Prophylactic use of antibiotics in surgery was introduced first in 1957 by Miles and in 1961 by Burke [1]. It is currently an essential component of the standard of care in virtually all surgical procedures and has resulted in reduced post-operative infections [2]. Antimicrobial prophylaxis is essential to eradicate or retard the growth of endogenous microorganisms [1].
Antibiotic prophylaxis in elective surgeries is essential to prevent Surgical Site Infection (SSI), chest infection and urinary tract infections. SSI is second only to urinary tract infection as the most common nosocomial infection in hospitalized patients. It has been estimated that SSI develops in at least 2% of hospitalized patients undergoing operative procedures. The mortality rate was 3% among patients who developed SSI [3].
The basic principle of antimicrobial prophylaxis in surgery is to achieve adequate serum and tissue drug levels that exceed, for the duration of the operation, the MICs for the organisms that are likely to be encountered during the operation [4].
The antimicrobial selection is based on cost, antibacterial activity, adverse-effect profile, ease of administration and pharmacokinetic profile. In the present study we made an effort to evaluate and compare the extent of rationality in administering antimicrobial prophylaxis on elective surgeries across three hospitals.
MATERIALS AND METHODS
This was a prospective, comparative, observational study approved by the Institutional Ethics Committee. The study was conducted at three hospitals in Mangalore city.
Wenlock District Government Hospital (Group I)
Kasturba Medical College teaching hospital (Group II)
Kasturba Medical College corporate hospital (Group III)
The study was conducted between April 2011 and March 2012.One hundred and fifty cases satisfying the inclusion and exclusion criteria were randomly selected from each hospital. Patients between 15- 80 years undergoing elective clean or clean- contaminated surgery without any local or generalized infection before surgery were included in the study. Patients with uncontrolled diabetes mellitus, immunodeficiency disorder, hepatic or renal disorders were excluded from the study.
The study was conducted on a real-time basis. Each patient was followed up till he/she was discharged from the hospital. The investigator did not intervene in the patient’s care in any way. The following details were collected using a pre-designed proforma from the case sheets of the patients, personal interview of the patient and consultation of the concerned surgeon, duty doctor, and staff nurse if necessary.
Age & sex of the patient
Surgical procedure conducted
Duration of stay in the hospital
Total number of antimicrobials used per group
Average number of antimicrobials used
Various antimicrobial agents used
Route of administration
Dosage
Timing of pre-operative dosing
Duration of prophylaxis
Assessment of appropriateness of antibiotic prophylaxis was done based on the following guidelines:
Scottish Intercollegiate Guidelines Network’ that was composed by National Health System Quality Improvement Scotland (NHS QIS) in 2008 [5].
The ASHP Therapeutic Guidelines on Antimicrobial Prophylaxis in Surgery that was drafted by Rocky Mountain Poison and Drug Center and American Society of Health System Pharmacists (ASHP) [6].
Appropriateness of antimicrobial prophylaxis was graded based on modified categories of judgment, as proposed by Kunin and co-workers [1].
STATISTICAL ANALYSIS
Data were entered and analyzed with Statistical Package for Social Service (SPSS) version 11.0. Rates of baseline clinical characteristics are reported as means with Standard Deviation (SD) or percentages. For discrete variables, chi square test was used. Comparison of continuous variables was performed with one way ANOVA (Analysis of Variance) followed by Scheffe’s post hoc analysis. Significance levels were set at p<0.05.
RESULTS
Demographic details of the patients are shown in [Table/Fig-1]. Cephalosporins were the most commonly used group of antimicrobials in all the three groups. The use of fluoroquinolones was relatively higher in group III (10.3%) followed by group II (8.9%) and group I (7.1%). The use of aminoglycosides was higher in group I (9.2%) & group III (8.1%) as compared to group II (3.2%).
Demographic details of the patients
| Demographic Data | Group I | Group II | Group III |
|---|
| Age in years (Mean±SD) | 39.49±16.77 | 42.65±14.94 | 44.97±17.061 |
| Sex (%) | Male | 111(74.0%) | 103(68.7%) | 96(64.0%) |
| Female | 39(26.0%) | 47(31.5%) | 54(36.0%) |
Twenty two percent of cases in group I, 64.9% cases in group II and 80.7% of cases in group III received pre-operative prophylaxis as per the guideline [6] that is, a single dose of antimicrobial agent half an hour before surgery.
DISCUSSION
Clinical trials have shown that antimicrobial prophylaxis can lower the incidence of infection after surgeries [7]. An effective prophylactic regimen should be directed against the most likely infecting organisms. Infections can be prevented when an effective concentration of the drug is present in the blood and the tissue during and shortly after the procedure. Therefore antibiotic prophylaxis should begin just before surgery [7]. A single dose prophylaxis before surgery has been found to be sufficient. Post-operative administration of more than single dose in clean and clean-contaminated surgeries is unnecessary and leads to development of resistant strains [8].
A total of 450 cases were selected in equal proportion from three hospitals, catering services to three different socioeconomic strata of population in and around Mangalore. The first was a government hospital, the second was a medical college teaching hospital and the third was a corporate tertiary care hospital.
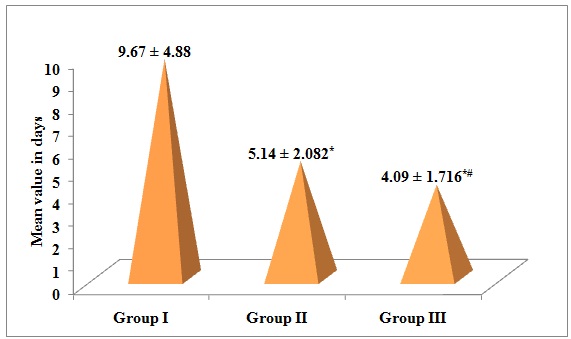
The duration of postoperative stay was found to be highest in the government hospital and least in the corporate hospital [Table/Fig-2] which correlates with the findings of a previous study conducted in Jordan. The most probable reason could be the differences in the expenses incurred in the hospital stay between the hospitals [9,10]. In the government hospital the stay is much cheaper than in the private sector (Group II & III). There also was a significantly positive correlation between the duration of stay in the hospital and the mean duration of administration of antimicrobial agents [Table/Fig-3–4]. [Table/Fig-5] shows the system wise distribution of procedures conducted.
Duration of stay in hospital
Mean duration of administration of the antimicrobial agent post operatively by intravenous route
| Group | Group I | Group II | Group III |
|---|
| Duration in days (Mean ± SD) | 4.56±2.779 | 2.49±1.47* | 2.14±1.99* |
*p<0.05 compared with group I; †p<0.05 compared with group II
Distribution of subjects based on the duration of antimicrobial agent post operatively by intravenous route
| Duration of administration | Group I | Group II | Group III |
|---|
| 1 day | 17 (11.3%) | 46 (30.7%)* | 55 (36.7%)*† |
| 2 days | 23 (15.3%) | 39 (26.0%)* | 49 (32.7%)*† |
| 3 days | 20 (13.3%) | 34 (22.7%)* | 28 (18.7%)*† |
| > 3 days | 90 (60.0%) | 31 (20.7%)* | 18 (12.0%)*† |
*p<0.05 compared with group I; †p<0.05 compared with group II
System wise distribution of procedures conducted
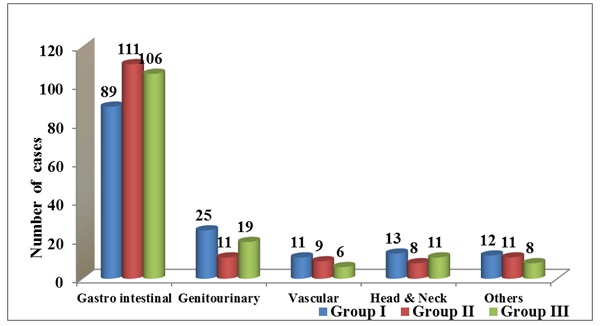
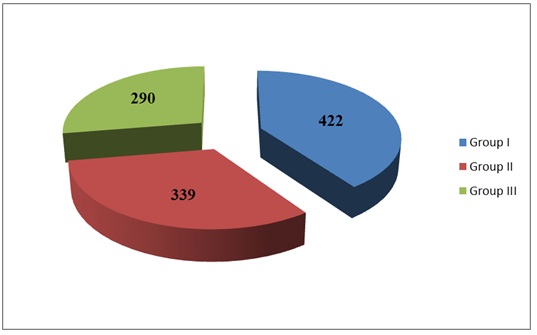
The total number of antimicrobial agents used was highest in government hospital followed by medical college hospital (32.25%) & corporate hospital (27.59%) [Table/Fig-6]. The number of antimicrobial agents used per patient was also significantly higher in government hospital [Table/Fig-7]. These results correlated with the findings of a similar study where the number of antimicrobial agents used was also significantly higher (1.9/patient) in government hospital as compared to private hospital [11] (1.63/ patient). The contributing factors for prescribing more antimicrobial agents in government hospital were prolonged duration of stay both pre & post operatively, thereby increasing the chances of nosocomial infection. The poor hygiene & nutritional status of subjects in government hospital might be the other contributory factors [11]. The cause of increased number of antimicrobials used may also be due to antibiotic anxiety [12] that is, the desire to leave no pathogen uncovered.
Total antimicrobial agents used
Number of antimicrobials per prescription
| Indicators | Group I | Group II | Group III |
|---|
| Number of anti-microbial agents per prescription | 2.81 ± 0.878 | 2.26 ± 0.699* | 1.93 ± 0.787*† |
*p<0.05 compared with group I; †p<0.05 compared with group II
Cephalosporins constituted the most commonly used group of antimicrobials in our study in all the three hospitals constituting 52.6%, 64.95% & 59.81% of total antimicrobial usage respectively [Table/Fig-8]. This correlated with the findings of a similar study where cephalosporins constituted 74.7% of the total antimicrobials used [13].
Categories of Antimicrobial Agents used
| Category of antimicrobial agents used | Group I | Group II | Group III |
|---|
| Penicillins | 24(5.6%) | 21(7.5%) | 31(13.9%) |
| Cephalosporins | 223(52.6%) | 241(64.95%) | 189(59.81%) |
| Nitroimidazoles | 96(22.6%) | 64(22.8%) | 51(16.1%) |
| Fluoroquinolones | 30(7.1%) | 25(8.9%) | 23(10.3%) |
| Aminoglcosides | 39(9.2%) | 9(3.2%) | 18(8.1%) |
| Sulfonamides | 5(1.2%) | 3(1.1%) | 0 |
| Macrolides & Lincosamides | 2(0.5%) | 4(1.4%) | 4(1.8%) |
| Anti-parasitic | 5(1.2%) | 4(1.4%) | 0 |
| Total | 424 | 371 | 316 |
Administration of single dose of antimicrobial agent half an hour to one hour before surgery was seen in 22%, 64.9% & 80.7% of patients respectively [Table/Fig-9]. In the medical college & corporate hospital the adherence to guidelines in terms of timing of administration was better than the previous study in which only 22% of cases received antimicrobials at the appropriate time [14]. Sixty percent of patients in the government hospital received antimicrobials for more than 24 hours prior to surgery even in the absence of any indications which is unacceptable. The probable reason could be that patients get hospitalized much earlier than the date of surgery in a government hospital & hence antimicrobial administration becomes necessary to prevent nosocomial infections.
Timing of pre-operative dose administration
| Timing of administration | Group I | Group II | Group III |
|---|
| Single dose half an hour before surgery | 33(22.0%) | 96(64.9%) | 121(80.7%) |
| First dose on the previous night & second half an hour before surgery | 25(16.7%) | 8(5.4%) | 3(2.0%) |
| For 1 day prior to surgery in single/divided doses & a dose half an hour before surgery | 71(47.3%) | 36(24.3%) | 25(16.7%) |
| For 2 days prior to surgery in single/divided doses & a dose half an hour before surgery | 17(11.3%) | 7(4.7%) | 1(0.7%) |
| For > 2 days prior to surgery in single/divided doses & a dose half an hour before surgery | 4(2.7%) | 1(0.7%) | 0 |
Mean duration of antimicrobial administration post operatively [Table/Fig-4] was highest in group I followed by group II & least in group III. The duration of administration was significantly higher in all the three groups when compared to previous study results [14]. The administration of prophylactic antimicrobial agent as recommended (not more than one day post operatively) was seen in none of the subjects in any of the three groups. This was in contrast to the previous study results where administration was done for a single day in 36.3% of patients [13]. Administration for 1-3 days was seen in 5 subjects (3.33%) in the government hospital, 28 subjects (18.66%) & 70 subjects (46.66%) in the medical college and corporate hospitals respectively [Table/Fig-10–11]. These results clearly show the wide discrepancies in the duration of administration among different hospitals. Administration of antimicrobials for 7- 10 days was seen in 38.7%, 12.7% & 5.3% of subjects in the three hospitals respectively. Administration for more than 10 days was highest in the government hospital (33.3%) followed by the medical college hospital (3.3%) and the corporate hospital (1.3%). The values of corporate hospital correlated with the previous study results where duration of administration for 7- 10 days was seen in 4.4% &> 10 days was seen in 1.4% of the patients [13].
Mean duration of administration of antimicrobial agents by oral and intravenous route
| Group | Group I | Group II | Group III |
|---|
| Duration in days (Mean ± SD) | 8.14±3.137 | 7.58±2.293* | 6.21±1.93*† |
Mean duration of administration of antimicrobial agents by oral and intravenous route
| Duration of administration | Group I | Group II | Group III |
|---|
| 1 - 3 days | 5(3.3%) | 28(18.7%)* | 70(46.7%)*† |
| 4 - 6 days | 37(24.7%) | 98(65.3%)* | 70(46.7%)*† |
| 7 - 10 days | 58(38.7%) | 19(12.7%)* | 8(5.3%)*† |
| >10 days | 50(33.3%) | 5(3.3%)* | 2(1.3%)*† |
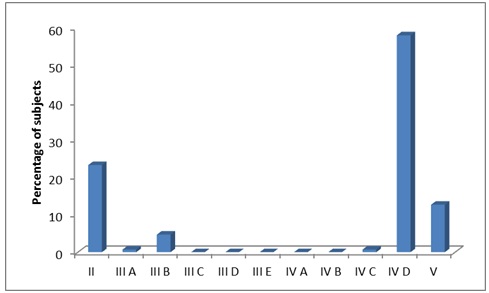
[Table/Fig-12, 13, 14, 15] depict the Kunin’s criteria analysis. None of the subjects in any of the three groups fell into category I that is, “agree with the use of prophylaxis, the program is appropriate (prophylactic use indicated, antibiotic spectrum coverage, timing and duration are appropriate) based on the practice guideline.” This is because none of the subjects in the study received only single dose of antimicrobial agent post operatively as suggested by the SIGN & ASHP guidelines. These findings were in contrast to the previous study findings where 16.3% of cases were classified under category I [13]. In our study 32.9% of subjects were classified under category II in corporate hospital, 23.3% in medical college hospital & [14]. One percent in government hospital that is, “agree with the use of prophylaxis, prophylaxis is probably appropriate, advantages derived remain controversial”. All those cases where antimicrobial agent selection, dose selection & timing of administration were appropriate were included in category II provided there was a substantial reason for the extension of duration of administration beyond 24 hours post operatively. However cases with inappropriate extension beyond 3 days without evidence of associated infection were not included in this category. In most of the cases the reason for extension of prophylaxis was probably the fear of development of SSI as a fresh wound post operatively has a relatively higher chance of developing SSI [1]. This in association with increased chances of developing a urinary tract infection post operatively due to catheterization may be the reason for extension of prophylaxis. Though the advantages derived from extension of prophylaxis in the above cases remains controversial, the use can still be agreed upon considering the local hospital conditions & other local parameters. Only one subject each of medical college and corporate hospital received ineffective antimicrobial regimen. This finding was encouraging as it provided evidence that ineffective antimicrobial agent selection was minimal in all the three groups.
Kunin’s Criteria Analysis
| Kunin’s Criteria | Group I | Group II | Group III |
|---|
| II | 21(14.1%) | 35(23.3%)* | 49(32.9%)*† |
| IIIA | 1(0.7%) | 1(0.7%)* | 0*† |
| III B | 12(8.1%) | 7(4.7%)* | 22(14.8%)*† |
| III C | 1(0.7%) | 0* | 0* |
| III D | 2(1.3%) | 0* | 3(2.0%)*† |
| III E | 4(2.7%) | 0* | 1(0.7%)*† |
| IV A | 1(0.7%) | 0* | 0* |
| IV C | 2(1.3%) | 1(0.7%) | 0* |
| IVD | 75(50.3%) | 87(58.0%)* | 67(45.0%)*† |
| V | 30(20.1%) | 19(12.7%) | 7(4.7%) |
Kunin’s Criteria Analysis
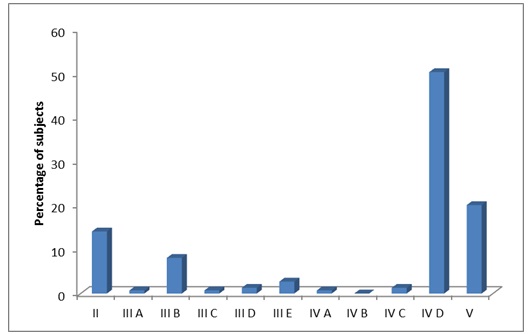
Distribution according to Kunin’s categories in group I
Distribution according to Kunin’s categories in group III
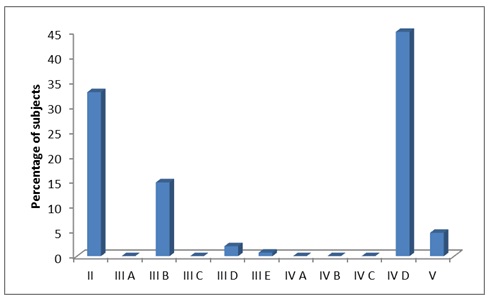
The use of antimicrobial agent that is too toxic when other less toxic alternative antimicrobial is available was seen in 1 subject in government hospital. The use of an antimicrobial agent to which patient is allergic was seen in 2 subjects in the government hospital& 3 subjects in the corporate hospital. The combination of antimicrobial agents chosen was inappropriate in 4 subjects in the government hospital & 1 subject in the corporate hospital.
The use of too expensive and broad-spectrum agents when antimicrobials which are cheaper or more specific against the microbes most likely to cause SSI are available, was seen most commonly in the corporate hospital (14.8%) followed by government hospital (8.1%) & medical college hospital (4.7%). Such values in the corporate hospital were higher than in the previous study where 12.8% subjects had received too expensive or broader spectrum agents [13].
Majority of the subjects in our study fell into category IV D in all the three groups (50.3%, 58%, and 45% respectively). In these subjects the problem was prolonged administration of antimicrobial agent in the absence of any conclusive evidence of infection. These findings in our study were higher in all the groups than one of the previous studies where inappropriate duration was seen in 10.5% of subjects. In another study conducted at St. Luke’s Medical Centre, Philippines, as high as 60.5% of subjects had inappropriate duration of administration [14].
The implementation with regards to regularity of antimicrobial agent administration was erroneous (any combination of III and IV) i.e. both the selection of the regimen & the administration program required modifications in 20.1% (30) subjects, 12.7% (19) subjects and 4.7% (7) subjects respectively in the three hospitals. The findings in the medical college and corporate hospitals were better than the findings of a previous study where 20.9% of cases were included in category V [13].
The Kunin’s criteria analysis gives an overall picture that the antimicrobial prophylactic regimen is relatively better (adherent to guidelines) in the corporate hospitals compared to the other two groups & there is least adherence to guidelines in the government hospital.
Hence antimicrobial use has to be streamlined in India and the way to achieve the goal is to introduce antibiotic guidelines in every hospital.
CONCLUSIONS
The results from this study continue to document the challenges of disseminating evidence-based knowledge systematically into clinical practice. Our study also highlights the fact that there exists a wide difference in the programme of antimicrobial prophylaxis between the three different clinical set ups.
*p<0.05 compared with group I; †p<0.05 compared with group II
*p<0.05 compared with group I; †p<0.05 compared with group II
*p<0.05 compared with group I; †p<0.05 compared with group II