Marchiafava - Bignami Disease: A Case Report
Sunil Kumar K1, Rimiki Challam2, Naveen J3, W. Jatishwor Singh4
1 PG Student, Department of Radiodiagnosis, RIMS, Imphal, India.
2 PG Student, Department of Radiodiagnosis, RIMS, Imphal, India.
3 PG Student, Department of Radiodiagnosis, RIMS, Imphal, India.
4 Professor, Department of Radiodiagnosis, RIMS, Imphal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Kumar K, c/o Department of Radiodiagnosis, RIMS, Imphal, India. Phone : 09774574738, E-mail : drsunilkumark@yahoo.in
Marchiafava-Bignami disease (MBD) is a rare neurological disorder of chronic alcoholism characterized by demyelination and necrosis of corpus callosum. In this case report we present the MR imaging findings of MBD and review of the other imaging features of the disease.
Alchoholism, Corpus callosum, Sandwich sign
Case Report
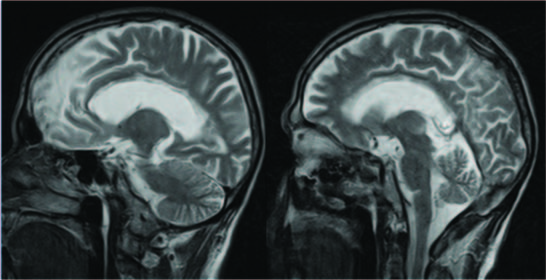
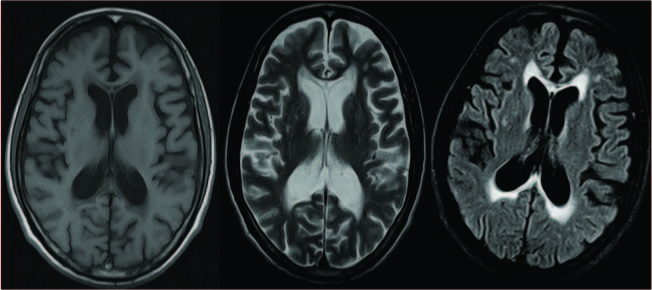
A 55-year-old male patient presented to our institution with complaints of altered sensorium followed by loss of consciousness since one day. He had a history of chronic alcohol intake for about 25 years. He used to take around 750 ml of country made alcohol daily. There was no history of fever, headache, vomiting, seizure or hypertension. On clinical examination patient was found to be malnourished and in altered sensorium (E2V2M3). Signs of meningeal irritation including neck rigidity and kernig sign were absent. Pupils were of normal size and normal reacting. Motor examination showed no neurological deficit. Laboratory results revealed normal haematological profile. Liver function test showed increased serum gamma glutamyl transpeptidase, bilirubin, alkaline phosphatase, and alanine transaminase. MR imaging showed low signal intensity in T1WI & high signal intensity in T2WI in the central portion of genu, body and splenium of corpus callosum with relative sparing of dorsal and ventral layer which give characteristic Sandwich sign [Table/Fig-1,2]. Corresponding region in FLAIR image show hyperintense rim and hypointense core suggestive of gliotic rim with central necrosis [Table/Fig-3]. Other imaging findings included periventricular demyelination & demyelination in left frontal lobe [Table/Fig-2,3]. On the basis of history, clinical features and imaging findings the diagnosis of MBD was made. However, other lesions involving corpus callosum like multiple sclerosis, encephalitis, lymphoma, infarction and astrocytoma were included in the differential diagnosis. History of chronic alchoholism with characteristic imaging findings showing central necrosis of corpus callosum strongly favours the diagnosis of MBD in this case.
Sagittal T1WI show low signal in the central layers of the genu, body & splenium of the corpus callosum
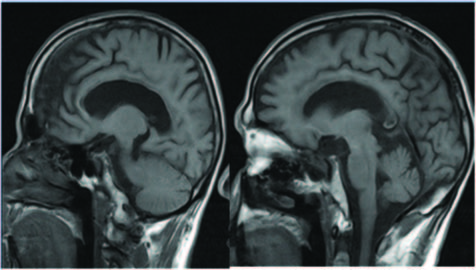
Sagittal T2WI show low signal in the central layers of the genu, body & splenium of the corpus callosum with sparing of the dorsal and ventral layers producing the “sandwich sign”
(a) Axial T1WI Show low signal in genu & splenium of carpus callosum;(b) Axial T2 WI show high signal in genu and splenium of carpus callosum; (c)Axial FLAIR image show Hyperintense rim and hypointense core in the genu & splenium suggestive of gliotic rim with central necrosis
Discussion
Marchiafava-Bignami disease (MBD) is a rare neurological complication of chronic alcoholism, with pathognomonic hallmark of corpus callosum demyelination [1]. It was first described by two Italian pathologists, Ettore Machiafava and Amico Bignami [2].
The main pathologic changes seen in MBD include symmetrical demyelination and necrosis of the central part of the corpus callosum, with relative sparing of dorsal and ventral layers. Rarely, other structures of the CNS like optic chiasm and tracts, putamen, anterior commissure, cerebellar peduncles and, cortical gray matter and U fibers may be involved [3,4].
Diagnosis is made on the basis of clinical findings in combination with radiological imaging features [2]. The corpus callosum appears hypoattenuated on CT, with the exception of cases that are characterized by subacute bleeding, in which it may be iso or hyperattenuated. The corpus callosum appears hyperintense on T2-WI, hypointense on T1-weighted images and proton density-weighted MR images during the acute phase. During the subacute phase, cystic lesions and small foci of T2 hypointensity can develop, most likely because of hemosiderin deposition. In chronic stage signal intensity alterations become less evident but residual atrophy of the involved structure is seen [3].
The recent clinical and neuroradiological classification of MBD describes two subtypes. Type A: acute to subacute onset of consciousness impairment, pyramidal tract signs, limb hypertonia, seizures, hyperintense swelling of the corpus callosum on T2-weighted MR sequences and is associated with poor prognosis. Type B: normal or slightly impaired level of consciousness, dysarthria, gait disturbance, signs of interhemispheric disconnection and hyperintense lesions on T2-weighted MR sequences partially involving the corpus callosum. Type B has favourable prognosis and lesions may reverse suggesting an underlying oedema rather than demyelination [5].
FLAIR images show central hypointense signal and peripheral hyperintense rim producing “sandwich sign”, the characteristic diagnostic sign of MBD. Central hypointense signal represents necrosis & hyperintense signal represents gliosis. Uniform hyperintense lesions indicates a combination of demyelination and oedema [6].
In our case the diagnosis was made on the basis of chronic alcoholism and radiological features showing characteristic sandwich sign which are seen as low signal intensity in T1WI, high signal intensity in T2WI & FLAIR images show central low signal intensity with peripheral high signal intensity suggesting central necrosis of corpus callosum with sparing of dorsal and ventral layers. The central necrosis involved genu, body and splenium of corpus callosum.
Lesions show high signal intensity on DWI with reduced or increased apparent diffusion coefficient (ADC) values depending on the progression of the disease. In early stage, cytotoxic oedema may be the underlying mechanism where the lesions are seen as hyperintense on DWI with reduced ADC. In the later stages, increased ADC may be due to the pure demyelination without axonal injury [7].
Other imaging modalities include MR spectroscopy (MRS) which shows increase in choline, increased choline/creatine (Cho/ Cr) ratio in acute phase. Lactate peak is usually seen in the acute/subacute phase of demyelination. SPECT studies shows bilateral reduction in cerebral blood flow [8].
Differential diagnosis includes infarction of recurrent artery of Heubner, neoplastic disease such as astrocytoma or lymphoma, demyelinating disease such as multiple sclerosis (MS), progressive multifocal leukoencephalopathy, or acute disseminated encephalomyelitis. MS is by far the most common and needs to be ruled out. Compared to MS, MBD has symmetric and oedematous spots restricted in corpus callosum on brain CT scans or MRI [9].
Marchiafava-Bignami disease may present in various clinical forms. Acute Marchiafava-Bignami disease may present with seizures, impairment of consciousness, and rapid death. Subacute Marchiafava-Bignami disease present with variable degrees of mental confusion, dysarthria, behavioral abnormalities, memory deficits and impairment of gait. Chronic Marchiafava-Bignami disease, is characterized by mild dementia which is progressive over years [10].
Treatment of MBD is usually empirical and consists of multivitamins, corticosteroids, stabilization of plasma glucose, and supportive care. Early diagnosis and prompt appropriate management are critical in reversing the underlying pathophysiology in the early stage [1].
Conclusion
Marchiafava-Bignami disease is a complication of chronic alcoholism with various clinical manifestations which is often misdiagnosed and mistreated. But recent advance in neuroimaging has made early diagnosis of MBD possible & helps in early initiation of treatment. Recognition of the imaging features of MBD is essential for radiologist for proper diagnosis.
[1]. Yadala S, Luo JJ, Marchiafava-Bignami Disease in a Nonalcoholic Diabetic PatientCase Reports in Neurological Medicine 2013 2013:979383 [Google Scholar]
[2]. Seneviratnea K, Alten S, Farrugiaa M, A Rare Case of Chronic Alcoholism Related Marchiafava-Bignami DiseaseJ Neurol Res 2011 1(4):168-69. [Google Scholar]
[3]. Gambini A, Falini A, Moiola L, Comi G, Scotti G, Marchiafava-Bignami Disease: Longitudinal MR Imaging and MR Spectroscopy StudyAm J Neuroradiol 2003 24:249-53. [Google Scholar]
[4]. Johkura K, Naito M, Naka T, Cortical Involvement in Marchiafava-Bignami DiseaseAm J Neuroradiol 2005 26:670-73. [Google Scholar]
[5]. Caulo M, Briganti C, Notturno F, Committeri G, Mattei PA, Tartaro A, Non-Alcoholic Partially Reversible Marchiafava-Bignami Disease: Review and Relation with Reversible Splenial LesionsThe Neuroradiology Journal 2009 22:53-8. [Google Scholar]
[6]. Bano S, Mehra S, Yadav SN, Chaudhary V, Marchiafava-Bignami disease: Role of neuroimaging in the diagnosis and management of acute diseaseNeurology India 2009 57(5):649-51. [Google Scholar]
[7]. Bilgic B, Bilgin Arslan A, Buluth H, Bayram A, Gokben Hizli F, A Marchiafava-Bignami Patient with Mild Symptoms and the Role of Diffusion-Weighted Magnetic Resonance Imaging in the DiagnosisArchives of Neuropsychiatry 2011 48:277-80. [Google Scholar]
[8]. Rudkin TM, Arnold DL, Proton magnetic resonance spectroscopy for the diagnosis and management of cerebral disordersArch neurol 1999 56:919-26. [Google Scholar]
[9]. Chang N, Kar-Wai E, Jung S, Liao C, A Rare Case of Marchiafava-Bignami Disease in TaiwanJ Radiol 2010 35:185-90. [Google Scholar]
[10]. Raina S, Mahesh DM, Mahajan J, Kaushal SS, Gupta D, Dhiman DS, Marchiafava-Bignami DiseaseJAPI 2008 56:633-35. [Google Scholar]