nevus, and drug-induced hyperpigmentation. Mongolian spot tends to spontaneously resolve by age 3–6 years and typically occurs in lumbosacral areas rarely in face. Melasma is bilateral, associated with pregnancy and is seen without palatal involvement [8].
Drug induced hyperpigmentation is usually acquired after ingestion of drugs like minocycline, amiodarone and gold whereas blue nevus may occur anywhere on skin. Sclera and oral mucosa are not involved in acquired bilateral nevus of Ota like macules (ABNOM) or Sun’s nevus [7,8].
Oral melanotic macule can also be misdiagnosed as nevus of Ota. It can also exist in palate but can be distinguished by small in size, and no involvement of sclera. Oral melanotic macule can occur solitary or as a part of syndromes like Peutz-Jeghers syndrome, Leopard syndrome, and Laugier-hanziker syndrome. Our patient, however, had no pigmentation of nail, perioral pigmentation, lentigines, and deafness, thus exclusion of above syndromes was made [8].
There is no definitive diagnosis for nevus of Ota. Skin biopsies are required only if clinical changes are suspected of malignant transformation within the involved skin, ocular tissues or mucosal tissues.
Involvement of palatal mucosa occurs infrequently in nevus of Ota. So far, only 11 cases are reported with intraoral involvement with female predominance (64%). Appearance of palatal pigmentation usually blends with oral mucosa and is seen as irregular, ill defined and often mottled patch. Palatal pigmentation can be differentiated from blue nevus as blue nevus is slightly raised and is usually less than 1 cm in size. Biopsy is generally not indicated.
The ocular complications associated with nevus of Ota are increased intraocular pressure and glaucoma . Melanoma arising in orbit, iris, ciliary body, and optic nerve in association with nevus of Ota has been documented [8]. Periodic reevaluation with ophthalmologist should also be performed annually.
Topical therapy is of no value in the medical treatment. Previous treatment modalities, including cryotherapy, dermabrasion, and microsurgery, can be associated with scarring. Development of the Q-Switched Nd: YAG laser (QSYL) and the Q-switched ruby laser (QSRL) has enabled complete, scarless elimination of the pigmentation in patients [8]. Without treatment, the skin lesions are permanent.
Conclusion
Nevus of Ota with palatal involvement is a rare entity. Dentists should have a thorough knowledge regarding the pigmented lesions as it can indicate varying medical conditions and can lead to future complications if not diagnosed early. Proper follow up and early referral to dermatologist and ophthalmologist is important in diagnosed cases of Nevus of Ota.
[1]. Page DG, Soirsky JA, Kaugars GE, Nevus of Ota within associated palatal involvementOral Surgery Oral Medicine and Oral Pathology 1985 59:282-84. [Google Scholar]
[2]. Mehta V, Balachandran C, Bilateral nevus of OtaJournal of Pakistan Association of Dermatologists 2007 17:59-61. [Google Scholar]
[3]. Singh AP, Bagewadi A, Keluskar V, Shetti A, Nevus of Ota involving palate: case reports and reviewJournal of Indian Academy of Oral Medicine and Radiology 2007 19:441-45. [Google Scholar]
[4]. Chan HH, Kono T, Nevus of Ota: clinical aspects and managementSkinmed 2003 2:89-96. [Google Scholar]
[5]. Hidano A, Kajima H, Ikeda S, Natural history of nevus of otaArch Dermatol 1967 95:187-95. [Google Scholar]
[6]. Hiryama T, Suzuki T, A new classification of ota’s nevus based on histopathological featuresDermatologica 1991 183:167-72. [Google Scholar]
[7]. Hino K, Nagane M, Fujioka Y, Shiokawa Y, Meningeal melanocytoma associated with ipsilateral nevus of Ota presenting as intracerebral hemorrhage: case reportNeurosurgery 2005 56:1376-77. [Google Scholar]
[8]. Sharma G, Nagpal A, Nevus of Ota with Rare Palatal Involvement: A case report with emphasis on differential diagnosisCase Rep Dent 2011 11:670-79. [Google Scholar]